Main Page/SlicerCommunity/2005-2010
Go to 2022 :: 2021 :: 2020 :: 2019 :: 2018 :: 2017 :: 2016 :: 2015 :: 2014-2011 :: 2010-2000
The community that relies on 3D Slicer is large and active: (numbers below updated on December 1st, 2023)
- 1,467,466+ downloads in the last 11 years (269,677 in 2023, 206,541 in 2022)
- over 17.900+ literature search results on Google Scholar
- 2,147+ papers on PubMed citing the Slicer platform paper
- Fedorov A., Beichel R., Kalpathy-Cramer J., Finet J., Fillion-Robin J-C., Pujol S., Bauer C., Jennings D., Fennessy F.M., Sonka M., Buatti J., Aylward S.R., Miller J.V., Pieper S., Kikinis R. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magnetic Resonance Imaging. 2012 Nov;30(9):1323-41. PMID: 22770690. PMCID: PMC3466397.
- 39 events in open source hackathon series continuously running since 2005 with 3260 total participants
- Slicer Forum with +8,138 subscribers has approximately 275 posts every week
The following is a sample of the research performed using 3D Slicer outside of the group that develops it. in 2005-2010
We monitor PubMed and related databases to update these lists, but if you know of other research related to the Slicer community that should be included here please email: marianna (at) bwh.harvard.edu.
Contents
- 1 2010
- 1.1 Application of Vascular Model Toolkit (VMTK) for Coronary Arteries
- 1.2 Ion-Abrasion Scanning Electron Microscopy Reveals Surface-Connected Tubular Conduits in HIV-Infected Macrophages
- 1.3 MRI-Guided Robotic Prostate Biopsy: A Clinical Accuracy Validation
- 1.4 A Method for Planning Safe Trajectories in Image-guided Keyhole Neurosurgery
- 1.5 JHU Workshop for Talented Youth
- 1.6 Canine Hippocampal Formation Composited Into Three-dimensional Structure using MPRAGE
- 1.7 Real-time 3-Dimensional Virtual Reality Navigation System with Open MRI for Breast-Conserving Surgery
- 1.8 Interfaces and Integration of Medical Image Analysis Frameworks: Challenges and Opportunities
- 1.9 Evaluation of Robotic Needle Steering in Ex Vivo Tissue
- 1.10 An Open Source Implementation of Colon CAD in 3D Slicer
- 1.11 In Vivo Visualization of Cranial Nerve Pathways in Humans using Diffusion-Based Tractography
- 1.12 Brain Maturation in Adolescence and Young Adulthood: Regional Age-Related Changesi in Cortical Thickness and White Matter Volume and Microstructure
- 1.13 Coronary Artery Centerline Extraction in 3D Slicer using VMTK based Tools
- 1.14 Assessment of Image Registration Accuracy in Three-dimensional Transrectal Ultrasound Guided Prostate Biopsy
- 1.15 Language Laterality in Autism Spectrum Disorder and Typical Controls: A Functional, Volumetric, and Diffusion Tensor MRI Study
- 1.16 Perk Station-Percutaneous Surgery Training and Performance Measurement Platform
- 2 2009
- 2.1 Three-dimensional Appearance of the Lips Muscles with Three-dimensional Isotropic MRI: In Vivo Study
- 2.2 Traces
- 2.3 CLIMB Study (Comprehensive Longitudinal Investigation of Multiple Sclerosis at Brigham and Women’s Hospital) Former NHS Study (The Harvard Multiple Sclerosis Natural History Study)
- 2.4 Steroid Adjunctive Treatment at Initiation of Avonex Therapy for Patients with Mono-Symptomatic or Relapsing-Remitting Multiple Sclerosis
- 2.5 Age-Related Changes of Cognition in Health and Diseases: Image Analysis Core
- 2.6 Harvard Research Nursing Home Project (MOBILIZE study)
- 2.7 Daclizumab Use in Patients with Pediatric Multiple Sclerosis Failing Interferon
- 2.8 MRI findings of pediatric-onset Multiple Sclerosis patients: a retrospective study
- 2.9 Pediatric MS MRI Pilot Project
- 2.10 The Multiple Sclerosis Database Project
- 2.11 Effects of Strain Thresholds on Bone Formation in Response to Mechanical Loading
- 2.12 Automated Ventricular Systems Segmentation in Brain CT Images by Combining Low-level Segmentation and High-level Template Matching
- 2.13 MRI-derived Measurements of Human Subcortical, Ventricular and Intracranial Brain Volumes: Reliability Effects of Scan Sessions, Acquisition Sequences, Data Analyses, Scanner Upgrade, Scanner Vendors and Field Strengths
- 2.14 Integration of the Vascular Modeling Toolkit in 3D Slicer
- 2.15 New EMSegment Module in Slicer3
- 2.16 Interactive 3D Navigation System for Image-guided Surgery
- 2.17 Smaller Amygdala is Associated with Anxiety in Patients with Panic Disorder
- 2.18 Optimal Transseptal Puncture Location for Robot-assisted Left Atrial Catheter Ablation
- 2.19 Measurements from Image-based Three Dimensional Pelvic Floor Reconstruction: A Study of Inter- and Intraobserver Reliability
- 2.20 Three-dimensional Analysis of Rodent Paranasal Sinus Cavities from X-ray Computed Tomography (CT) Scans
- 2.21 Multimodal Imaging in Mild Cognitive Impairment: Metabolism, Morphometry and Diffusion of the Temporal–parietal Memory Network
- 2.22 The Relation between Connection Length and Degree of Connectivity in Young Adults: A DTI Analysis
- 2.23 The ROBOCAST Project: ROBOt and Sensors Integration for Computer Assisted Surgery and Therapy
- 2.24 A Trajectory Planning Method for Reduced Patient Risk in Image-guided Neurosurgery: Preliminary Results
- 2.25 Contrast-maximizing Adaptive Region Growing for CT
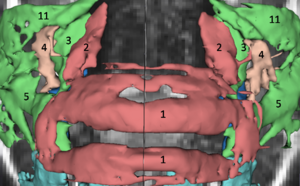
- 2.26 Computer-aided 3D Visualization in Oto-rhino-laryngology
- 2.27 Clinical Application of Curvilinear Distraction Osteogenesis for Correction of Mandibular Deformities
- 2.28 In Vivo Hippocampal Measurement and Memory: A Comparison of Manual Tracing and Automated Segmentation in a Large Community-Based Sample
- 2.29 How Volumetric Analysis Quantifies Therapeutic Response of Slow-flow Vascular Malformations
- 2.30 A Minimally Invasive Registration Method using Surface Template-assisted Marker Positioning (STAMP) for Image-guided Otologic Surgery
- 2.31 Diffusion Tractography of the Fornix in Schizophrenia
- 2.32 Spiny Versus Stubby: 3D Reconstruction of Human Myenteric (type I) Neurons
- 3 2008
- 3.1 An Integrated System for Planning, Navigation and Robotic Assistance for Skull Base Surgery
- 3.2 The Relationship between Diffusion Tensor Imaging and Volumetry as Measures of White Matter Properties
- 3.3 3D Modeling-based Surgical Planning in Transsphenoidal Pituitary Surgery - Preliminary Results
- 3.4 A Generic Framework for Internet-based Interactive Applications of High-resolution 3-D Medical Image Data
- 3.5 Anterior Cingulate Cortex Volume Reduction in Patients with Panic Disorder
- 3.6 Future Trends in Robotic Neurosurgery
- 3.7 A Computer Modelling Tool for Comparing Novel ICD Electrode Orientations in Children and Adults
- 3.8 Using Magnetic Resonance Microscopy to Study the Growth Dynamics of a Glioma Spheroid in Collagen I: A Case Study
- 3.9 Lowering the Barriers Inherent in Translating Advances in Neuroimage Analysis to Clinical Research Applications
- 4 2007
- 4.1 Towards Scarless Surgery: An Endoscopic Ultrasound Navigation System for Transgastric Access Procedures
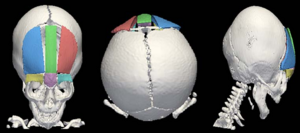
- 4.2 3D Visualization and Simulation of Frontoorbital Advancement in Metopic Synostosis
- 4.3 Creating Physical 3D Stereolithograph Models of Brain and Skull
- 4.4 Morphology, Constraints, and Scaling of Frontal Sinuses in the Hartebeest, Alcelaphus Buselaphus (Mammalia: Artiodactlya, Bovidae)
- 4.5 Image-guided Otologic Surgery Based on Patient Motion Compensation and Intraoperative Virtual CT
- 4.6 Non-rigid Registration of Pre-procedural MR Images with Intra- procedural Unenhanced CT Images for Improved Targeting of Tumors During Liver Radiofrequency Ablations
- 4.7 A Detailed 3D Model of the Guinea Pig Cochlea
- 4.8 Dynamic 3-D Computer Modeling Tracks Brain Changes During Surgery
- 4.9 Surface Rendering-based Virtual Intraventricular Endoscopy: Retrospective Feasibility Study and Comparison to Volume Rendering-based Approach
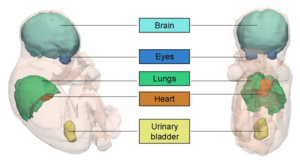
- 4.10 Interest of the Steady State Free Precession (SSFP) Sequence for 3D Modeling of the Whole Fetus
- 4.11 Longitudinal in Vivo Reproducibility of Cartilage Volume and Surface in Osteoarthritis of the Knee
- 4.12 A Novel Manipulator for 3D Ultrasound Guided Percutaneous Needle Insertion
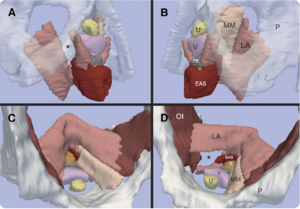
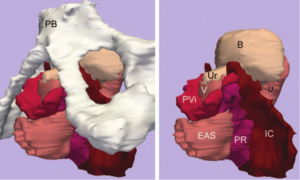
- 4.13 Origin and Insertion Points Involved in Levator Ani Muscle Defects
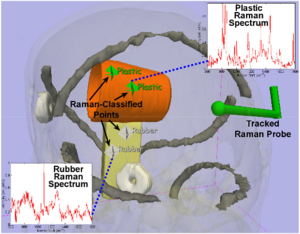
- 4.14 A Prototype Biosensor-integrated Image-guided Surgery System
- 4.15 Accuracy Evaluation of Initialization-free Registration for Intraoperative 3D-navigation
- 4.16 Development of a Three-dimensional Multiscale Agent-based Tumor Model: Simulating Gene-protein Interaction Profiles, Cell Phenotypes and Multicellular Patterns in Brain Cancer
- 4.17 Image Registered FAST (IRFAST) for Combat Casualty Triage
- 4.18 A Preliminary Study on the Relationship between Nasal Cavity and Maxillary Sinus Volumes
- 4.19 Interobserver Variability in the Determination of Upper Lobe-predominant Emphysema
- 4.20 Registered, Sensor-integrated Virtual Reality for Surgical Applications
- 4.21 Modeling Cancer Biology
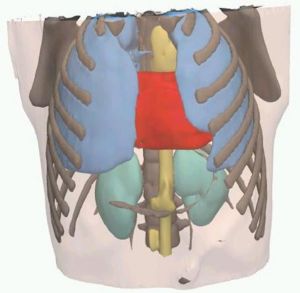
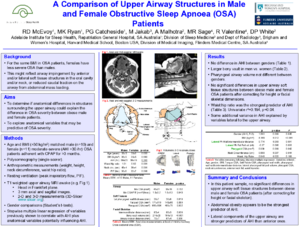
- 4.22 A Comparison of Upper Airway Structures in Male and Female Obstructive Sleep Apnoea (OSA) Patients
- 5 2006
- 5.1 Shaving Diffusion Tensor Images in Discriminant Analysis: A Study into Schizophrenia
- 5.2 Interventional Navigation for Abdominal Surgery by Simultaneous Use of MRI and Ultrasound
- 5.3 Diffusion Tensor Imaging Reveals White Matter Reorganization in Early Blind Humans
- 5.4 Molar Crown Thickness, Volume, and Development in South African Middle Stone Age Humans
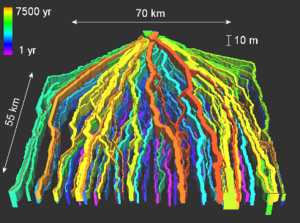
- 5.5 A 3D Model Simulating Sediment Transport, Erosion and Deposition within a Network of Channel Belts and an Associated Floodplain
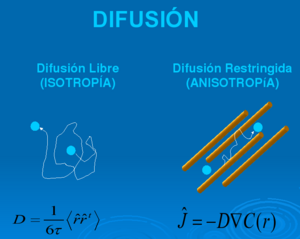
- 5.6 Molecular Diffusion in MRI: Technical Application of Fiber Tracking
- 5.7 Quantification of Levator Ani Cross-sectional Area Differences between Women with and Those without Prolapse
- 5.8 Liver Metastases: 3D Shape-based Analysis of CT Scans for Detection of Local Recurrence After Radiofrequency Ablation
- 5.9 Atlas Guided Identification of Brain Structures by Combining 3D Segmentation and SVM Classification
- 5.10 Development of a CAD (Computer Assisted Detection) System to Detect Lung Nodules in CT Scans
- 5.11 Dynamic Simulation of Joints using Multi-Scale Modeling
- 5.12 Quasi-isometric Flattening of Curved Surfaces for Medical Imaging
- 5.13 A Translation Station for Imaging
- 5.14 User-guided 3D Active Contour Segmentation of Anatomical Structures: Significantly Improved Efficiency and Reliability
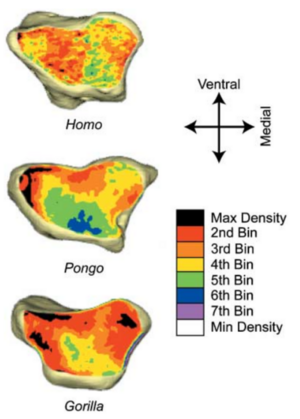
- 5.15 Habitual Use of the Primate Forelimb is Reflected in the Material Properties of Subchondral Bone in the Distal Radius
- 5.16 Appearance of the Levator Ani Muscle Subdivisions in Magnetic Resonance Images
- 5.17 Virtual Cystoscopy - A Surgical Planning and Guidance Tool
- 5.18 Measurement of the Pubic Portion of the Levator Ani Muscle in Women with Unilateral Defects in 3D Models from MR Images
- 5.19 Finite-element-method (FEM) Model Generation of Time-resolved 3D Echocardiographic Geometry Data for Mitral-valve Volumetry
- 5.20 Range of Curvilinear Distraction Devices Required for Treatment of Mandibular Deformities
- 5.21 Preliminary Study on Digitized Nasal and Temporal Bone Anatomy
- 5.22 Developmental Response to Cold Stress in Cranial Morphology of Rattus: Implications for the Interpretation of Climatic Adaptation in Fossil Hominins
- 5.23 A Ceratopsid Dinosaur Parietal from New Mexico and Its Implications for Ceratopsid Biogeography and Systematics
- 6 2005
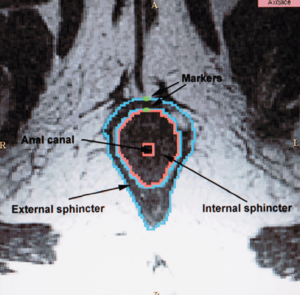
- 6.1 Magnetic Resonance Imaging and 3-Dimensional Analysis of External Anal Sphincter Anatomy
- 6.2 Group-Slicer: A Collaborative Extension of 3D Slicer
- 6.3 2D Rigid Registration of MR Scans using the 1D Binary Projections
- 6.4 Preoperative Hepatic 3D Models: Virtual Liver Resection using Three-dimensional Imaging Technique
- 6.5 Three-dimensional Reconstruction and Volumetry of Intracranial Haemorrhage and its Mass Effect
- 6.6 Vaginal Thickness, Cross-Sectional Area, and Perimeter in Women with and Those without Prolapse
- 6.7 Registration and Fusion of CT and MRI of the Temporal Bone
- 6.8 Open-configuration MR-guided Microwave Thermocoagulation Therapy for Metastatic Liver Tumors from Breast Cancer]
- 6.9 Quantification of Airway Diameters and 3D Airway Tree Rendering from Dynamic Hyperpolarized 3He Magnetic Resonance Imaging
- 6.10 A Finite Element Method Model to Simulate Laser Interstitial Thermo Therapy in Anatomical Inhomogeneous Regions
- 6.11 The Application of DTI to Investigate White Matter Abnormalities in Schizophrenia
- 7 2004
- 7.1 A Statistically Based Flow for Image Segmentation
- 7.2 Decreases in Ventricular Volume Correlate with Decreases in Ventricular Pressure in Idiopathic Normal Pressure Hydrocephalus Patients Who Experienced Clinical Improvement after Implantation with Adjustable Valve Shunts
- 7.3 Spatial Motion Constraints in Medical Robot using Virtual Fixtures Generated by Anatomy
- 7.4 Clinical Validation of the Normalized Mutual Information Method for Registration of CT and MR Images in Radiotherapy of Brain Tumors
- 7.5 Diffusion-tensor Imaging–guided Tracking of Fibers of the Pyramidal Tract Combined with Intraoperative Cortical Stimulation Mapping in Patients with Gliomas
- 7.6 Abnormal Association Between Reduced Magnetic Mismatch Field to Speech Sounds and Smaller Left Planum Temporale Volume in Schizophrenia
- 8 2003
- 8.1 Genetic Contribution to Cartilage Volume in Women: A Classical Twin Study
- 8.2 Advanced Computer Assistance for Magnetic Resonance-guided Microwave Thermocoagulation of Liver Tumors
- 8.3 The Association of Cartilage Volume with Knee Pain
- 8.4 Three-dimensional Reconstruction of Magnetic Resonance Images of the Anal Sphincter and Correlation between Sphincter Volume and Pressure
- 8.5 Surgical Navigation in the Open MRI
- 8.6 The Virtual Craniofacial Patient: 3D Jaw Modeling and Animation
- 9 2002
- 10 2001
- 11 2000
2010
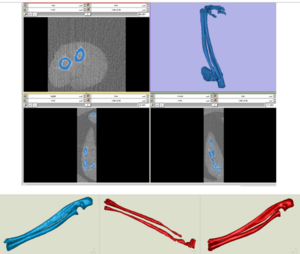
Application of Vascular Model Toolkit (VMTK) for Coronary Arteries
|
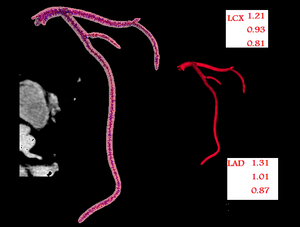
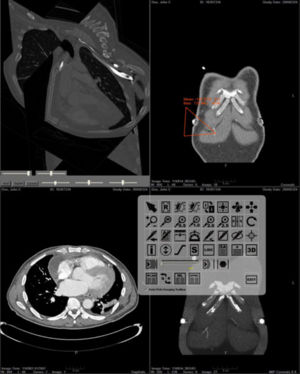
Publication: Presented at 62nd Cardiological Society of India Conference, Kolkata, India, 2010 Dec; | PDF Authors: Christopher J, Mohan R, Duraikannu C, Kishore LT, Raju K. Institution: Care Hospitals, Hyderabad, India Background/Purpose: Functional evaluation of coronary arteries involves study of their 3D shapes and diameters. Segmentation of vascular structures from 3D-Computerized Tomographic Angiogram (CTA) images can be achieved by using VMTK. This gives: (1) a polygonal surface model of vascular structures having centerline based geometric quantities and (2) compute centerlines and Maximal Inscribed Sphere Radius (MISR) of branching tubular structures (Voronoi image). VMTK module integrated in 3D Slicer is used as it allows use of other 3D Slicer modules for processing of images. We use: VesselEnhancement, EasyLevelsetSegmentation and Centerlines modules for study. |
Ion-Abrasion Scanning Electron Microscopy Reveals Surface-Connected Tubular Conduits in HIV-Infected Macrophages
|
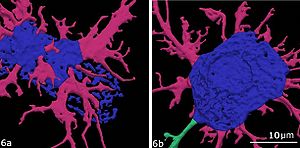
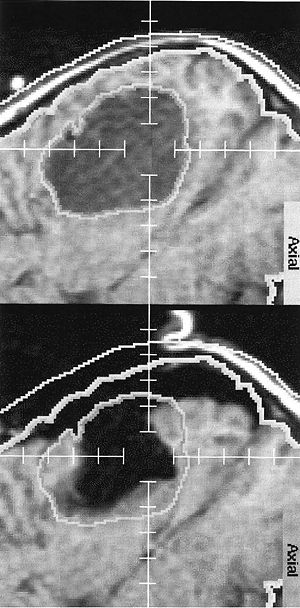
Publication: PLoS Pathog. 2010 Sep;5(9):e1000591. PMID: 19779568 | PDF Authors: Bennett AE, Narayan K, Shi D, Hartnell LM, Gousset K, He H, Lowekamp BC, Yoo TS, Bliss D, Freed EO, Subramaniam S. Institution: Laboratory of Cell Biology, Center for Cancer Research, NCI, NIH, Bethesda, MD, USA. Background/Purpose: HIV-1-containing internal compartments are readily detected in images of thin sections from infected cells using conventional transmission electron microscopy, but the origin, connectivity, and 3D distribution of these compartments has remained controversial. Here, we report the 3D distribution of viruses in HIV-1-infected primary human macrophages using cryo-electron tomography and ion-abrasion scanning electron microscopy (IA-SEM), a recently developed approach for nanoscale 3D imaging of whole cells. Using IA-SEM, we show the presence of an extensive network of HIV-1-containing tubular compartments in infected macrophages, with diameters of 150-200 nm, and lengths of up to 5 mm that extend to the cell surface from vesicular compartments that contain assembling HIV-1 virions. These types of surface-connected tubular compartments are not observed in T cells infected with the 29/31 KE Gag-matrix mutant where the virus is targeted to multi-vesicular bodies and released into the extracellular medium. IA-SEM imaging also allows visualization of large sheet-like structures that extend outward from the surfaces of macrophages, which may bend and fold back to allow continual creation of viral compartments and virion-lined channels. This potential mechanism for efficient virus trafficking between the cell surface and interior may represent a subversion of pre-existing vesicular machinery for antigen capture, processing, sequestration, and presentation. Funding:
|
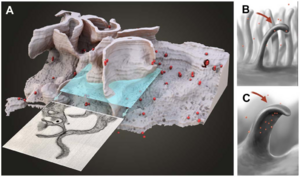 3D representation of the surface and interior of an HIV-infected macrophage (animation is presented in Video S10). (A) Sections that would appear to contain ‘‘filopodia’’ when imaged by transmission electron microscopy of individual sections can actually correspond to large wavelike membrane processes as in this example. The virions are shown in red. (B, C) Schematic side (B) and front (C) views of these surface protrusions shown to indicate how bending and folding back of the extensions onto the surface of the cell could trap the contents of the aqueous environment within the invaginated folds of the membrane, and allow creation of viral compartments. |
MRI-Guided Robotic Prostate Biopsy: A Clinical Accuracy Validation
|
Publication: Int Conf Med Image Comput Comput Assist Interv. 2010 Sep;13(Pt 3):383-391. PMID: 20879423 | PDF Authors: Xu H, Lasso A, Vikal S, Guion P, Krieger A, Kaushal A, Whitcomb LL, Fichtinger G. Institutions: Queen's University, Kingston, ON, Canada.
Funding:
|
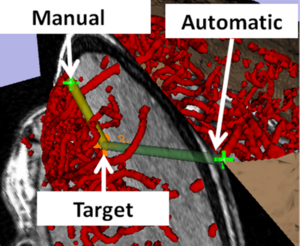
A Method for Planning Safe Trajectories in Image-guided Keyhole Neurosurgery
|
Publication: Med Image Comput Comput Assist Interv. 2010 Sep;13(Pt 3):457-64. PMID: 20879432 | PDF Authors: Shamir RR, Tamir I, Dabool E, Joskowicz L, Shoshan Y. Institution: School of Engineering and Computer Science, Hebrew University, Jerusalem, Israel. Background/Purpose: We present a new preoperative planning method for reducing the risk associated with insertion of straight tools in image-guided keyhole neurosurgery. The method quantifies the risks of multiple candidate trajectories and presents them on the outer head surface to assist the neurosurgeon in selecting the safest path. The surgeon can then define and/or revise the trajectory, add a new one using interactive 3D visualization, and obtain a quantitative risk measures. The trajectory risk is evaluated based on the tool placement uncertainty, on the proximity of critical brain structures, and on a predefined table of quantitative geometric risk measures. Our results on five targets show a significant reduction in trajectory risk and a shortening of the preoperative planning time as compared to the current routine method. Funding:
|
JHU Workshop for Talented Youth
|
Publication: Workshop for Talented Youth, 2010 Sep; Author: Wyatt C. Institution: John Hopkins University, Baltimore, MD. Background/Purpose: This 2010 workshop for the JHU Center for Talented Youth was hosted at Virginia Tech and focused on neuroscience. The event included an interactive session titled "Brain Shape: Using images to predict the development of Alzheimer's Disease." The session included a short introduction to neuroimaging, followed by students, alone or in pairs, using t3D Slicer software to compare healthy and pathological images of the brain. 100 students ranging in age from 13 to 16 years old attended the event. |
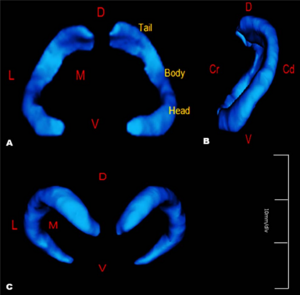
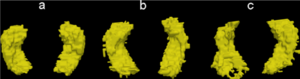
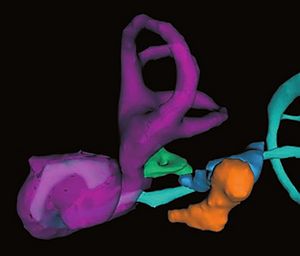
Canine Hippocampal Formation Composited Into Three-dimensional Structure using MPRAGE
|
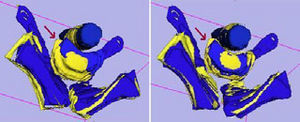
Publication: J Vet Med Sci. 2010 Jul;72(7):853-60. PMID: 20179383 | PDF Authors: Jung MA, Lee MS, Lee IH, Lee AR, Jang DP, Kim YB, Cho ZH, Nahm SS, Eom KD. Institution: Department of Veterinary Radiology and Diagnostic Imaging, College of Veterinary Medicine, Konkuk University. Background/Purpose: This study was performed to anatomically illustrate the living canine hippocampal formation in three-dimensions (3D), and to evaluate its relationship to surrounding brain structures. Three normal beagle dogs were scanned on a MR scanner with inversion recovery segmented three-dimensoinal gradient echo sequence (known as MP-RAGE: Magnetization Prepared Rapid Gradient Echo). The MRI data was manually segmented and reconstructed into a three-dimensional model using the 3D Slicer software tool. From the three-dimensional model, the spatial relationships between hippocampal formation and surrounding structures were evaluated. With the increased spatial resolution and contrast of the MPRAGE, the canine hippocampal formation was easily depicted. The reconstructed three-dimensional image allows easy understanding of the hippocampal contour and demonstrates the structural relationship of the hippocampal formation to surrounding structures in vivo. Funding:
|
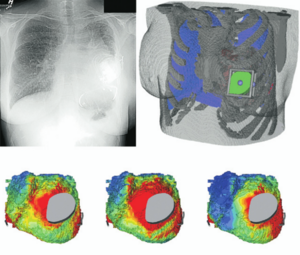
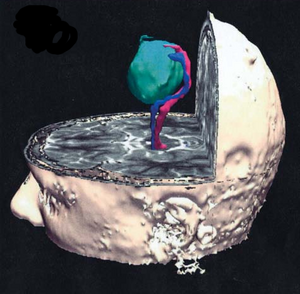
|
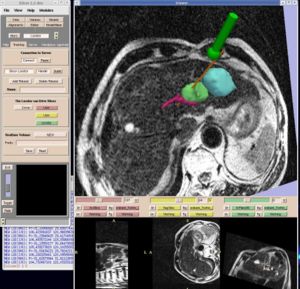
Publication: J Am Coll Surg. 2010 Jun;210(6):927-33. PMID: 20510801 | PDF Authors: Tomikawa M, Hong J, Shiotani S, Tokunaga E, Konishi K, Ieiri S, Tanoue K, Akahoshi T, Maehara Y, Hashizume M. Institution: Department of Future Medicine and Innovative Medical Information, Graduate School of Medical Sciences, Kyushu University, Higashi-ku, Fukuoka, Japan. Background/Purpose: The aim of this study was to report on the early experiences using a real-time 3-dimensional (3D) virtual reality navigation system with open MRI for breast-conserving surgery. We developed a real-time 3D virtual reality navigation system with open MRI, and evaluated the mismatch between the navigation system and real distance using a 3D phantom. Two patients with nonpalpable MRI-detected breast tumors underwent breast-conserving surgery under the guidance of the navigation system. An initial MRI for the breast tumor using skin-affixed markers was performed immediately before excision. A percutaneous intramammary dye marker was applied to delineate an excision line, and the computer software 3D Slicer generated a real-time 3D virtual reality model of the tumor and the puncture needle in the breast. Excision of the tumor was performed in the usual manner along the excision line indicated with the dye. The resected specimens were carefully examined histopathologically. The mean mismatch between the navigation system and real distance was 2.01±0.32 mm when evaluated with the 3D phantom. Under guidance by the navigation system, a percutaneous intramammary dye marker was applied without any difficulty. Fiducial registration errors were 3.00 mm for patient no. 1, and 4.07 mm for patient no. 2. Histopathological examinations of the resected specimens of the 2 patients showed noninvasive ductal carcinoma in situ. The surgical margins were free of carcinoma cells. Real-time 3D virtual reality navigation system with open MRI is feasible for safe and accurate excision of nonpalpable MRI-detected breast tumors. Long-term outcomes of this technique should be evaluated further. |
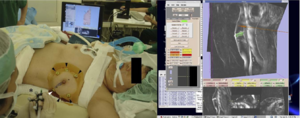 Left, percutaneous intramammary injection of dye in the syringe to make a dissection line of the tumor with the navigation of 3D Slicer. Arrowheads, skin markers; asterisk, a syringe attached with infrared markers; right, virtual MR images on the monitor of 3D Slicer reflecting the same slice as the puncture line. A breast tumor is indicated in green; a needle and a puncture line are indicated in red. |
Interfaces and Integration of Medical Image Analysis Frameworks: Challenges and Opportunities
|
Publication: Annu ORNL Biomed Sci Eng Cent Conf. 2010 May 25;2010:1-4. PMID: 21151892 | PDF Authors: Covington K, McCreedy ES, Chen M, Carass A, Aucoin N, Landman BA. Institution: Department of Electrical Engineering, Vanderbilt University, Nashville, TN, USA. Background/Purpose: Clinical research with medical imaging typically involves large-scale data analysis with interdependent software toolsets tied together in a processing workflow. Numerous, complementary platforms are available, but these are not readily compatible in terms of workflows or data formats. Both image scientists and clinical investigators could benefit from using the framework which is a most natural fit to the specific problem at hand, but pragmatic choices often dictate that a compromise platform is used for collaboration. Manual merging of platforms through carefully tuned scripts has been effective, but exceptionally time consuming and is not feasible for large-scale integration efforts. Hence, the benefits of innovation are constrained by platform dependence. Removing this constraint via integration of algorithms from one framework into another is the focus of this work. We propose and demonstrate a light-weight interface system to expose parameters across platforms and provide seamless integration. In this initial effort, we focus on four platforms Medical Image Analysis and Visualization (MIPAV), Java Image Science Toolkit (JIST), command line tools, and 3D Slicer. We explore three case studies: (1) providing a system for MIPAV to expose internal algorithms and utilize these algorithms within JIST, (2) exposing JIST modules through self-documenting command line interface for inclusion in scripting environments, and (3) detecting and using JIST modules in 3D Slicer. We review the challenges and opportunities for light-weight software integration both within development language (e.g., Java in MIPAV and JIST) and across languages (e.g., C/C++ in 3D Slicer and shell in command line tools). Funding:
|
Evaluation of Robotic Needle Steering in Ex Vivo Tissue
|
Publication: IEEE Int Conf Robot Autom. 2010 May 3;2010:2068-2073. PMID: 21339851 | PDF Authors: Majewicz A, Wedlick TR, Reed KB, Okamura AM. Institution: Department of Mechanical Engineering, Laboratory for Computational Sensing and Robotics, Johns Hopkins University, Baltimore, MD, USA. Background/Purpose: Insertion velocity, tip asymmetry, and shaft diameter may influence steerable needle insertion paths in soft tissue. In this paper we examine the effects of these variables on needle paths in ex vivo goat liver, and demonstrate practical applications of robotic needle steering for ablation, biopsy, and brachytherapy. All experiments were performed using a new portable needle steering robot that steers asymmetric-tip needles under fluoroscopic imaging. For bevel-tip needles, we found that larger diameter needles resulted in less curvature, i.e. less steerability, confirming previous experiments in artificial tissue. The needles steered with radii of curvature ranging from 3:4 cm (for the most steerable pre-bent needle) to 2:97m (for the least steerable bevel needle). Pre-bend angle significantly affected needle curvature, but bevel angle did not. We hypothesize that biological tissue characteristics such as inhomogeneity and viscoelasticity significantly increase path variability. These results underscore the need for closed-loop image guidance for needle steering in biological tissues with complex internal structure. Funding:
|
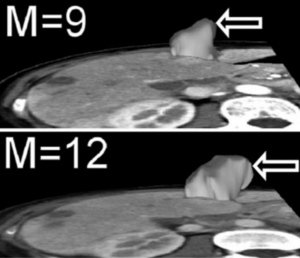
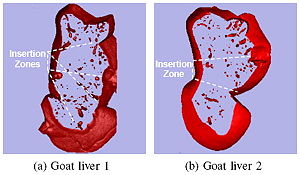 Slices of volume-rendered goat livers generated using fluoroscopic images and 3D Slicer software. |
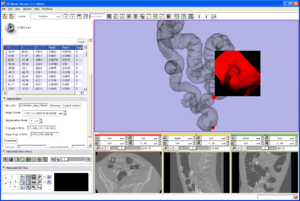
An Open Source Implementation of Colon CAD in 3D Slicer
|
Publication: Proc. of SPIE 2010. Vol. 7624 762421-2 | PDF Authors: Xu H, Gage HD, Santago P. Institution: Department of Biomedical Engineering, Wake Forest University Health Sciences, Winston-Salem, NC, USA. Background/Purpose: Most colon CAD (computer aided detection) software products, especially commercial products, are designed for use by radiologists in a clinical environment. Therefore, those features that effectively assist radiologists in finding polyps are emphasized in those tools. However, colon CAD researchers, many of whom are engineers or computer scientists, are working with CT studies in which polyps have already been identified using CT Colonography (CTC) and/or optical colonoscopy (OC). Their goal is to utilize that data to design a computer system that will identify all true polyps with no false positive detections. Therefore, they are more concerned with how to reduce false positives and to understand the behavior of the system than how to find polyps. Thus, colon CAD researchers have different requirements for tools not found in current CAD software. We have implemented a module in 3D Slicer to assist these researchers. As with clinical colon CAD implementations, the ability to promptly locate a polyp candidate in a 2D slice image and on a 3D colon surface is essential for researchers. Our software provides this capability, and uniquely, for each polyp candidate, the prediction value from a classifier is shown next to the 3D view of the polyp candidate, as well as its CTC/OC finding. This capability makes it easier to study each false positive detection and identify its causes. We describe features in our colon CAD system that meets researchers’ specific requirements. Our system uses an open source implementation of a 3D Slicer module, and the software is available to the public for use and for extension (http://www2.wfubmc.edu/ctc/download/). Funding:
|
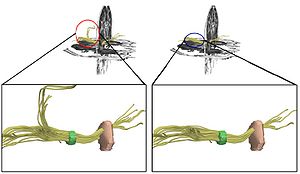
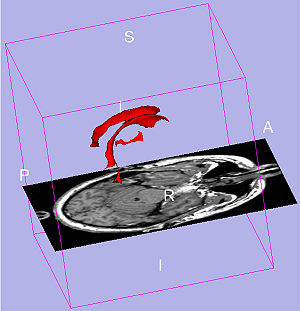
In Vivo Visualization of Cranial Nerve Pathways in Humans using Diffusion-Based Tractography
|
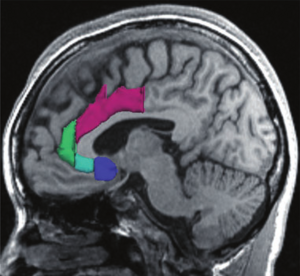
Publication: Neurosurgery. 2010 Apr;66(4):788-95; discussion 795-6. PMID: 20305498 | PDF Authors: Hodaie M, Quan J, Chen DQ. Institution: Division of Neurosurgery, University of Toronto and Toronto Western Hospital, Toronto, ON, Canada. Background/Purpose: Diffusion-based tractography has emerged as a powerful technique for 3-dimensional tract reconstruction and imaging of white matter fibers; however, tractography of the cranial nerves has not been well studied. In particular, the feasibility of tractography of the individual cranial nerves has not been previously assessed. Methods: 3-Tesla magnetic resonance imaging scans, including anatomic magnetic resonance images and diffusion tensor images, were used for this study. Tractography of the cranial nerves was performed using 3D Slicer software. The reconstructed 3-dimensional tracts were overlaid onto anatomic images for determination of location and course of intracranial fibers. Detailed tractography of the cranial nerves was obtained, although not all cranial nerves were imaged with similar anatomic fidelity. Some tracts were imaged in great detail (cranial nerves II, III, and V). Tractography of the optic apparatus allowed tracing from the optic nerve to the occipital lobe, including Meyer's loop. Trigeminal tractography allowed visualization of the gasserian ganglion as well as postganglionic fibers. Tractography of cranial nerve III shows the course of the fibers through the midbrain. Lower cranial nerves (cranial nerves IX, XI, and XII) could not be imaged well. Tractography of the cranial nerves is feasible, although technical improvements are necessary to improve the tract reconstruction of the lower cranial nerves. Detailed assessment of anatomy and the ability of overlaying the tracts onto anatomic magnetic resonance imaging scans is essential, particularly in the posterior fossa, to ensure that the tracts have been reconstructed with anatomic fidelity. |
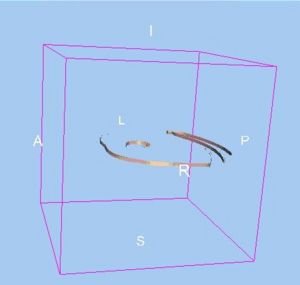
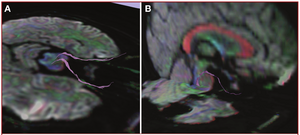 Intra- and extracranial course of cranial nerve III, depicted onto mixed anatomic/color-by-orientation MRI slices. Images are overlaid onto axial MRI slices (A) and sagittal MRI slices (B). The intracranial course takes a sharp angle, after which the fibers appear to enter the medial longitudinal fasciculus. The large commissural fibers of the corpus callosum (red) and fornix (blue) can be easily visualized on the sagittal slices. (Please see also Supplementary Digital Content 2, Figure 2, a 3-dimensional representation of the oculomotor nerves.) |
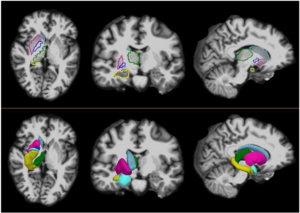
Brain Maturation in Adolescence and Young Adulthood: Regional Age-Related Changesi in Cortical Thickness and White Matter Volume and Microstructure
|
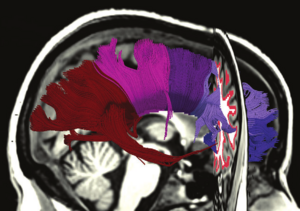
Publication: Cereb Cortex. 2010 Mar;20(3):534-48. PMID: 19520764 | PDF Authors: Tamnes CK, Ostby Y, Fjell AM, Westlye LT, Due-Tønnessen P, Walhovd KB. Institution: Center for the Study of Human Cognition, Department of Psychology, University of Oslo, Oslo, Norway. Background/Purpose: The development of cortical gray matter, white matter (WM) volume, and WM microstructure in adolescence is beginning to be fairly well characterized by structural magnetic resonance imaging (sMRI) and diffusion tensor imaging (DTI) studies. However, these aspects of brain development have rarely been investigated concurrently in the same sample and hence the relations between them are not understood. We delineated the age-related changes in cortical thickness, regional WM volume, and diffusion characteristics and investigated the relationships between these properties of brain development. One hundred and sixty-eight healthy participants aged 8-30 years underwent sMRI and DTI. The results showed regional age-related cortical thinning, WM volume increases, and changes in diffusion parameters. Cortical thickness was the most strongly age-related parameter. All classes of measures showed unique associations with age. The results indicate that cortical thinning in adolescence cannot be explained by WM maturation in underlying regions as measured by volumetry or DTI. Moderate associations between cortical thickness and both volume and diffusion parameters in underlying WM regions were also found, although the relationships were not strong. It is concluded that none of the measures are redundant and that the integration of the 3 will yield a more complete understanding of brain maturation. |
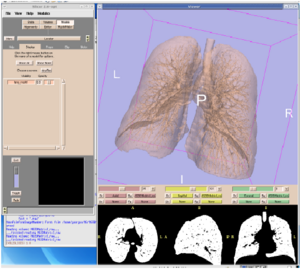
 Three-dimensional renderings of the probabilistic tracts. The 11 atlas-based probabilistic tracts from the Mori atlas are shown as 3D renderings in anterior, left, and dorsal views, displayed on a semitransparent template brain from FreeSurfer (fsaverage). Color codes refer to: Dark brown: Anterior thalamic radiation (ATR), Blue: Cingulum- cingulate gyrus (CCG), Purple: Cingulum-hippocampus gyrus (CHG), Dark blue: Cortico-spinal tract (CST), Pink: Forceps major (FMa), Red: Forceps minor (FMi), Brown: Inferior fronto-occipital fasciculus (IFOF), Orange: Inferior longitudinal fasciculus (ILF), Dark green: Superior longitudinal fasciculus (SLF), Green: Superior longitudinal fasciculus temporal part (SLFTP), and Yellow: Uncinate fasciculus (UF). The figure was made by the use of 3D Slicer software. |
Coronary Artery Centerline Extraction in 3D Slicer using VMTK based Tools
|
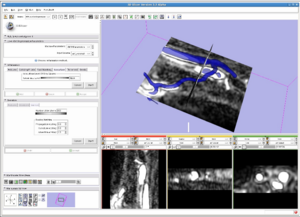
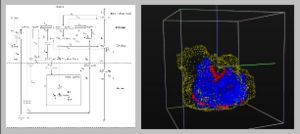
Publication: Master's Thesis, University of Heidelberg 2010 Feb; | PDF Author: Daniel Hähn Institution: Medical Informatics, University of Heidelberg, Heidelberg, Germany. Background/Purpose: Atherosclerosis of the coronary arteries leads to Coronary Artery Disease (CAD) and is one of the main causes of death worldwide. Diagnosis and investigation of the severity of atherosclerosis is performed through medical imaging. In this context, the central lumen line of coronary arteries is of importance because it can be used for visualization and reconstruction based on reformatted images. We studied algorithms performing vessel enhancement filtering, level set segmentation and centerline computation based on Delaunay tessellation. By composing a pipeline of these, it is possible to extract the centerlines of coronary arteries in Computed Tomography Angiography (CTA) images. We implemented the pipeline as modules in 3D Slicer, an application providing a wide range of tools for medical image processing. This was accomplished by using methods of the Vascular Modeling Toolkit, an open source framework for image-based modeling of blood vessels. We evaluated the pipeline on eight CTA datasets by extracting the centerlines of the right and left coronary arteries. Using a large-scale parameter exploration study, we could achieve an average overlap over 72% of the clinically relevant part of the vessels combined with an average accuracy of 0.47 mm by finding individual parameters for each dataset. Through a leave-one-out cross validation approach, we recognized parameter sets targeting the different branches of the arteries suitable for all datasets. Nevertheless, the found pattern lowers the average overlap to 54% and the average accuracy to 0.66 mm. The software modules created during this project are available as open source software and suitable for end-users. Funding:
|
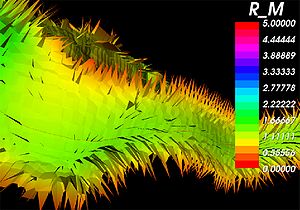 A close-up of the internal Voronoi diagram and the corresponding centerline of a blood vessel obtained using the created tools in 3D Slicer. The individual Voronoi regions are visible as ”tiles” where the color indicates the maximum inscribed sphere radius R_M ( x ) [vx]. Surface noise leads to the small perturbations visible as spikes near the vessel lumen wall. |
Assessment of Image Registration Accuracy in Three-dimensional Transrectal Ultrasound Guided Prostate Biopsy
|
Publication: Med Phys. 2010 Feb;37(2):802-13. PMID: 20229890 Authors: Karnik VV, Fenster A, Bax J, Cool DW, Gardi L, Gyacskov I, Romagnoli C, Ward AD. Institution: Biomedical Engineering Graduate Program, University of Western Ontario, London, ON, Canada. Background/Purpose: Prostate biopsy, performed using two-dimensional (2D) transrectal ultrasound (TRUS) guidance, is the clinical standard for a definitive diagnosis of prostate cancer. Histological analysis of the biopsies can reveal cancerous, noncancerous, or suspicious, possibly precancerous, tissue. During subsequent biopsy sessions, noncancerous regions should be avoided, and suspicious regions should be precisely rebiopsied, requiring accurate needle guidance. It is challenging to precisely guide a needle using 2D TRUS due to the limited anatomic information provided, and a three-dimensional (3D) record of biopsy locations for use in subsequent biopsy procedures cannot be collected. Our tracked, 3D TRUS-guided prostate biopsy system provides additional anatomic context and permits a 3D record of biopsies. However, targets determined based on a previous biopsy procedure must be transformed during the procedure to compensate for intraprocedure prostate shifting due to patient motion and prostate deformation due to transducer probe pressure. Thus, registration is a critically important step required to determine these transformations so that correspondence is maintained between the prebiopsied image and the real-time image. Registration must not only be performed accurately, but also quickly, since correction for prostate motion and deformation must be carried out during the biopsy procedure. The authors evaluated the accuracy, variability, and speed of several surface-based and image-based intrasession 3D-to-3D TRUS image registration techniques, for both rigid and nonrigid cases, to find the required transformations. Our surface-based rigid and nonrigid registrations of the prostate were performed using the iterative-closest-point algorithm and a thin-plate spline algorithm, respectively. For image-based rigid registration, the authors used a block matching approach, and for nonrigid registration, the authors define the moving image deformation using a regular, 3D grid of B-spline control points. The authors measured the target registration error (TRE) as the postregistration misalignment of 60 manually marked, corresponding intrinsic fiducials. The authors also measured the fiducial localization error (FLE), the effect of segmentation variability, and the effect of fiducial distance from the transducer probe tip. Lastly, the authors performed 3D principal component analysis (PCA) on the x, y, and z components of the TREs to examine the 95% confidence ellipsoids describing the errors for each registration method. Using surface-based registration, the authors found mean TREs of 2.13±0.80 and 2.09±0.77 mm for rigid and nonrigid techniques, respectively. Using image-based rigid and non-rigid registration, the authors found mean TREs of 1.74±0.84 and 1.50±0.83 mm, respectively. Our FLE was 0.21 mm and did not dominate the overall TRE. However, segmentation variability contributed substantially approximately 50%) to the TRE of the surface-based techniques. PCA showed that the 95% confidence ellipsoid encompassing fiducial distances between the source and target registration images was reduced from 3.05 to 0.14 cm3, and 0.05 cm3 for the surface-based and image-based techniques, respectively. The run times for both registration methods were comparable at less than 60 s. Our results compare favorably with a clinical need for a TRE of less than 2.5 mm, and suggest that image-based registration is superior to surface-based registration for 3D TRUS-guided prostate biopsies, since it does not require segmentation. |
Language Laterality in Autism Spectrum Disorder and Typical Controls: A Functional, Volumetric, and Diffusion Tensor MRI Study
|
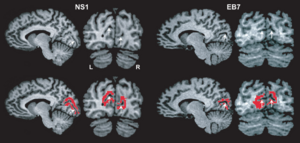
Publication: Brain Lang. 2010 Feb;112(2):113-20. PMID: 20031197 | PDF Authors: Knaus TA, Silver AM, Kennedy M, Lindgren KA, Dominick KC, Siegel J, Tager-Flusberg H. Institution: Department of Anatomy and Neurobiology, Boston University School of Medicine, Boston, MA, USA. Background/Purpose: Language and communication deficits are among the core features of autism spectrum disorder (ASD). Reduced or reversed asymmetry of language has been found in a number of disorders, including ASD. Studies of healthy adults have found an association between language laterality and anatomical measures but this has not been systematically investigated in ASD. The goal of this study was to examine differences in gray matter volume of perisylvian language regions, connections between language regions, and language abilities in individuals with typical left lateralized language compared to those with atypical (bilateral or right) asymmetry of language functions. Fourteen adolescent boys with ASD and 20 typically developing adolescent boys participated, including equal numbers of left- and right-handed individuals in each group. Participants with typical left lateralized language activation had smaller frontal language region volume and higher fractional anisotropy of the arcuate fasciculus compared to the group with atypical language laterality, across both ASD and control participants. The group with typical language asymmetry included the most right-handed controls and fewest left-handers with ASD. Atypical language laterality was more prevalent in the ASD than control group. These findings support an association between laterality of language function and language region anatomy. They also suggest anatomical differences may be more associated with variation in language laterality than specifically with ASD. Language laterality therefore may provide a novel way of subdividing samples, resulting in more homogenous groups for research into genetic and neurocognitive foundations of developmental disorders. |
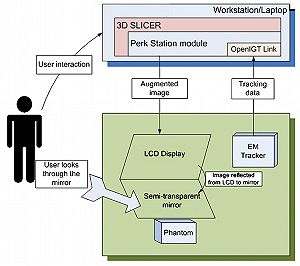
Perk Station-Percutaneous Surgery Training and Performance Measurement Platform
|
Publication: Comput Med Imaging Graph. 2010 Jan;34(1):19-32. PMID: 19539446 | PDF Authors: Vikal S, U-Thainual P, Carrino JA, Iordachita I, Fischer GS, Fichtinger G. Institution: Queen's University, Kingston, ON, Canada. Background/Purpose: Image-guided percutaneous (through the skin) needle-based surgery has become part of routine clinical practice in performing procedures such as biopsies, injections and therapeutic implants. A novice physician typically performs needle interventions under the supervision of a senior physician; a slow and inherently subjective training process that lacks objective, quantitative assessment of the surgical skill and performance. Shortening the learning curve and increasing procedural consistency are important factors in assuring high-quality medical care. This paper describes a laboratory validation system, called Perk Station, for standardized training and performance measurement under different assistance techniques for needle-based surgical guidance systems. The initial goal of the Perk Station is to assess and compare different techniques: 2D image overlay, biplane laser guide, laser protractor and conventional freehand. The main focus of this manuscript is the planning and guidance software system developed on the 3D Slicer platform, a free, open source software package designed for visualization and analysis of medical image data. The prototype Perk Station has been successfully developed, the associated needle insertion phantoms were built, and the graphical user interface was fully implemented. The system was inaugurated in undergraduate teaching and a wide array of outreach activities. Initial results, experiences, ongoing activities and future plans are reported. Funding:
|
2009
Three-dimensional Appearance of the Lips Muscles with Three-dimensional Isotropic MRI: In Vivo Study
|
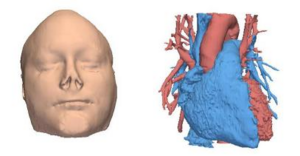
Publication: Int J Comput Assist Radiol Surg. 2009 Jun;4(4):349-52. PMID: 20033581 | PDF Authors: Olszewski R, Liu Y, Duprez T, Xu TM, Reychler H. Institution: Department of Oral and Maxillofacial Surgery, Cliniques Universitaires Saint Luc, Université Catholique de Louvain, Brussels, Belgium. Background/Purpose: Our knowledge of facial muscles is based primarily on atlases and cadaveric studies. This study describes a non-invasive in vivo method (3D MRI) for segmenting and reconstructing facial muscles in a three-dimensional fashion. Three-dimensional (3D), T1-weighted, 3 Tesla, isotropic MRI was applied to a subject. One observer performed semi-automatic segmentation using the Editor module from the 3D Slicer software (Harvard Medical School, Boston, MA, USA), version 3.2. We were able to successfully outline and three-dimensionally reconstruct the following facial muscles: pars labialis orbicularis oris, m. levatro labii superioris alaeque nasi, m. levator labii superioris, m. zygomaticus major and minor, m. depressor anguli oris, m. depressor labii inferioris, m. mentalis, m. buccinator, and m. orbicularis oculi. 3D reconstruction of the lip muscles should be taken into consideration in order to improve the accuracy and individualization of existing 3D facial soft tissue models. More studies are needed to further develop efficient methods for segmentation in this field. |
Traces
|
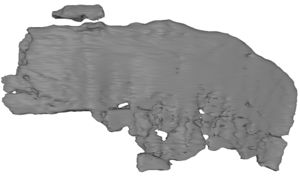
Author: Caitlin Berrigan Assistance: Marianna Jakab, BWH Special Thanks: J. Levi Schmidt (MIT), Tom Lutz (MIT Media Lab), Neil Gershenfeld (MIT Center for Bits & Atoms), Clare Tempany (BWH) Institution: MIT Visual Arts Program, 2010 Jun; Background/Purpose: Traces is a renewable sculpture of the artist’s own disembodied kidney, cast in frozen spit. Every two hours a new frozen organ is put on display, only to melt and drip away. The artist - using 3D Slicer - carefully traced the topography of her internal organ from a 3D MRI, consisting of hundreds of sequential medical images, in order to materialize its form outside of her body. Traces is a poetic deterritorialization of medical biotechnologies, organs without bodies and fleshy displacements. It calls attention to the alienability of body parts and the vast global industry that sustains the promise of an infinitely repairable body. Funding:
|
CLIMB Study (Comprehensive Longitudinal Investigation of Multiple Sclerosis at Brigham and Women’s Hospital) Former NHS Study (The Harvard Multiple Sclerosis Natural History Study)
|
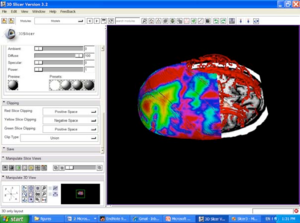
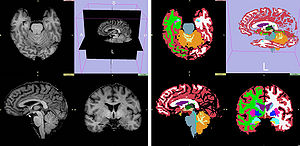
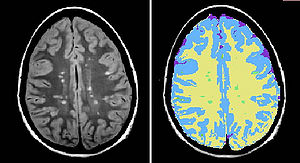
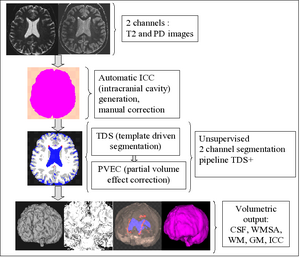
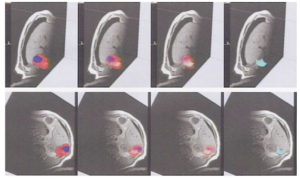
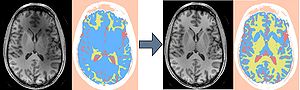
Institution: Multiple Sclerosis Center Background/Purpose: The CLIMB study is a longitudinal natural history study conducted at the Partners Multiple Sclerosis Center. All patients enrolled in the CLIMB undergo a detailed neurological examination at least annually, and have a brain MRI and a blood draw with associated immunological analysis on an annual basis. Within the CLIMB study, the following cohorts of patients are enrolled: relapsing-remitting MS (RRMS) and secondary progressive MS (SPMS), as well as patients with primary progressive MS (PPMS), CIS, and benign MS. Over 30 publications have been generated from CLIMB-related data since its inception. The MRI Analysis Center of the Partners MS Center manages routine MRI processing of all CLIMB study subject MRIs. Routine processing includes calculation of T2 lesion volume and brain parenchymal fraction and number of gadolinium enhancing lesions. Image Workflow system based on Standart Operationg Procedures/Modules in Database system to allow for query from data fields as well as in image space. Several advanced image visualization packages are used for visualization and analysis. These include 3D Slicer, OSIRIX and GDC (in house). 3D Slicer and OSIRIX are open source packages, for which CNI had developed plugins and scripts to streamline workflow. Following processing steps are performed using 3D Slicer software:
|
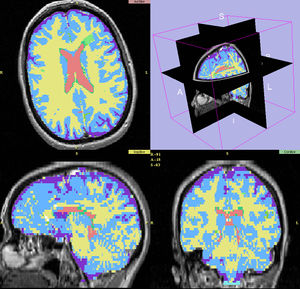 Last step of processing pipeline, segmented label map (green - MS lesions, yellow- WM, blue - GM, Red - ventrical CSF, purple - cortical CSF) displayed in 3D Slicer for expert review along with original grayscale 2D PD and T2 images (source of 2 channel TDS+ segmentation pipeline). Original axial images are reconstructed in 3D to display sagittal and coronal view as well. |
Steroid Adjunctive Treatment at Initiation of Avonex Therapy for Patients with Mono-Symptomatic or Relapsing-Remitting Multiple Sclerosis
|
Principal Investigator: Rohit Bakshi Institution: Laboratory for Neuroimaging Research, Partners MS Center Background/Purpose: We used quantitative MRI parameters such as T2 lesion volume (T2LV) and brain parenchymal fraction (BPF) to assess treatment in patients with MS. T2 lesion volume and BPF were measured using template-driven segmentation (TDS+) algorithm by automated pipeline. Medical image data were visualized with 3D Slicer to provide QC for original data, segmented output and perform manual correction on required steps of processing pipeline. Funding:
|
Age-Related Changes of Cognition in Health and Diseases: Image Analysis Core
|
Principal Investigator: Marilyn S. Albert Institution: Johns Hopkins Alzheimer’s Disease Research Center Background/Purpose: The goal of this project was the utilization of magnetic resonance imaging for morphometric analysis and tissue characterization to distinguish the patterns of brain atrophy and gray or white matter changes and white matter signal abnormalities in normal aging or Alzheimer's disease. Image analysis comprized an automated tissue segmentation into the intracranial cavity (ICC) and subclasses of white matter (WM), gray matter (GM), cerebrospinal fluid (CSF), and WM signal abnormalities (WMSA). Brain parenchymal fraction (BPF) was defined as BPF=(1-CSF)/ICC. Medical image data were visualized by 3D Slicer to provide QC for original grayscale data, segmented output and perform manual correction of ICC. Funding:
|
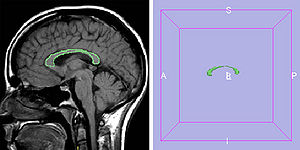 Corpus callosum (CC) measures were obtained from Mid-sagittal T1-weighted MRI scans by manually tracing the outer edge of the corpus callosum on the midsagittal slice using 3D Slicer software. |
Harvard Research Nursing Home Project (MOBILIZE study)
|
Principal Investigator: Lewis A. Lipsitz Institution: Institute for Aging Research (IFAR), Harvard Medica School, Boston, MA, USA. Background/Purpose: The project focuses on abnormal blood pressure regulation and its relationship to the development of falls and syncope in the elderly. 3D Slicer was used to provide visualization during QC step of original data (1.5T and 3T), segmented output and perform manual correction on required steps of processing pipeline as well as corpus callosum outline for parcellation. |
Daclizumab Use in Patients with Pediatric Multiple Sclerosis Failing Interferon
|
Principal Investigator: Tanuja Chitnis Institution: Partners Pediatric MS Center Background/Purpose: We used quantitative MRI parameters such as T2 lesion volume (T2LV) to assess treatment in patients with POMS. The T2-lesion volume of the brain was manually outlined using 3D Slicer. Funding:
|
MRI findings of pediatric-onset Multiple Sclerosis patients: a retrospective study
|
Principal Investigator: Tanuja Chitnis Institution: Partners Pediatric MS Center Background/Purpose: To assess differences in MRI-derived lesion volume and brain parenchymal fraction (BPF) between patients with pediatric- and adult-onset Multiple Sclerosis (MS). T2 lesion volume and BPF were measured using template-driven segmentation (TDS+) algorithm by automated pipeline of the Multiple Sclerosis Database Project. Medical image data were visualized by 3D Slicer to provide QC for original data, segmented output and perform manual correction on required steps of processing pipeline. Funding:
|
Pediatric MS MRI Pilot Project
|
Principal Investigator: Tanuja Chitnis Institution: Partners Pediatric MS Center Background/Purpose: The goal of this project is to assess the characteristics of the pediatric MS patient population and increase education and awareness of this disease subtype. 3D Slicer is used to QC MRI images coming to the multi-center MRI data repository at the Center for Neurological Imaging (CNI) at Brigham and Women’s Hospital. Funding:
|
The Multiple Sclerosis Database Project
|
Institution: Multiple Sclerosis Center Background/Purpose: Project is an initiative to design, develop and implement a database system integrating all aspects of clinical data with medical image data. This image-centric database will enable users to visualize clinical data, including laboratory results, immunologic data, and examination scores, simultaneously with that individual’s MRI images. By integrating the medical images and clinical patient data in a comprehensive system, the efficiency of patient care and data analysis is dramatically improved. This database is another small step towards our ultimate goal: Finding a cure for MS. Image Workflow system based on Standard Operation Procedures/Modules in Database system to allow the day-to-day management and query from data fields to ensure that trial was performed according to SOPs by managing the efforts of MRI research personnel, quality control of data, image analysis and image processing as a part of quantitative pipeline for trial. 3D Slicer advanced image visualization package is used for visualization and analysis MRI data to provide T2 lesion volume and BPF volumetric measurements. |
Effects of Strain Thresholds on Bone Formation in Response to Mechanical Loading
|
Publication: TBA Authors: Thiagarajan G, Johnson M, Dallas M, Lu Y. Institution: University of Missouri-Kansas City, KS, USA. Background/Purpose: It has been hypothesized that osteocytes are stimulated by local strain distribution within the bone subjected to mechanical loadings. In this research project, the mouse forearm model was built which was later used for extensive finite element study. The study will be the first in the field to include the radius in the numerical analysis to examine its effect on the load distribution between the ulna/radius. In order to preserve the geometrical details of the bones, the cavities were traced independently. Then a 3D volume subtraction was performed in another software to produce the exact CAD model of the bone structure. The results of the current research are expected to shed light on how bone perceives mechanical load and the pathway whereby the physical load is transduced into a biochemical event and eventually results in new bone formation. The study will help in developing new treatments for bone diseases such as osteoporosis. Funding:
|
Automated Ventricular Systems Segmentation in Brain CT Images by Combining Low-level Segmentation and High-level Template Matching
|
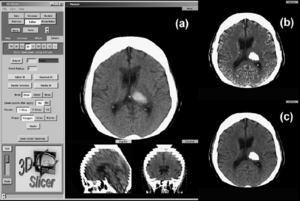
Publication: BMC Med Inform Decis Mak. 2009 Nov 3;9 Suppl 1:S4. PMID: 19891798 | PDF Authors: Chen W, Smith R, Ji SY, Ward KR, Najarian K. Institution: Department of Computer Science, Virginia Commonwealth University, Richmond, VA, USA. Background/Purpose: Accurate analysis of CT brain scans is vital for diagnosis and treatment of Traumatic Brain Injuries (TBI). Automatic processing of these CT brain scans could speed up the decision making process, lower the cost of healthcare, and reduce the chance of human error. In this paper, we focus on automatic processing of CT brain images to segment and identify the ventricular systems. The segmentation of ventricles provides quantitative measures on the changes of ventricles in the brain that form vital diagnosis information. |
 3D ventricle model from 3D Slicer sample visualization. The red parts are ventricular system model. Two symmetrical lateral ventricles on each side in normal case. The lower part in the middle is the third ventricle. The fourth ventricle is the lowest part which is not considered in our paper, but it can be included following the method in this paper. |
MRI-derived Measurements of Human Subcortical, Ventricular and Intracranial Brain Volumes: Reliability Effects of Scan Sessions, Acquisition Sequences, Data Analyses, Scanner Upgrade, Scanner Vendors and Field Strengths
|
Publication: Neuroimage. 2009 May 15;46(1):177-92. PMID: 19233293 | PDF Authors: Jovicich J, Czanner S, Han X, Salat D, van der Kouwe A, Quinn B, Pacheco J, Albert M, Killiany R, Blacker D, Maguire P, Rosas D, Makris N, Gollub R, Dale A, Dickerson BC, Fischl B. Institution: Center for Mind-Brain Sciences, Department of Cognitive and Education Sciences, University of Trento, Italy. Background/Purpose: Automated MRI-derived measurements of in-vivo human brain volumes provide novel insights into normal and abnormal neuroanatomy, but little is known about measurement reliability. Here we assess the impact of image acquisition variables (scan session, MRI sequence, scanner upgrade, vendor and field strengths), FreeSurfer segmentation pre-processing variables (image averaging, B1 field inhomogeneity correction) and segmentation analysis variables (probabilistic atlas) on resultant image segmentation volumes from older (n=15, mean age 69.5) and younger (both n=5, mean ages 34 and 36.5) healthy subjects. The variability between hippocampal, thalamic, caudate, putamen, lateral ventricular and total intracranial volume measures across sessions on the same scanner on different days is less than 4.3% for the older group and less than 2.3% for the younger group. Within-scanner measurements are remarkably reliable across scan sessions, being minimally affected by averaging of multiple acquisitions, B1 correction, acquisition sequence (MPRAGE vs. multi-echo-FLASH), major scanner upgrades (Sonata-Avanto, Trio-TrioTIM), and segmentation atlas (MPRAGE or multi-echo-FLASH). Volume measurements across platforms (Siemens Sonata vs. GE Signa) and field strengths (1.5 T vs. 3 T) result in a volume difference bias but with a comparable variance as that measured within-scanner, implying that multi-site studies may not necessarily require a much larger sample to detect a specific effect. These results suggest that volumes derived from automated segmentation of T1-weighted structural images are reliable measures within the same scanner platform, even after upgrades; however, combining data across platform and across field-strength introduces a bias that should be considered in the design of multi-site studies, such as clinical drug trials. The results derived from the young groups (scanner upgrade effects and B1 inhomogeneity correction effects) should be considered as preliminary and in need for further validation with a larger dataset. Funding:
|
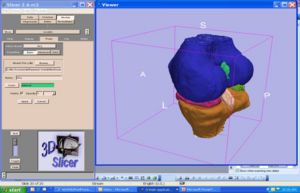
 Sample color-coded subcortical segmentation results (right hemisphere only): hippocampus (yellow), thalamus (green), caudate (light blue), putamen (pink), pallidum (dark blue) and amygdala (turquoise). Top: Freesurfer derived subcortical labels, from a two-averaged MPRAGE in axial (left), coronal (center) and sagittal (right) views. Bottom: 3D surface models created with 3D Slicer derived from the Freesurfer subcortical segmentations. |
Integration of the Vascular Modeling Toolkit in 3D Slicer
|
Publication: Student Research Project 2009 Apr; | PDF Author: Daniel Hähn Institution: Medical Informatics, University of Heidelberg, Germany. Background/Purpose: The extraction of vessels in two- and three-dimensional images is part of many clinical analysis tasks. Surgical and radiology procedures often involve the visualization and quantification of vessels in order to perform surgical planning or diagnostics. There is no single segmentation method that can extract vessels from every medical image modality, but different approaches and robust algorithms exist. Various published key algorithms are available within an open-source framework for image-based modeling of blood vessels, referred to as the Vascular Modeling Toolkit (VMTK). The library of VMTK was made available in 3D Slicer, an application providing a wide range of tools for medical image processing. This was realized using a hidden loadable module approach in order to provide a flexible way of distributing and including the library. To evaluate and verify the integration, a software module offering VMTK level set segmentation methods within 3D Slicer was created. With the successful connection of the two above mentioned software solutions, processing pipelines between VMTK code and other algorithms can be established. Several techniques for three dimensional reconstruction, geometric analysis, mesh generation and surface data analysis for image-based modeling of blood vessels are now accessible to the 3D Slicer developer. The reference implementation for accessing VMTK, as well as the created library module are available as open-source software. Funding:
|
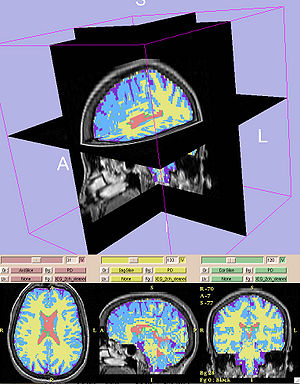
New EMSegment Module in Slicer3
|
Publication: Insight Journal, Sep 15, 2009. Authors: Rannou N, Jaume S, Pieper S, Kikinis R. Institution: ISEN Brest, France. Background/Purpose: Many neuroanatomy studies rely on brain tissue segmentation in Magnetic Resonance images (MRI). The Expectation-Maximization (EM) theory offers a popular framework for this task. We studied the EM algorithm developed at the Surgical Planning Laboratory (SPL) at Harvard Medical School and implemented in the 3D Slicer software. We observed that the segmentation lacks accuracy if the image exhibits some intensity inhomogeneity. Moreover the optimum parameters are challenging to estimate. This document aims at describing our solutions within the context of statistical modeling. Our contributions range from algorithm improvements to novel representations of the statistical distribution model. First we added a bias field correction module and exposed the most significant parameters. Second we proposed a new way to select the distribution of the tissues to be segmented. Finally we designed a set of interactive tools to make the segmentation process easier and more accurate. To validate the new segmentation pipeline, we performed our experiments on MRI data and a clinical expert evaluated our results. Funding:
|
 New EMSegment Module in Slicer3. We improved the usability of EMSegment in a clinical setting and studied the influence of MRI Bias Field Correction on the segmentation accuracy. |
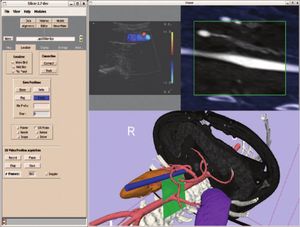
|
Publication: The International Journal of Virtual Reality, 2009, 8(1):9-16. | PDF Authors: Tran HH, Matsumiya K, Masamune K, Sakuma I, Dohi T, Liao H. Institution: Graduate School of Information Science and Technology, University of Tokyo, Tokyo, Japan. Background/Purpose: In this paper, we mainly focus on a high-speed IV rendering method that allows interactions to be done in almost real-time, while maintaining the rendered result at an acceptable quality. We also built a navigation system based on the open source software, 3D Slicer, so that many tasks can be done in a single application. Funding:
|
Smaller Amygdala is Associated with Anxiety in Patients with Panic Disorder
|
Publication: Psychiatry and Clinical Neurosciences 2009; 63:266-76. PMID: 19566756 | PDF Authors: Hayano F, Nakamura M, Asami T, Uehara K, Yoshida T, Roppongi T, Otsuka T, Inoue T, Hirayasu Y. Institution: Department of Psychiatry, Yokohama City University, Yokohama, Kanagawa, Japan. Background/Purpose: Anxiety a core feature of panic disorder, is linked to function of the amygdala. Volume alterations in the brain of patients with panic disorder have previously been reported, but there has been no report of amygdala volume association with anxiety. Methods: Volumes of hippocampus and amygdala were manually measured using magnetic resonance imaging obtained from 27 patients with panic disorder and 30 healthy comparison subjects. In addition the amygdala was focused on, applying small volume correction to optimized voxel-based morphometry (VBM). State-Trait Anxiety Inventory and the NEO Personality Inventory Revised were also used to evaluate anxiety. Amygdala volumes in both hemispheres were significantly smaller in patients with panic disorder compared with control subjects (left: t = -2.248, d.f. = 55, P = 0.029; right: t = -2.892, d.f. = 55, P = 0.005). VBM showed that structural alteration in the panic disorder group occurred on the corticomedial nuclear group within the right amygdala (coordinates [x,y,z (mm)]: [26,-6,-16], Z score = 3.92, family-wise error-corrected P = 0.002). The state anxiety was negatively correlated with the left amygdala volume in patients with panic disorder (r = -0.545, P = 0.016). These findings suggested that the smaller volume of the amygdala may be associated with anxiety in panic disorder. Of note, the smaller subregion in the amygdala estimated on VBM could correspond to the corticomedial nuclear group including the central nucleus, which may play a crucial role in panic attack. Funding:
|
 Voxels with a significant decrease in region of amygdala area among panic disorder (PD) patients compared with healthy control (HC) subjects. (a) statistical parametric map showing significantly smaller subregion within the amygdala. (b) The same statistical parametric map overlayed on a structural volume. |
Optimal Transseptal Puncture Location for Robot-assisted Left Atrial Catheter Ablation
|
Publication: Int Conf Med Image Comput Comput Assist Interv. 2009;12(Pt 1): 1-8. PMID: 20425964 | PDF Authors: Jayender J, Patel RV, Michaud GF, Hatal N. Institution: Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA.
Funding:
|
 The result of the GII algorithm displayed as a color map on the septal wall. The color blue represents the GII with highest value, which correspond to the optimal port, while red represents a low value of GII. Discrete points on the septal wall which provide the maximum maneuverability of the catheter within the left atrium. |
Measurements from Image-based Three Dimensional Pelvic Floor Reconstruction: A Study of Inter- and Intraobserver Reliability
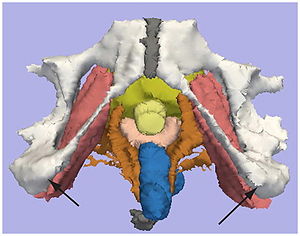
|
Publication: J Magn Reson Imaging. 2009 Aug;30(2):344-50. PMID: 19629987 | PDF Authors: Hoyte L, Brubaker L, Fielding JR, Lockhart ME, Heilbrun ME, Salomon CG, Ye W, Brown MB; Pelvic Floor Disorders Network. Institution: University of South Florida, College of Medicine, Division of Urogynecology and Pelvic Reconstructive Surgery, Tampa General Hospital, Urogynecology Division, Tampa, FL, USA. Background/Purpose: To describe inter- and intraobserver reliability of 3D measurements of female pelvic floor structures. Twenty reconstructed MR datasets of primiparas at 6-12 months postpartum were analyzed. Pelvic organ measurements were independently made twice by three radiologists blinded to dataset order. A "within-reader" analysis, a "between-reader" analysis, and the intraclass correlation (ICC), and standard deviation ratio (SDR) were computed for each parameter. Fifteen continuous variables and one categorical variable were measured. Eight continuous parameters showed excellent agreement (ICC >0.85 / SDR <0.40), five parameters showed relatively good agreement (ICC >0.70 / SDR >or=0.40, <0.60). Two parameters showed poor agreement (ICC <or=0.70 and/or SDR >or=0.60). The categorical variable showed poor agreement. Agreement was best where landmark edges were well defined, acceptable where more "reader judgment" was needed, and poor where levator defects made landmarks difficult to identify. Automated measurement algorithms are under study and may improve agreement in the future. Funding:
|
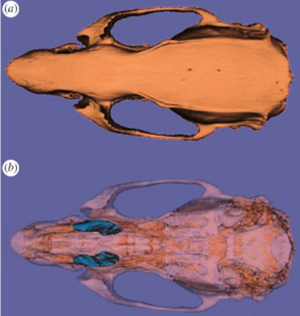
Three-dimensional Analysis of Rodent Paranasal Sinus Cavities from X-ray Computed Tomography (CT) Scans
|
Publication: Can J Vet Res. 2009 Jul;73(3):205-11. PMID: 19794893 | PDF Authors: Phillips JE, Ji L, Rivelli MA, Chapman RW, Corboz MR. Institution: Pulmonary and Peripheral Neurobiology, Schering-Plough Research Institute, Kenilworth, NJ, USA. Background/Purpose: Continuous isometric microfocal X-ray computed tomography (CT) scans were acquired from an AKR/J mouse, Brown-Norway rat, and Hartley guinea pig. The anatomy and volume of the paranasal sinus cavities were defined from 2-dimensional (2-D) and 3-dimensional (3-D) CT images. Realistic 3-D images were reconstructed and used to determine the anterior maxillary, posterior maxillary, and ethmoid sinus cavity airspace volumes (mouse: 0.6, 0.7, and 0.7 mm3, rat: 8.6, 7.7, and 7.0 mm3, guinea pig: 63.5, 46.6 mm3, and no ethmoid cavity, respectively). The mouse paranasal sinus cavities are similar to the corresponding rat cavities, with a reduction in size, while the corresponding maxillary sinus cavities in the guinea pig are different in size, location, and architecture. Also, the ethmoid sinus cavity is connected by a common drainage pathway to the posterior maxillary sinus in mouse and rat while a similar ethmoid sinus was not present in the guinea pig. We conclude that paranasal sinus cavity airspace opacity (2-D) or volume (3-D) determined by micro-CT scanning may be used to conduct longitudinal studies on the patency of the maxillary sinus cavities of rodents. This represents a potentially useful endpoint for developing and testing drugs in a small animal model of sinusitis. Funding:
|
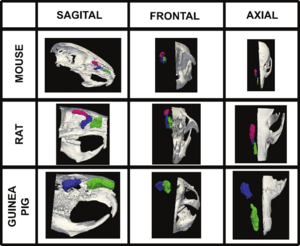 Volumetric surface renderings of paranasal sinus created from sequential computed tomography (CT) images. Three different orientations of the paranasal sinuses (anterior maxillary in green, posterior maxillary in blue, and anterior ethmoid in red) are shown with respect to location in skull according to species, all at different magnifications. |
Multimodal Imaging in Mild Cognitive Impairment: Metabolism, Morphometry and Diffusion of the Temporal–parietal Memory Network
|
Publication: Neuroimage. 2009 Mar 1;45(1):215-23. PMID: 19056499 | PDF Authors: Walhovd KB, Fjell AM, Amlien I, Grambaite R, Stenset V, Bjørnerud A, Reinvang I, Gjerstad L, Cappelen T, Due-Tønnessen P, Fladby T. Institution: Center for the Study of Human Cognition, Department of Psychology, University of Oslo, Norway. Background/Purpose: This study compared sensitivity of FDG-PET, MR morphometry, and diffusion tensor imaging (DTI) derived fractional anisotropy (FA) measures to diagnosis and memory function in mild cognitive impairment (MCI). Patients (n = 44) and normal controls (NC, n = 22) underwent FDG-PET and MRI scanning yielding measures of metabolism, morphometry and FA in nine temporal and parietal areas affected by Alzheimer's disease and involved in the episodic memory network. Patients also underwent memory testing (RAVLT). Logistic regression analysis yielded 100% diagnostic accuracy when all methods and ROIs were combined, but none of the variables then served as unique predictors. Within separate ROIs, diagnostic accuracy for the methods combined ranged from 65.6% (parahippocampal gyrus) to 73.4 (inferior parietal cortex). Morphometry predicted diagnostic group for most ROIs. PET and FA did not uniquely predict group, but a trend was seen for the precuneus metabolism. For the MCI group, stepwise regression analyses predicting memory scores were performed with the same methods and ROIs. Hippocampal volume and FA of the retrosplenial WM predicted learning, and hippocampal metabolism and parahippocampal cortical thickness predicted 5 minute recall. No variable predicted 30 minute recall independently of learning. In conclusion, higher diagnostic accuracy was achieved when multiple methods and ROIs were combined, but morphometry showed superior diagnostic sensitivity. Metabolism, morphometry and FA all uniquely explained memory performance, making a multi-modal approach superior. Memory variation in MCI is likely related to conversion risk, and the results indicate potential for improved predictive power by the use of multimodal imaging. Funding:
|
 Illustrations of the main steps in the multi-modal image analysis. (A and B) The brain surface is parcellated into 34 different regions in each hemisphere (B), and a newly developed algorithm assigns a label to each underlying WM voxel (A). (C) Five cortical ROI's and hippocampus, of much importance in the episodic memory network, were chosen for analyses in the present paper. EC — entorhinal cortex; PH — parahippocampal cortex; RC — retrosplenial cortex; PC — posterior cingulate; Pre — precuneus. (D) Every voxel in each brain volume is assigned a label based on the cortical parcellations (A), the WM parcellations (B), and the whole-brain segmentation. The distance between the red and the yellow line is the cerebral cortex. (E) The FA volume is registered to the anatomical volume, and mean FA is calculated from the voxels included in each WM ROI (A). (F) FDG-PET data are also registered to the anatomical volume, and the metabolism is divided by the metabolism in the brainstem. Mean metabolism in each cortical ROI and hippocampus is calculated. (G) The whole-brain segmentation yields hippocampal volume (hippocampus is marked in yellow, indicated by the red arrows). A three-dimensional rendering of hippocampus is shown to illustrate the result of the segmentation. |
The Relation between Connection Length and Degree of Connectivity in Young Adults: A DTI Analysis
|
Publication: Cereb Cortex. 2009 Mar;19(3):554-62. PMID: 18552356 | PDF Authors: Lewis JD, Theilmann RJ, Sereno MI, Townsend J. Institution: Department of Cognitive Science, University of California-San Diego, La Jolla, CA, USA. Background/Purpose: Using diffusion tensor imaging and tractography to detail the patterns of interhemispheric connectivity and to determine the length of the connections, and formulae based on histological results to estimate degree of connectivity, we show that connection length is negatively correlated with degree of connectivity in the normal adult brain. The degree of interhemispheric connectivity - the ratio of interhemispheric connections to total corticocortical projection neurons - was estimated for each of 5 subregions of the corpus callosum in 22 normal males between 20 and 45 years of age (mean 31.68; standard deviation 8.75), and the average length of the longest tracts passing through each point of each subregion was calculated. Regression analyses were used to assess the relation between connection length and the degree of connectivity. Connection length was negatively correlated with degree of connectivity in all 5 subregions, and the regression was significant in 4 of the 5, with an average r(2) of 0.255. This is contrasted with previous analyses of the relation between brain size and connectivity, and connection length is shown to be a superior predictor. The results support the hypothesis that cortical networks are optimized to reduce conduction delays and cellular costs. Funding:
|
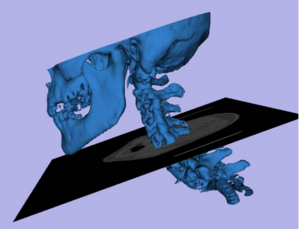
The ROBOCAST Project: ROBOt and Sensors Integration for Computer Assisted Surgery and Therapy
|
Authors: Shamir RR, Joskowicz L, Ferrigno G. Institution: School of Engineering and Computer Science, The Hebrew University of Jerusalem, Israel. Background/Purpose: The goal of the European FP7 ROBOCAST project is to develop a system for keyhole neurosurgery. ROBOCAST integrates optical and electromagnetic localization devices with two modified commercial surgical robots: 1. PathFinder (Prosurgics Ltd, UK), which is used for gross positioning, and; 2. MARS (Mazor Surgical Technologies Ltd, Israel), which is used for fine positioning. A third snake-like robot, currently under development, will be attached to the MARS robot and is intended for curved paths. The system includes as well a haptic device, a tracked ultrasound probe and a micro Doppler ultrasound probe. This sensor and actuation redundancy is expected to yield higher accuracy and robustness, to significantly increase the patient safvety, and to allow new procedures. The ROBOCAST software is based on 3D Slicer 3.4 and uses many of its functions. Funding:
|
A Trajectory Planning Method for Reduced Patient Risk in Image-guided Neurosurgery: Preliminary Results
|
Authors: Shamir RR, Roth R, Joskowicz L, Antiga L, Foroni RI, Shoshan Y. Institution: School of Engineering and Computer Science, The Hebrew University of Jerusalem, Israel. Background/Purpose: We present a new preoperative planning method to better assess and reduce the risk caused by a misplacement of surgical tools in image-guided keyhole neurosurgery. The goal is to quantify the risk of a proposed straight trajectory and to find the trajectory with the lowest risk to hit nearby brain structures based on pre-operative CT/MRI images and their segmentation. First, distance maps are computed on the segmented data such that each voxel on the preoperative CT/MRI image is associated with a vector of distances to each of the segmented structures. A risk volume is then created from the distance maps such that a risk ratio is computed based on the vector of distances associated with each voxel. Next, the risk for each possible trajectory is computed such that the risk along a trajectory is assigned with the maximal risk ratio of intersected voxels. The trajectory that is associated with the lowest risk is presented using 3D Slicer v.3.2 to the neurosurgeon for further revision. The neurosurgeon can revise the suggested trajectory and can add new paths using interactive 3D visualization and quantitative risk assessment. The interactive 3D visualization shows the segmented structures to be avoided along with a geometric structure that envelopes the defined trajectory and represents the localization uncertainty. In addition, candidate entry points are represented by the outer head surface that is extracted automatically from the patient’s preoperative image and the neurosurgeon can select parts of the surface to restrict the optional entry points. A table, called ‘risk card’, of quantitative measures regarding the risk that is associated with the defined trajectory is presented. It shows the neurosurgeon meaningful geometrical information, including the path length and distance of segmented structures to the path. For the initial validation, we have compared the conventional approach for trajectory planning with our method on 8 targets selected at various locations on a clinical Magnetic Resonance Angiography (MRA) head image. For each target, the user selected two trajectories: one with the conventional method based on the axial, sagittal, and coronal 2D views of the original MRA image, and the second with our method. Our preliminary results show a significant reduction in trajectory risk and planning time when compared to the conventional method. Funding:
|
Contrast-maximizing Adaptive Region Growing for CT
|
Publication: Poster Presentation at the Second International Workshop on Pulmonary Image Analysis. | Poster, Paper. Oral Presentation at Advanced Concepts for Intelligent Vision Systems, ACIVS 2009. Authors: Mendoza CS, Acha B, Serrano C. Institution: Signal Processing Department, University of Sevilla, Spain. Background/Purpose: We have developed a general segmentation framework based on a contrast-based self-assessed region growing strategy. Thanks to a previous normalization stage, a wide variety of CT imaging conditions are supported, requiring limited user intervention. Although multiple seeds are accepted for performance boosting, only a single-seed selection stage is required for most of our application specific tissues. The detection of the optimal parameters is managed internally using a measure of the varying contrast of the growing region. Validation is provided for some synthetic images, and also for real CT images. Results have been obtained in the context of surgical planning (bone, muscle and fat segmentation) and pulmonary image analysis (airway segmentation). Funding:
|
Computer-aided 3D Visualization in Oto-rhino-laryngology
|
Publication: Poster Presentation at the 80th Conference of the German ENT Society. | PDF Authors: Nagy AL, Tanács A, Czesznak A, Smehák Gy, Tóth F, Rovó L, Jóri J, Kiss JG. Institution: Department of Oto-rhino-laryngology and Head, Neck Surgery, University of Szeged, Hungary. Background/Purpose: Most of the CT and MR data is stored nowadays on digital media. This opens up new possibilities for us to inspect these data. In our department we evaluated the use of the 3D Slicer software, a free, open source and is being actively developed. In oto-rhino-laryngology we often encounter situations where the exact localization and estimation of the size of a lesion, or tumor is of critical importance. Especially in the neck and the facial region an extended resection may easily cause damage to the function of the affected organ. The preservation of the swallowing function in case of the neck, and the preservation of sight in interventions around the orbita are two of these areas. By visualizing these space-occupying lesions we were able to plan and carry out the surgery more precisely. |
Clinical Application of Curvilinear Distraction Osteogenesis for Correction of Mandibular Deformities
|
Publication: J Oral Maxillofac Surg. 2009 May;67(5):996-1008. PMID: 19375009 | PDF Authors: Kaban LB, Seldin EB, Kikinis R, Yeshwant K, Padwa BL, Troulis MJ. Institution: Department of Oral and Maxillofacial Surgery, Massachusetts General Hospital, Harvard School of Dental Medicine, Boston, MA, USA. Background/Purpose: To report the use of a semiburied curvilinear distraction device, with a 3-dimensional (3D) computed tomography treatment planning system, for correction of mandibular deformities. This was a retrospective evaluation of 13 consecutive patients, with syndromic and nonsyndromic micrognathia, who underwent correction by curvilinear distraction osteogenesis. A 3D computed tomography scan was obtained for each patient and imported into a 3D treatment planning system (Slicer/Osteoplan). Surgical guides were constructed to localize the osteotomy and to drill holes to secure the distractor's proximal and distal footplates to the mandible. Postoperatively, patients were followed by clinical examination and plain radiographs to ensure the desired vector of movement. At end distraction, when possible, a 3D computed tomography scan was obtained to document the final mandibular position. Of the 13 patients, 8 were females and 5 were males, with a mean age of 11.9 years (range 15 months to 39 years). All 13 underwent bilateral mandibular curvilinear distraction. Of the 13 patients, 8 were 16 years old or younger and 5 were younger than 6 years of age. The diagnoses included Treacher Collins syndrome (n = 3), Nager syndrome (n = 3), craniofacial microsomia (n = 2), post-traumatic ankylosis (n = 1), and micrognathia (syndromic, n = 3; nonsyndromic, n = 1). The correct distractor placement, vector of movement, and final mandibular position were achieved in 10 of 13 patients. In the other 3 patients, the desired jaw position was achieved by "molding" the regenerate. The use of a semiburied curvilinear distraction device, with 3D treatment planning, is a potentially powerful tool to correct complex mandibular deformities. Funding:
|
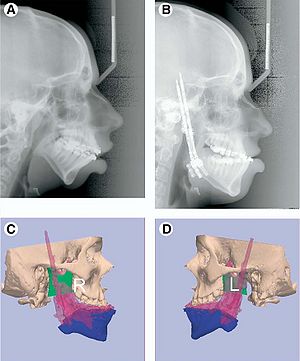 A, Preoperative and B, end-distraction lateral cephalograms. (Patient in Fig 4.) Posterior airway space increased from 5.03 to 18.96 mm and distance from hyoid to mandible decreased from 19.3 to 12.9 mm (normal values 11 mm and Ͻ15 mm, respectively). Overlay of predicted (blue) and end-fixation (pink) position of C, right and D, left sides of mandible demonstrating desired movement was achieved. |
In Vivo Hippocampal Measurement and Memory: A Comparison of Manual Tracing and Automated Segmentation in a Large Community-Based Sample
|
Publication: PLoS One. 2009 Apr; 4(4):e5265. PMID: 19370155 | PDF Authors: Cherbuin N, Anstey KJ, Réglade-Meslin C, Sachdev PS. Institution: Centre for Mental Health Research, Australian National University, Canberra, Australia. Background/Purpose: Each segmented volume was inspected by producing a 3D model using the 3D Slicer software package and its quality rated: a) no or minor defects (estimated to be smaller than ,0.5% of total volume) b) moderate defects (,0.5-5% of total volume), major defects (greater than 5% of total volume). Exemplars are given in Figure 1. Funding:
|
How Volumetric Analysis Quantifies Therapeutic Response of Slow-flow Vascular Malformations
|
Publication: ECR Today 2009 Mar 9. | PDF Authors: Dobrocky T, Kubiena H, Kikinis R, Kettenbach J. Institution: Medical University of Vienna, Austria. Background/Purpose: Slow-flow vascular malformations, such as venous and lymphatic lesions, are most often recognized in infancy and are thus characterized by a rapid expansion. The majority of these lesions are found in the head and neck region, where many options for treatment modalities (drug therapy, percutaneous sclerotherapy, surgical resection) have been reported in the literature. In many cases, excellent results have been achieved by ultrasound-guided or fluoroscopy-guided percutaneous sclerotherapy, sometimes combined with final surgical resection (see figure). Diagnostic MRI of vascular malformations allows non-invasive treatment planning and follow-up, with excellent soft-tissue contrast. |
A Minimally Invasive Registration Method using Surface Template-assisted Marker Positioning (STAMP) for Image-guided Otologic Surgery
|
Publication: Otolaryngol Head Neck Surg. 2009 Jan;140(1):96-102. PMID: 19130970 | PDF Authors: Matsumoto N, Hong J, Hashizume M, Komune S. Institution: Department of Otorhinolaryngology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan. Background/Purpose: A new, minimally invasive registration method was developed for image-guided otologic surgery. We utilized laser-sintered template of the patient's bone surface to transfer the virtual markers to the patient's bone intraoperatively and eliminated the necessity for preoperative marker positioning or additional CT scan. Simulation surgeries and clinical application. We measured registration errors in 10 trials using replicas and six ear surgeries (two cochlear implant insertions, four translabyrinthine acoustic tumor removals). The target registration errors varied among the surgical targets. Errors were less than 1 mm near the cochlear implant insertion target both in phantom study and in actual surgeries. Our newly developed method reduced the preoperative procedures for patients but did not reduce the accuracy in cochlear implant surgery. Our method would be a useful image-guided surgery method in the field of otology, where both accuracy and noninvasiveness are required. Funding:
|
 The IGS screen during surgery. (A) The navigation view of the surgery during cochleostomy. Red, facial nerve; light green, semicircular canals; orange, cochlea; green, drill. (B) The navigation view of the surgery during translabyrinthine approach to the internal auditory canal. The surgeon is now pointing to target “SA” of Table 2. Red, facial nerve; orange, semicircular canals; light green, internal auditory canal; pink, sigmoid sinus and jugular bulb; green, drill with 10-mm extension marks. |
Diffusion Tractography of the Fornix in Schizophrenia
|
Publication: Schizophr Res. 2009 Jan;107(1):39-46. PMID: 19046624 | PDF Authors: Fitzsimmons J, Kubicki M, Smith K, Bushell G, Estepar RS, Westin CF, Nestor PG, Niznikiewicz MA, Kikinis R, McCarley RW, Shenton ME. Institution: Psychiatry Neuroimaging Laboratory, Department of Psychiatry, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: White matter fiber tracts, especially those interconnecting the frontal and temporal lobes, are likely implicated in pathophysiology of schizophrenia. Very few studies, however, have focused on the fornix, a compact bundle of white matter fibers, projecting from the hippocampus to the septum, anterior nucleus of the thalamus and the mamillary bodies. Diffusion Tensor Imaging (DTI), and a new post-processing method, fiber tractography, provides a unique opportunity to visualize and to quantify entire trajectories of fiber bundles, such as the fornix, in vivo. We applied these techniques to quantify fornix diffusion anisotropy in schizophrenia. DTI images were used to evaluate the left and the right fornix in 36 male patients diagnosed with chronic schizophrenia and 35 male healthy individuals, group matched on age, parental socioeconomic status, and handedness. Regions of interest were drawn manually, blind to group membership, to guide tractography, and fractional anisotropy (FA), a measure of fiber integrity, was calculated and averaged over the entire tract for each subject. The Doors and People test (DPT) was used to evaluate visual and verbal memory, combined recall and combined recognition. Analysis of variance was performed and findings demonstrated a difference between patients with schizophrenia and controls for fornix FA (p=0.006). Protected post-hoc independent sample t-tests demonstrated a bilateral FA decrease in schizophrenia, compared with control subjects (left side: p=0.048; right side p=0.006). Higher fornix FA was statistically significantly correlated with DPT and measures of combined visual memory (r=0.554, p=0.026), combined verbal memory (r=0.647, p=0.007), combined recall (r=0.516, p=0.041), and combined recognition (r=0.710, p=0.002) for the control group. No such statistically significant correlations were found in the patient group. Our findings show the utility of applying DTI and tractography to study white matter fiber tracts in vivo in schizophrenia. Specifically, we observed a bilateral disruption in fornix integrity in schizophrenia, thus broadening our understanding of the pathophysiology of this disease. Funding:
|
Spiny Versus Stubby: 3D Reconstruction of Human Myenteric (type I) Neurons
|
Publication: Histochem Cell Biol. 2009 Jan;131(1):1-12. PMID: 18807064 | PDF Authors: Lindig TM, Kumar V, Kikinis R, Pieper S, Schrödl F, Neuhuber WL, Brehmer A. Institution: Department of Anatomy I, University of Erlangen-Nuremberg, Erlangen, Germany. Background/Purpose: We have compared the three-dimensional (3D) morphology of stubby and spiny neurons derived from the human small intestine. After immunohistochemical triple staining for leu-enkephalin (ENK), vasoactive intestinal peptide (VIP) and neurofilament (NF), neurons were selected and scanned based on their immunoreactivity, whether ENK (stubby) or VIP (spiny). For the 3D reconstruction, we focused on confocal data pre-processing with intensity drop correction, non-blind deconvolution, an additional compression procedure in z-direction, and optimizing segmentation reliability. 3D Slicer software enabled a semi-automated segmentation based on an objective threshold (interrater and intrarater reliability, both 0.99). We found that most dendrites of stubby neurons emerged only from the somal circumference, whereas in spiny neurons, they also emerged from the luminal somal surface. In most neurons, the nucleus was positioned abluminally in its soma. The volumes of spiny neurons were significantly larger than those of stubby neurons (total mean of stubbies 806±128 μm3, of spinies 2,316±545 μm3), and spiny neurons had more dendrites (26.3 vs. 11.3). The ratios of somal versus dendritic volumes were 1:1.2 in spiny and 1:0.3 in stubby neurons. In conclusion, 3D reconstruction revealed new differences between stubby and spiny neurons and allowed estimations of volumetric data of these neuron populations. Funding:
|
2008
|
Publication: Int J Med Robot. 2008 Dec;4(4):321-30. PMID: 18803337 | PDF Authors: Xia T, Baird C, Jallo G, Hayes K, Nakajima N, Hata N, Kazanzides P. Institution: Department of Computer Science, Johns Hopkins University, Baltimore, MD, USA. Background/Purpose: We developed an image-guided robot system to provide mechanical assistance for skull base drilling, which is performed to gain access for some neurosurgical interventions, such as tumor resection. The motivation for introducing this robot was to improve safety by preventing the surgeon from accidentally damaging critical neurovascular structures during the drilling procedure. We integrated a Stealthstation((R)) navigation system, a NeuroMate((R)) robotic arm with a six-degree-of-freedom force sensor, and the 3D Slicer visualization software to allow the robotic arm to be used in a navigated, cooperatively-controlled fashion by the surgeon. We employed virtual fixtures to constrain the motion of the robot-held cutting tool, so that it remained in the safe zone that was defined on a preoperative CT scan. We performed experiments on both foam skull and cadaver heads. The results for foam blocks cut using different registrations yielded an average placement error of 0.6 mm and an average dimensional error of 0.6 mm. We drilled the posterior porus acusticus in three cadaver heads and concluded that the robot-assisted procedure is clinically feasible and provides some ergonomic benefits, such as stabilizing the drill. We obtained postoperative CT scans of the cadaver heads to assess the accuracy and found that some bone outside the virtual fixture boundary was cut. The typical overcut was 1-2 mm, with a maximum overcut of about 3 mm. The image-guided cooperatively-controlled robot system can improve the safety and ergonomics of skull base drilling by stabilizing the drill and enforcing virtual fixtures to protect critical neurovascular structures. The next step is to improve the accuracy so that the overcut can be reduced to a more clinically acceptable value of about 1 mm. Funding:
|
The Relationship between Diffusion Tensor Imaging and Volumetry as Measures of White Matter Properties
|
Publication: Neuroimage. 2008 Oct 1;42(4):1654-68. PMID: 18620064 | PDF Authors: Fjell AM, Westlye LT, Greve DN, Fischl B, Benner T, van der Kouwe AJ, Salat D, Bjørnerud A, Due-Tønnessen P, Walhovd KB. Institution: Center for the Study of Human Cognition, Department of Psychology, University of Oslo, Norway. Background/Purpose: There is still limited knowledge about the relationship between different structural brain parameters, despite huge progress in analysis of neuroimaging data. The aim of the present study was to test the relationship between fractional anisotropy (FA) from diffusion tensor imaging (DTI) and regional white matter (WM) volume. As WM volume has been shown to develop until middle age, the focus was on changes in WM properties in the age range of 40 to 60 years. 100 participants were scanned with magnetic resonance imaging (MRI). Each hemisphere was parcellated into 35 WM regions, and volume, FA, axial, and radial diffusion in each region were calculated. The relationships between age and the regional measures of FA and WM volume were tested, and then FA and WM volume were correlated, corrected for intracranial volume, age, and sex. WM volume was weakly related to age, while FA correlated negatively with age in 26 of 70 regions, caused by a mix of reduced axial and increased radial diffusion with age. 23 relationships between FA and WM volume were found, with seven being positive and sixteen negative. The positive correlations were mainly caused by increased radial diffusion. It is concluded that FA is more sensitive than volume to changes in WM integrity during middle age, and that FA-age correlations probably are related to reduced amount of myelin with increasing age. Further, FA and WM volume are moderately to weakly related and to a large extent sensitive to different characteristics of WM integrity. Funding:
|
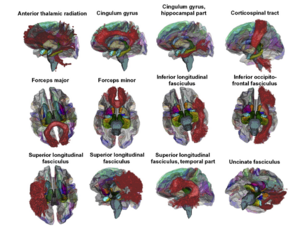 3D renderings of the probabilistic tracts overlaid on a transparent template brain with the FreeSurfer WM parcellations and whole-brain segmentation. The 11 atlas-based probabilistic tracts from the Mori atlas is shown as 3D renderings, displayed on a semi-transparent template brain from FreeSurfer (fsaverage). The subcortical structures are results from FreeSurfer's whole brain segmentation procedure. The colors on the cortical surface are the cortical parcellations on which the WM parcellations are based (see Figs. 1 and 2). The figure was made by use of 3D Slicer software. |
3D Modeling-based Surgical Planning in Transsphenoidal Pituitary Surgery - Preliminary Results
|
Publication: Acta Otolaryngol. 2008 Sep;128(9):1011-8. PMID: 19086197 Authors: Raappana A, Koivukangas J, Pirilä T. Institution: Department of Otorhinolaryngology, Head and Neck Surgery, Oulu University Hospital, Oulu, Finland. Background/Purpose: The preoperative three-dimensional (3D) modeling of the pituitary adenoma together with pituitary gland, optic nerves, carotid arteries, and the sphenoid sinuses was adopted for routine use in our institution for all pituitary surgery patients. It gave the surgeon a more profound orientation to the individual surgical field compared with the use of conventional 2D images only. To demonstrate the feasibility of 3D surgical planning for pituitary adenoma surgery using readily available resources. The computed tomography (CT) and magnetic resonance imaging (MRI) data of 40 consecutive patients with pituitary adenoma were used to construct 3D models to be used in preoperative planning and during the surgery. 3D Slicer, a free, open source program downloaded to a conventional personal computer (PC) was applied. The authors present a brief description of the 3D reconstruction-based surgical planning workflow. In addition to the preoperative planning the 3D model was used as a 'road map' during the operation. With the 3D model the surgeon was more confident when opening the sellar wall and when evacuating the tumor from areas in contact with vital structures than when using only conventional 2D images. |
A Generic Framework for Internet-based Interactive Applications of High-resolution 3-D Medical Image Data
|
Publication: IEEE Trans Inf Technol Biomed. 2008 Sep;12(5):618-26. PMID: 18779076 Authors: Liu D, Hua KA, Sugaya K. Institution: School of Electrical Engineering and Computer Science, University of Central Florida, Orlando, FL, USA. Background/Purpose: With the advances in medical imaging devices, large volumes of high-resolution 3-D medical image data have been produced. These high-resolution 3-D data are very large in size, and severely stress storage systems and networks. Most existing Internet-based 3-D medical image interactive applications therefore deal with only low- or medium-resolution image data. While it is possible to download the whole 3-D high-resolution image data from the server and perform the image visualization and analysis at the client site, such an alternative is infeasible when the high-resolution data are very large, and many users concurrently access the server. In this paper, we propose a novel framework for Internet-based interactive applications of high-resolution 3-D medical image data. Specifically, we first partition the whole 3-D data into buckets, remove the duplicate buckets, and then, compress each bucket separately. We also propose an index structure for these buckets to efficiently support typical queries such as 3D Slicer and region of interest, and only the relevant buckets are transmitted instead of the whole high-resolution 3D medical image data. Furthermore, in order to better support concurrent accesses and to improve the average response time, we also propose techniques for efficient query processing, incremental transmission, and client sharing. Our experimental study in simulated and realistic environments indicates that the proposed framework can significantly reduce storage and communication requirements, and can enable real-time interaction with remote high-resolution 3-D medical image data for many concurrent users. |
Anterior Cingulate Cortex Volume Reduction in Patients with Panic Disorder
|
Publication: Psychiatry Clin Neurosci. 2008 Jun;62(3):322-30. PMID: 18588593 | PDF Authors: Asami T, Hayano F, Nakamura M, Yamasue H, Uehara K, Otsuka T, Roppongi T, Nihashi N, Inoue T, Hirayasu Y. Institution: Department of Psychiatry, Yokohama City University School of Medicine, Yokohama, Japan. Background/Purpose: Recent neuroimaging studies have suggested that the anterior cingulate cortex (ACC) has an important role in the pathology of panic disorder. Despite numerous functional neuroimaging studies that have elucidated the strong relationship between functional abnormalities of the ACC and panic disorder and its symptoms and response to emotional tasks associated with panic disorder, there has been no study showing volumetric changes of the ACC or its subregions. To clarify the structural abnormalities of ACC and its subregions, the combination of region of interest (ROI) and optimized voxel-based morphometry (VBM) methods were performed on 26 patients with panic disorder, and 26 age and sex-matched healthy subjects. In the ROI study, ACC was divided into four subregions: dorsal, rostral, subcallosal and subgenual ACC. The results of the manually traced ROI volume comparison showed significant volume reduction in the right dorsal ACC. VBM also showed a volume reduction in the right dorsal as well as a part of the rostral ACC as a compound mass. Both manual ROI tracing and optimized VBM suggest a subregion-specific pattern of ACC volume deficit in panic disorder. In addition to functional abnormalities, these results suggest that structural abnormalities of the ACC contribute to the pathophysiology of panic disorder. Funding:
|
Future Trends in Robotic Neurosurgery
|
Publication: 14th Nordic-Baltic Conference on Biomedical Engineering and Medical Physics 2008;20:229-33.| PDF Authors: Haidegger T, Kovacs L, Fordos G, Benyo Z, Kazanzides P. Institution: Laboratory of Medical Informatics, Department of Control Engineering and Information Technology, Budapest University of Technology and Economics, Budapest, Hungary. Background/Purpose: Computer Integrated Surgery has only existed for two decades, however it has already spread out world wide, with well over 100.000 operations performed. In the near future, newly developed robotic systems may conquer even the most challenging fields—such as neurosurgery—to provide better patient care and medical outcome. This paper presents the major systems and different strategies applied in robotic neurosurgery. Besides appropriate design, adequate control strategies are required to ensure maximal safety. This makes automated neurosurgery a technologically challenging area for researchers. It is also important during the design phase to consider market aspects. We anticipate that the future trends of clinical applications are outlined by the current leading research directions. The conclusions of the past years of innovation will lead forward on the path of further improvement. |
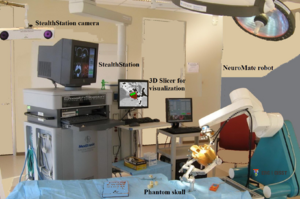 Robotic neurosurgery setup at the Johns Hopkins University with a modified NeuroMate robot, a StealthStation surgical navigation system and the 3D Slicer software. |
A Computer Modelling Tool for Comparing Novel ICD Electrode Orientations in Children and Adults
|
Publication: Heart Rhythm. 2008 Apr;5(4):565-72. PMID: 18362024 | PDF Authors: Jolley M, Stinstra J, Pieper S, Macleod R, Brooks DH, Cecchin F, Triedman JK. Institution: Department of Cardiology, Children’s Hospital Boston, Boston, MA, USA. Background/Purpose: Use of implantable cardiac defibrillators (ICDs) in children and patients with congenital heart disease is complicated by body size and anatomy. A variety of creative implantation techniques has been used empirically in these groups on an ad hoc basis. Objective: To rationalize ICD placement in special populations, we used subject-specific, image-based finite element models (FEMs) to compare electric fields and expected defibrillation thresholds (DFTs) using standard and novel electrode configurations. FEMs were created by segmenting normal torso computed tomography scans of subjects ages 2, 10, and 29 years and 1 adult with congenital heart disease into tissue compartments, meshing, and assigning tissue conductivities. The FEMs were modified by interactive placement of ICD electrode models in clinically relevant electrode configurations, and metrics of relative defibrillation safety and efficacy were calculated. Predicted DFTs for standard transvenous configurations were comparable with published results. Although transvenous systems generally predicted lower DFTs, a variety of extracardiac orientations were also predicted to be comparably effective in children and adults. Significant trend effects on DFTs were associated with body size and electrode length. In many situations, small alterations in electrode placement and patient anatomy resulted in significant variation of predicted DFT. We also show patient-specific use of this technique for optimization of electrode placement. Image-based FEMs allow predictive modeling of defibrillation scenarios and predict large changes in DFTs with clinically relevant variations of electrode placement. Extracardiac ICDs are predicted to be effective in both children and adults. This approach may aid both ICD development and patient-specific optimization of electrode placement. Further development and validation are needed for clinical or industrial utilization. Funding:
|
Using Magnetic Resonance Microscopy to Study the Growth Dynamics of a Glioma Spheroid in Collagen I: A Case Study
|
Publication: BMC Med Imaging. 2008 Jan 29;8:3. PMID: 18230155 | PDF Authors: Huang S, Vader D, Wang Z, Stemmer-Rachamimov A, Weitz DA, Dai G, Rosen BR, Deisboeck TS. Institution: Harvard-MIT (HST) Athinoula A, Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Charlestown, MA, USA. Background/Purpose: Highly malignant gliomas are characterized by rapid growth, extensive local tissue infiltration and the resulting overall dismal clinical outcome. Gaining any additional insights into the complex interaction between this aggressive brain tumor and its microenvironment is therefore critical. Currently, the standard imaging modalities to investigate the crucial interface between tumor growth and invasion in vitro are light and confocal laser scanning microscopy. While immensely useful in cell culture, integrating these modalities with this cancer's clinical imaging method of choice, i.e. MRI, is a non-trivial endeavour. However, this integration is necessary, should advanced computational modeling be able to utilize these in vitro data to eventually predict growth behavior in vivo. We therefore argue that employing the same imaging modality for both the experimental setting and the clinical situation it represents should have significant value from a data integration perspective. In this case study, we have investigated the feasibility of using a specific form of MRI, i.e. magnetic resonance microscopy or MRM, to study the expansion dynamics of a multicellular tumor spheroid in a collagen type I gel. |
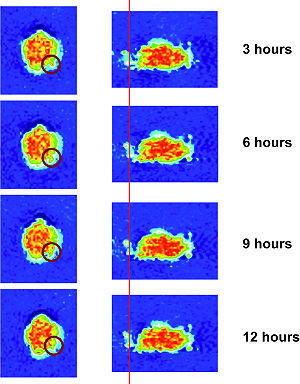 MRM images that show the MTS growth over time from different angles. The images to the left depict the axial view, whereas those to the right show an arbitrary angle. These 2D images confirm the surface heterogeneity that emerges already 12 hrs post placement of the MTS into the gel, and depict a small group of invasive cells (images on the right) that can also be seen in Figures 2(A) and 3. On the other hand, images on the left demonstrate that certain parts of the solid spheroid actually grew into the gel (red circle). |
Lowering the Barriers Inherent in Translating Advances in Neuroimage Analysis to Clinical Research Applications
|
Publication: Acad Radiol. 2008 Jan;15(1):114-8. PMID: 18078914 | PDF Authors: Pujol S, Kikinis R, Gollub R. Institution: Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: This article presents an initiative for the translation of advances in neuroimage analysis techniques to clinical research scientists. Our objective is to bridge the gap between scientific advances made by the biomedical imaging community and their widespread use in the clinical research community. Through national collaborative effort supported by the National Institutes of Health Roadmap, the integration of the most sophisticated algorithms into usable working open-source systems enables clinical researchers to have access to a broad spectrum of cutting edge analysis techniques. A critical step to maximize the long-term positive impact of this collaborative effort is to translate these techniques into new skills of clinical researchers. To address this challenge, we developed a methodology based on three criteria: a multidisciplinary approach, a balance between theory and common practice, and an immersive collaborative environment. The article illustrates our initiative through the exemplar case of diffusion tensor imaging tractography, and reports on our experience over the past two years of designing and delivering training workshops to more than 300 clinicians and scientists using the developed methodology. Funding:
|
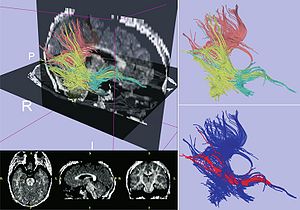 Exemplar case for Diffusion Tensor Imaging Tractography. Upper left panel displays fiber tractography combined with sagittal and axial slices from a fractional anisotropy map computed using 3D Slicer. Upper-right panel shows fiber tracts generated from regions of interest in the posterior-temporal lobe (yellow), splenium of the corpus callosum (pink), and temporal stem (green). Lower-right figure shows 3D visualization of the computed trajectory of the inferior occipito-frontal fasciculus bundle (red). |
2007
|
Publication: Comput Aided Surg. 2007 Nov;12(6):311-24. PMID: 18066947 | PDF Authors: Estepar RS, Stylopoulos N, Ellis R, Samset E, Westin C-F, Thompson C, Vosburgh K.G. Institution: Department of Radiology, Harvard Medical School and Brigham and Women's Hospital, Boston, MA, USA. Background/Purpose: Scarless surgery is an innovative and promising technique that may herald a new era in surgical procedures. We have created a navigation system, named IRGUS, for endoscopic and transgastric access interventions and have validated it in in vivo pilot studies. Our hypothesis is that endoscopic ultrasound procedures will be performed more easily and efficiently if the operator is provided with approximately registered 3D and 2D processed CT images in real time that correspond to the probe position and ultrasound image. The system provides augmented visual feedback and additional contextual information to assist the operator. It establishes correspondence between the real-time endoscopic ultrasound image and a preoperative CT volume registered using electromagnetic tracking of the endoscopic ultrasound probe position. Based on this positional information, the CT volume is reformatted in approximately the same coordinate frame as the ultrasound image and displayed to the operator. The system reduces the mental burden of probe navigation and enhances the operator's ability to interpret the ultrasound image. Using an initial rigid body registration, we measured the mis-registration error between the ultrasound image and the reformatted CT plane to be less than 5 mm, which is sufficient to enable the performance of novice users of endoscopic systems to approach that of expert users. Our analysis shows that real-time display of data using rigid registration is sufficiently accurate to assist surgeons in performing endoscopic abdominal procedures. By using preoperative data to provide context and support for image interpretation and real-time imaging for targeting, it appears probable that both preoperative and intraoperative data may be used to improve operator performance. Funding:
|
3D Visualization and Simulation of Frontoorbital Advancement in Metopic Synostosis
|
Publication: Childs Nerv Syst. 2007 Nov;23(11):1313-7. PMID: 17701413 | PDF Authors: Rodt T, Schlesinger A, Schramm A, Diensthuber M, Rittierodt M, Krauss JK. Institution: Department of Radiology, Hannover University Medical School, Hannover, Germany. Background/Purpose: Current multislice computed tomography (CT) technology can be used for diagnosis and surgical planning applying computer-assisted three-dimensional (3D) visualization and surgical simulation. The usefulness of a technique for surgical simulation of frontoorbital advancement is demonstrated here in a child with metopic synostosis. Postprocessing of multi-slice CT data was performed using the 3D Slicer software. 3D models were created for the purpose of surgical simulation. These allow planning the course of the osteotomies and individually placing the different bony fragments by an assigned matrix to simulate the surgical result. Photo documentation was obtained before and after surgery. Surgical simulation of the procedure allowed determination of the osteotomy course and assessment of the positioning of the individual bony fragments. Computer-assisted postprocessing and simulation is a useful tool for surgical planning in craniosynostosis surgery. The time-effort for segmentation currently limits the routine clinical use of this technique. |
Creating Physical 3D Stereolithograph Models of Brain and Skull
|
Publication: PLoS One. 2007 Oct; 2(10): e1119. PMID: 17971879 | PDF Authors: Kelley DJ, Farhoud M, Meyerand ME, Nelson DL, Ramirez LF, Dempsey RJ, Wolf AJ, Alexander AL, Davidson RJ. Institution: Waisman Laboratory for Brain Imaging and Behavior, Waisman Center, Madison, WI, USA. Background/Purpose: The human brain and skull are three dimensional (3D) anatomical structures with complex surfaces. However, medical images are often two dimensional (2D) and provide incomplete visualization of structural morphology. To overcome this loss in dimension, we developed and validated a freely available, semi-automated pathway to build 3D virtual reality (VR) and hand-held, stereolithograph models. To evaluate whether surface visualization in 3D was more informative than in 2D, undergraduate students (n = 50) used the Gillespie scale to rate 3D VR and physical models of both a living patient-volunteer's brain and the skull of Phineas Gage, a historically famous railroad worker whose misfortune with a projectile tamping iron provided the first evidence of a structure-function relationship in brain. Using our processing pathway, we successfully fabricated human brain and skull replicas and validated that the stereolithograph model preserved the scale of the VR model. Based on the Gillespie ratings, students indicated that the biological utility and quality of visual information at the surface of VR and stereolithograph models were greater than the 2D images from which they were derived. The method we developed is useful to create VR and stereolithograph 3D models from medical images and can be used to model hard or soft tissue in living or preserved specimens. Compared to 2D images, VR and stereolithograph models provide an extra dimension that enhances both the quality of visual information and utility of surface visualization in neuroscience and medicine. Funding:
|
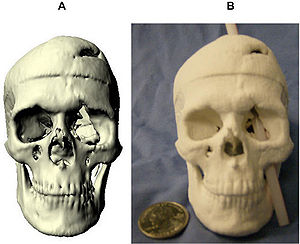 Stereolithograph of Phineas Gage's Skull. The processing pathway we developed can replicate preserved specimens. (a) Virtual model of Phineas Gage's skull. (b) With this physical 3D model of Phineas Gage's skull, we illustrate the approximate path of the tamping iron that produced Phineas Gage's famous injury. |
Morphology, Constraints, and Scaling of Frontal Sinuses in the Hartebeest, Alcelaphus Buselaphus (Mammalia: Artiodactlya, Bovidae)
|
Publication: Journal of Morphology 2007; 268:243-53. PMID: 17278134 | PDF See also 3D Slicer: The Tutorial Part V. Author: Farke AA. Institution: Department of Anatomical Sciences, Stony Brook University, New York, NY, USA. Background/Purpose: The frontal sinuses of bovid mammals display a great deal of diversity, which has been attributed to both phylogenetic and functional influences. In-depth study of the hartebeest (Alcelaphus buselaphus), a large African antelope, reveals a number of previously undescribed details of frontal sinus morphology. In A. buselaphus, the frontal sinuses conform closely to the shape of the frontal bone, filling nearly the entire element. However, the horncores are never extensively pneumatized, contrasting with the condition seen in many other bovids. This evidence is inconsistent with the hypothesis that sinuses are opportunistic pneumatizing agents, suggesting that phylogenetic factors also play a role in determining sinus size. Both cranial sutures and neurovasculature appear to constrain the growth of sinuses in part. In turn, the sinus also affects the growth of the parietal; apparently this element is not truly pneumatized by the sinus in most cases, but the bone’s shape changes under the influence of the sinus. Furthermore, the sinuses present relatively few struts when compared with the sinuses of some other bovids, such as Ovis. By adapting methods previously developed for measuring structural parameters of trabecular bone, it is possible to quantify certain aspects of sinus morphology. These include the number of bony struts within the sinus, the spacing of these struts, and the size of individual cavities within the sinus. Some differences in the number of struts are evident between subspecies. Similarly, significant differences occur in the relative number of struts between male and female A. buselaphus, which may be related to behavior. The volume of the sinus is strongly correlated with the size of the frontal, but less so with overall cranial size. This finding illustrates the importance of choosing variables carefully when comparing sinus sizes and growth between species. |
Image-guided Otologic Surgery Based on Patient Motion Compensation and Intraoperative Virtual CT
|
Publication: Proceedings of ACCAS2007, #P110064 Authors: Hong J, Matsumoto N, Ouchida R, Komune S, Hashizume M. Institution: Redox Navi Institute, Kyushu University, Japan. Background/Purpose: Image-guided surgery has been established particularly in ear, nose, throat (ENT) surgery that requires precise approach in small and complicated anatomy. During the surgery, the registration between the patient and the radiographic images must be maintained regardless of the patient movement. In this study, relative position and orientation of the surgical instrument is calculated referring to the moving patient position. Since the system does not directly handle the 3-D volume data, real-time update of 3-D navigational view is possible. The proposed method also keeps recording the surgical drill position while tracking it. With these digitized data, the temporal bone resection area is computed with several rule-based image processing. Finally, virtual CT images are constructed, and presented for the surgeon to understand and evaluate the current operation intraoperatively by observing their familiar CT images. The aim of this study is to develop and evaluate a novel otologic navigation system supporting patient motion compensation and intraoperative virtual CT construction. |
Non-rigid Registration of Pre-procedural MR Images with Intra- procedural Unenhanced CT Images for Improved Targeting of Tumors During Liver Radiofrequency Ablations
|
Publication: Int Conf Med Image Comput Comput Assist Interv. 2007;10(Pt 2):969-77. PMID: 18044662 | PDF Authors: Archip N, Tatli S, Morrison P, Jolesz F, Warfield SK, Silverman S. Institution: Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: In the United States, unenhanced CT is currently the most common imaging modality used to guide percutaneous biopsy and tumor ablation. The majority of liver tumors such as hepatocellular carcinomas are visible on contrast-enhanced CT or MRI obtained prior to the procedure. Yet, these tumors may not be visible or may have poor margin conspicuity on unenhanced CT images acquired during the procedure. Non-rigid registration has been used to align images accurately, even in the presence of organ motion. However, to date, it has not been used clinically for radiofrequency ablation (RFA), since it requires significant computational infrastructure and often these methods are not sufficient robust. We have already introduced a novel finite element based method (FEM) that is demonstrated to achieve good accuracy and robustness for the problem of brain shift in neurosurgery. In this current study, we adapt it to fuse pre-procedural MRI with intra-procedural CT of liver. We also compare its performance with conventional rigid registration and two non-rigid registration Methods: b-spline and demons on 13 retrospective datasets from patients that underwent RFA at our institution. FEM non-rigid registration technique was significantly better than rigid (p<10-5), non-rigid b-spline (p<10- 4) and demons (p<10-4) registration techniques. The results of our study indicate that this novel technology may be used to optimize placement of RF applicator during CT-guided ablations. Funding:
|
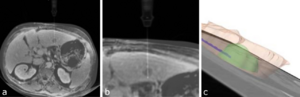 The position of RF applicator and tumor margin are illustrated on both axial images. Advanced 3D visualization using 3D Slicer enables accurate estimation of RFA electrode with respect to the tumor margins. |
A Detailed 3D Model of the Guinea Pig Cochlea
|
Publication: Brain Struct Funct. 2007 Sep;212(2):223-30. PMID: 17717692 Authors: Liu B, Gao XL, Yin HX, Luo SQ, Lu J. Institution: Department of Anatomy, Capital Medical University, Beijing, China. Background/Purpose: Several partial models of cochlear subparts are available. However, a complete 3D model of an intact cochlea based on actual histological sections has not been reported. Hence, the aim of this study was to develop a novel 3D model of the guinea pig cochlea and conduct post-processes on this reconstructed model. We used a combination of histochemical processing and the method of acquiring section data from the visible human project (VHP) to obtain a set of ideal raw images of cochlear sections. After semi-automatic registration and accurate manual segmentation with professional image processing software, one set of aligned data and six sets of segmented data were generated. Finally, the segmented structures were reconstructed by 3D Slicer (a professional imaging processing and analysis tool). Further, post-processes including 3D visualization and a virtual endoscope were completed to improve visualization and simulate the course of the cochlear implant through the scala tympani. The 3D cochlea model contains the main six structures: (1) the inner wall, (2) modiolus and spiral lamina, (3) cochlea nerve and spiral ganglion, (4) spiral ligament and inferior wall of cochlear duct, (5) Reissner's membrane and (6) tectorial membrane. Based on the results, we concluded that ideal raw images of cochlear sections can be acquired by combining the processes of conventional histochemistry and photographing while slicing. After several vital image processing and analysis steps, this could further generate a vivid 3D model of the intact cochlea complete with internal details. This novel 3D model has great potential in teaching, basic medical research and in several clinical applications. |
Dynamic 3-D Computer Modeling Tracks Brain Changes During Surgery
|
Publication: National Science Foundation (NSF) Discoveries - Brain Surgery: It Really Is Brain Surgery, August 31, 2007. Authors: Nikos Chrisochoides Institution: College of William and Mary, Williamsburg, VA, USA. Background/Purpose: In essence, the William and Mary team provides the surgical team with a dynamic computer model of the patient's brain. In clinical trials, Chrisochoides says his team can render a new model in six or seven minutes, but hopes to be able to do so in under two minutes. More... Funding:
|
Surface Rendering-based Virtual Intraventricular Endoscopy: Retrospective Feasibility Study and Comparison to Volume Rendering-based Approach
|
Publication: Neuroimage. 2007;37 Suppl 1:S89-99. PMID: 17513130 | PDF Authors: Nakajima N, Wada J, Miki T, Haraoka J, Hata N. Institution: Department of Radiology, Brigham and Women's Hospital, Boston, MA, USA. Background/Purpose: Virtual endoscopic simulations using volume rendering (VR) have been proposed as a tool for training and understanding intraventricular anatomy. It is not known whether surface rendering (SR), an alternative to VR, can visualize intraventricular and subependymal structures better and thus making the virtual endoscope more useful for simulating the intraventicular endoscopy. We sought to develop SR virtual endsocopy and compared the visibility of anatomical structures in SR and VR using retrospective cases. Fourteen patients who underwent endoscopic intraventricular surgery of third ventricle enrolled the study. SR virtual endoscopy module was developed in open-source software 3D Slicer and virtual endoscopic scenes from the retrospective cases were created. VR virtual endoscopy of the same cases was prepared in commercial software. Three neurosurgeons scored the visibility of substructures in lateral and third ventricle, arteries, cranial nerves, and other lesions. We found that VR and SR virtual endoscopy performed similarly in visualization of substructures in lateral and third ventricle (not significant statistically). However, the SR was statistically significantly better in visualizing subependymal arteries, cranial nerves, and other lesions (p<0.05, respectively). Funding:
|
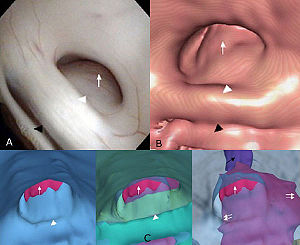 Visualization of the subependymal extension of the tumor in endoscopic surgical simulation using 3D Slicer. (A) The real intraoperative image (flexible videoscope) presents the cerebral aqueduct obstructed by the tectal tumor. (B) Volume rendering-based virtual endoscopy provides the similar image to the real intraoperative image. (C) Surface renderingbased virtual endoscopy reveals the subependymal extension of the tumor by changing the opacity and visibility of the other structures. Tumor (white arrow); posterior commissure (white arrowhead); habenular commissure (black arrowhead); cerebral aqueduct behind the tumor (black arrow). |
Interest of the Steady State Free Precession (SSFP) Sequence for 3D Modeling of the Whole Fetus
|
Publication: Proceedings of the 29th Annual International Conference of the IEEE EMBS, 2007. | PDF Authors: Anquez J, Angelini E, Bloch I, Merzoug V, Bellaiche-Millischer AE, Adamsbaum C. Institution: Signal and Image Processing Department, GET - Telecom Paris, France. Background/Purpose: Fetal magnetic resonance imaging (MRI) has been gaining interest over the last two decades. Current fast MRI sequences provide imaging data of the whole uterus in less than 20 seconds, avoiding fetal motion related artifacts without any maternal or fetal sedation. MRI has proved to be a useful adjunct to echographic screening for prenatal diagnosis. However, MRI volumetric data is still mainly interpreted on 2D slices and 3D applications remain limited. In this paper, we discuss the qualities of the SSFP MRI sequences to provide adequate data for 3D segmentation and modeling of the fetus. Potential exploitations of 3D segmentation and derived anatomical models cover several domains: biometric and morphologic clinical studies, quantitative longitudinal studies of normal and abnormal fetus developments, direct visualization of the overall fetus body and simulations in different fields (surgery, radiation dosimetry,...). |
Longitudinal in Vivo Reproducibility of Cartilage Volume and Surface in Osteoarthritis of the Knee
|
Publication: Skeletal Radiol. 2007 Apr;36(4):315-20. PMID: 17219231 | PDF Authors: Brem MH, Pauser J, Yoshioka H, Brenning A, Stratmann J, Hennig FF, Kikinis R, Duryea J, Winalski CS, Lang P. Institution: Musculoskeletal Division, Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: The aim of this study was to evaluate the longitudinal reproducibility of cartilage volume and surface area measurements in moderate osteoarthritis (OA) of the knee. We analyzed 5 MRI (GE 1.5T, sagittal 3D SPGR) data sets of patients with osteoarthritis (OA) of the knee (Kellgren Lawrence grade I-II). Two scans were performed: one baseline scan and one follow-up scan 3 months later (96±10 days). For segmentation, 3D Slicer v.2.5 software was used. Two segmentations were performed by two readers independently who were blinded to the scan dates. Tibial and femoral cartilage volume and surface were determined. Longitudinal and cross-sectional precision errors were calculated using the standard deviation (SD) and coefficient of variation (CV%=100x[SD/mean]) from the repeated measurements in each patient. The in vivo reproducibility was then calculated as the root mean square of these individual reproducibility errors. The cross-sectional root mean squared coefficient of variation (RMSE-CV) was 1.2, 2.2 and 2.4% for surface area measurements (femur, medial and lateral tibia respectively) and 1.4, 1.8 and 1.3% for the corresponding cartilage volumes. Longitudinal RMSE-CV was 3.3, 3.1 and 3.7% for the surface area measurements (femur, medial and lateral tibia respectively) and 2.3, 3.3 and 2.4% for femur, medial and lateral tibia cartilage volumes. The longitudinal in vivo reproducibility of cartilage surface and volume measurements in the knee using this segmentation method is excellent. To the best of our knowledge we measured, for the first time, the longitudinal reproducibility of cartilage volume and surface area in participants with mild to moderate OA. Funding:
|
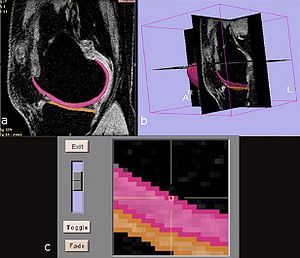 Screen shots of the segmentation software, the 3D Slicer. |
A Novel Manipulator for 3D Ultrasound Guided Percutaneous Needle Insertion
|
Publication: IEEE International Conference on Robotics and Automation. 2007 Apr 10-14; pp.617-22. Authors: Bassan H, Hayes T, Patel RV, Moallem M. Institution: Department of Electrical and Computer Engineering, Western Ontario University, London, ON, Canada. Background/Purpose: The prostate is a small exocrine gland in men responsible for production of the liquid component of the seminal fluid. In North America, prostate cancer accounts for over 300,000 new cases and 40,000 deaths each year and it is the second leading cause of cancer death in men. Low-dose Rate (LDR) brachytherapy is gaining interest as a viable treatment option for prostate cancer due to its low side effects and high benefits. The present manual approach for brachytherapy needle insertion and the inherent flexibility of the needles make it extremely difficult to achieve accurate and consistent dosimetry. In this paper, we present a new 5 degrees-of-freedom (DOF) manipulator capable of performing percutaneous needle insertion. The manipulator can perform orientation, insertion and rotation of the needle and linear motion of the plunger to drop radioactive seeds at targeted locations. The manipulator is an integral part of a system utilizing a mechanically rotated side-fire transducer to create 3D ultrasound images of the organ and utilizing 3D Slicer software to visualize those images. Experiments conducted in agar phantoms reveal an average RMS targeting error of 1.45mm at an average insertion depth of 75.78 mm proving the feasibility and efficacy of the proposed robotic system for percutaneous needle insertion. |
Origin and Insertion Points Involved in Levator Ani Muscle Defects
|
Publication: Am J Obstet Gynecol. 2007 Mar;196(3):251.e1-5. PMID: 17346542 | PDF Authors: Margulies RU, Huebner M, DeLancey JO. Institution: Pelvic Floor Research Group, University of Michigan, Ann Arbor, MI, USA. Background/Purpose: This project sought to identify and to describe the anatomical connections affected by levator ani defects involving the pubovisceral portion of the muscle. Fourteen magnetic resonance scans of women with unilateral levator defects were selected. The missing muscle mapping technique was used to characterize the absent muscle. Normal muscle was visualized and compared with the contralateral side. Using 3D Slicer, the outline of the intact muscle was traced; models of this muscle and surrounding structures were generated. The missing muscle originates from the posterior pubic bone and extends laterally over the obturator internus muscle; it inserts into the vaginal wall, perineal body, and the intersphincteric space. Architectural distortion, with an asymmetric lateral spilling of the vagina was present in 50% of women. The defect was right sided in 71% of patients. The origin and insertion points of the damaged portion of the levator ani muscle were identified. Funding:
|
A Prototype Biosensor-integrated Image-guided Surgery System
|
Publication: Int J Med Robot. 2007 Mar;3:82-8. PMID: 17441030 | PDF Authors: Reisner LA, King BW, Klein MD, Auner GW, Pandya AK. Institution: Department of Electrical and Computer Engineering, Wayne State University, Detroit, MI, USA. Background/Purpose: In this study we investigated the integration of a Raman spectroscopy-based biosensor with an image-guided surgery system. Such a system would provide a surgeon with both a diagnosis of the tissue being analyzed (e.g. cancer) and localization information displayed within an imaging modality of choice. This type of mutual and registered information could lead to faster diagnoses and enable more accurate tissue resections. Methods: A test bed consisting of a portable Raman probe attached to a passively articulated mechanical arm was used to scan and classify objects within a phantom skull. The prototype system was successfully able to track the Raman probe, classify objects within the phantom skull, and display the classifications on medical imaging data within a virtual reality environment. We discuss the implementation of the integrated system, its accuracy and improvements to the system that will enhance its usefulness and further the field of sensor-based computer-assisted surgery. Funding:
|
|
Publication: Int J CARS (2007) 2:65-73. | PDF Authors: Diakov G, Freysinger W. Institution: 4D Visualization Laboratory, University Clinic of Oto-, Rhino-, Laryngology, Innsbruck Medical University, Innsbruck, Austria. Background/Purpose: An initialization-free approach for perioperative registration in functional endoscopic sinus surgery (FESS) is sought. The quality of surgical navigation relies on registration accuracy of preoperative images to the patient. Although landmark-based registration is fast, it is prone to human operator errors. This study evaluates the accuracy of two well-known methods for segmentation of the occipital bone from CT-images for use in surgical 3D-navigation. Funding:
|
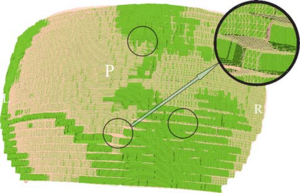 A zoom in the mesh, displayed in 3D Slicer. The oversampling is seen as three layers at each “step”. The difference between the TMCS mesh and the “ground truth” is seen in the colored spots (“ground truth” green, TMCS pink). The three circles mark zones with visibly discernible differences in the segmentation; the inset is a magnification of one of these zones |
Development of a Three-dimensional Multiscale Agent-based Tumor Model: Simulating Gene-protein Interaction Profiles, Cell Phenotypes and Multicellular Patterns in Brain Cancer
|
Publication: J Theor Biol. 2007 Jan 7;244(1):96-107. PMID: 16949103 | PDF Authors: Zhang L, Athale CA, Deisboeck TS. Institution: Complex Biosystems Modeling Laboratory, Massachusetts General Hospital, Harvard medical School, Boston, MA, USA. Background/Purpose: Related also to efforts within the Center for the Development of a Virtual Tumor, CViT, our research here focuses on developing multi-scale and multi-resolution (brain) cancer models. Using a hybrid 3D agent-based modeling platform we connect gene-protein interaction maps on the molecular and single cell level (Figure 1, left) up to the volumetric tumor scale of clinical MR-images. For the latter, we plan on using 3D Slicer for segmentation of tumor-affected areas and 3D reconstruction of tumor volume and surface. Figure 1, right depicts a first step towards this approach where the yellow points depict the 3D surface reconstruction of a T1+Gd MRI while the blue and red points represent virtual tumor cells in attempt to match the real data points. Amongst the more challenging steps is the translation of these 2D in vivo imaging data onto our in silico lattices. Funding:
|
Image Registered FAST (IRFAST) for Combat Casualty Triage
|
Authors: Pohl KM, Pieper S, Vosburgh K, Takacs B. Background/Purpose: Dr. Pohl's research involves developing an automatic segmentation approach identifying major anatomical compartments from torso CT scans. Using 3D Slicer, he developed a procedure for automatically segmenting the body, bone structures, lungs, and hart from CT images (see figure). The method iterates between the identification of anatomical structures and the registration of an “atlas” to the CT data set of the subject. The atlas is based on CT data set, which we call template, and a label map that already identifies the structures of interest in the template. In the first iteration, the template with the segmentation of the body is mapped onto the CT data set of the subject. This results in a very accurate segmentation of the subject’s body. The method then combines the segmentation of the body and the CT images of the subject to identify the lungs and bone structures. In the second iteration, the method maps the atlas specific label map of body, bones, and lungs to the corresponding label map of the subject. The segmented structures are then used as a "coordinate system" used for the identification of the remaining anatomical compartments. Funding:
|
A Preliminary Study on the Relationship between Nasal Cavity and Maxillary Sinus Volumes
|
Publication: Proceedings of the 76th Annual Meeting of the American Association of Physical Anthropologists Mar 2007. | PDF Authors: Butaric LN, Broadfield DC, McCarthy RC. Institution: Department of Anthropology, Texas A&M University, College Station, TX, USA. Background/Purpose: Previous research suggests that nasal cavity volume (NCV), thought to be related to climate, is inversely correlated with maxillary sinus volume (MSV). According to this hypothesis, changes in nasal cavity size and shape reflect physiological needs, such as warming and humidifying inspired air. Owing to volumetric constraints in the mid-face, relative increases in NCV are hypothesized to result in concomitant decreases in MSV, respectively. To test this hypothesis thirty-nine dried adult human crania from seven different climatic regions were examined using computerized tomography (CT) scans. Significant differences in MSV and NCV between populations were identified using Analysis of Variance (ANOVA). In addition, least-squares and reduced major axis (RMA) regression analyses were performed to test the scaling relationships between MSV, NCV and several cranial size variables. Contrary to previous studies, results indicate that MSV and NCV are not significantly correlated. RMA analyses indicate that NCV, but not MSV, scales isometrically with skull size. Finally, post hoc ANOVA results identify significant differences between human populations for MSV that do not follow climatic or environmental trends. These results suggest that (1) it is unlikely that NCV and MSV compete for space in the mid-face, (2) NCV is largely a byproduct of skull size, and (3) NCV and MSV may not be as closely tied to climate as previously thought. Additional genetic and epigenetic factors need to be considered regarding the structure and function of the human maxillary sinus. |
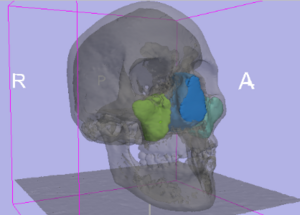 Color labels of segmented areas were then rendered using the “Model Module” in 3D Slicer to create 3D models. Using the “MeasVol Module,” absolute volumes of the nasal cavity and each maxillary sinus were quantified. |
Interobserver Variability in the Determination of Upper Lobe-predominant Emphysema
|
Publication: Chest. 2007 Feb;131(2):424-31. PMID: 17296643 | PDF Authors: Hersh CP, Washko GR, Jacobson FL, Gill R, Estepar RS, Reilly JJ, Silverman EK. Institution: Channing Laboratory, Brigham and Women's Hospital, Boston, MA, USA. Background/Purpose: Appropriateness for lung volume reduction surgery is often determined based on the results of high-resolution CT (HRCT) scanning of the chest. At many centers, radiologists and pulmonary physicians both review the images, but the agreement between readers from these specialties is not known. Two thoracic radiologists and three pulmonologists retrospectively reviewed the HRCT scans of 30 patients with emphysema involved in two clinical studies at our institution. Each reader assigned an emphysema severity score and assessed upper lobe predominance, using a methodology similar to that of the National Emphysema Treatment Trial. In addition, the percentage of emphysema at -910 Hounsfield units was objectively determined by density mask analysis. For the emphysema severity scores, (Spearman) correlation between readers ranged from 0.59 (p = 0.0005) to 0.87 (p < 0.0001), with generally stronger correlations among readers from the same medical specialty. Emphysema severity scores were significantly correlated with prebronchodilator and postbronchodilator spirometry findings, as well as with density mask analysis. In the assessment of upper lobe predominance, kappa statistics for agreement ranged from 0.20 (p = 0.4) to 0.60 (p = 0.0008). Examining all possible radiologist-pulmonologist pairs, the two readers agreed in their assessments of emphysema distribution in 75% of the comparisons. Readers agreed on upper lobe-predominant disease in 9 of the 10 patients in which regional density mask analysis clearly showed upper lobe predominance. In a group of patients with varying emphysema severity, interobserver agreement in the determination of upper lobe-predominant disease was poor. Agreement between readers tended to be better in cases with clear upper lobe predominance as determined by densitometry. Funding:
|
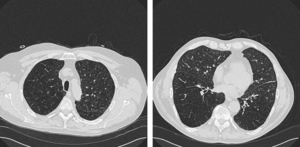 Example of disagreement among readers. Two of five observers interpreted this HRCT scan as showing upper lobe-predominant emphysema. Representative 1-mm sections from the level of (left, A) the top of the aortic arch and (right, B) the right inferior pulmonary vein are shown, using lung windows (width, –1,500 HU; level, 600 HU). |
Registered, Sensor-integrated Virtual Reality for Surgical Applications
|
Publication: Proceedings of the International Conference and Exhibition in Virtual Reality 2007; 277-8. | PDF Authors: King BW, Reisner LA, Klein MD, Auner GW, Pandya AK. Institution: Wayne State University, Detroit, MI, USA. Background/Purpose: The visualization for our image-guided surgery system is implemented using 3D Slicer, an open-source application for displaying medical data. 3D Slicer provides a virtual reality environment in which various imaging modalities (e.g. CT or MRI data) can be presented. The software includes the ability to display the locations of objects with respect to 3D models that are derived from segmentation of the medical imaging. We modified 3D Slicer in several ways to adapt it to our application. First, we developed a TCP/IP interface that receives the tracking data for the MicroScribe and displays its position in the VR environment relative to the medical imaging data. This allows us to track the Raman probe in real-time. Second, we developed a way to place colored markers that indicate tissue/material classification on the medical imaging data. The combination of these modifications enables us to denote the location and classification of tissue/material scanned with the probe in near-real-time. |
Modeling Cancer Biology
|
Publication: Biomedical Computation Review Spring 2007 pp. 16-24. | PDF Author: Kristin Cobb |
A Comparison of Upper Airway Structures in Male and Female Obstructive Sleep Apnoea (OSA) Patients
|
Publication: Poster Presentation at the 2007 American Thoracic Society International Conference. Authors: McEvoy RD, Ryan MK, Catcheside PG, Jakab M, Malhotra A, Sage MR, Valentine R, White DP. Institution: Adelaide Institute for Sleep Health, Repatriation General Hospital, Daw Park, South Australia. Background/Purpose: For the same BMI female OSA patients tend to have less severe sleep disordered breathing than male OSA patients. This study investigates features of upper airway anatomy that may contribute to this difference. Male (n=6) and female (n=9) patients matched for age [mean(SD); men 56.5(5.7), women 55.3(6.2) yrs] and BMI [35.2(3.4), 34.3 (3.0) kg/m²], who had previously been diagnosed with OSA (AHI>30/h), and adherent with CPAP for >3 months were studied. T1 weighted magnetic resonance imaging of the upper airway and surrounding tissues was performed and analyzed using 3D Slicer to determine airway, soft tissue and bony dimensions. The oropharyngeal bony vault volume was greater in males after normalizing for height (1.2(0.1) vs 0.97(0.1), mls/cm, p=0.001). Men had greater neck circumference (45.3(4.3) vs 39.5(4.5) cm, p=0.026) and longer pharyngeal airways (75.2(8.3) vs 64.6(9.5) mm, p=0.042) compared to women. Pharyngeal airway volume and minimum CSA were not different between the genders. In the mid sagittal plane, the tongue CSA was greater in men before and after (36.4(1.4) vs 32.6(3.5) mm²/mm, p=0.01) normalizing for bony vault dimensions. In data collected to date, AHI was not different between males and females (55(12) vs 62(21) events/h). These preliminary data suggest that male OSA patients have greater oropharyngeal bony vault volume than female patients; a larger tongue (normalized for bony vault dimensions) and a longer pharyngeal airway. These findings may have implications for the male predisposition for OSA. Funding:
|
2006
Shaving Diffusion Tensor Images in Discriminant Analysis: A Study into Schizophrenia
|
Publication: Med Image Anal. 2006 Dec;10(6):841-9. PMID: 16965928 | PDF Authors: Caan MW, Vermeer KA, van Vliet LJ, Majoie CB, Peters BD, den Heeten GJ, Vos FM. Institution: Quantitative Imaging Group, Delft University of Technology, Delft, The Netherlands. Background/Purpose: A technique called 'shaving' is introduced to automatically extract the combination of relevant image regions in a comparative study. No hypothesis is needed, as in conventional pre-defined or expert selected region of interest (ROI)-analysis. In contrast to traditional voxel based analysis (VBA), correlations within the data can be modeled using principal component analysis (PCA) and linear discriminant analysis (LDA). A study into schizophrenia using diffusion tensor imaging (DTI) serves as an application. Conventional VBA found a decreased fractional anisotropy (FA) in a part of the genu of the corpus callosum and an increased FA in larger parts of white matter. The proposed method reproduced the decrease in FA in the corpus callosum and found an increase in the posterior limb of the internal capsule and uncinate fasciculus. A correlation between the decrease in the corpus callosum and the increase in the uncinate fasciculus was demonstrated. Funding:
|
|
Publication: Med Bio Eng Comput. 2006 Dec; 44(12):1127-34. PMID: 17102954 Authors: Hong J, Nakashima H, Konishi K, Ieiri S, Tanoue K, Hashizume M. Institution: Redox Navi Institute, Kyushu University, Fukuoka, Japan. Background/Purpose: Surgical navigation systems can contribute to abdominal interventions such as radiofrequency ablation (RFA) or percutaneous ethanol injection therapy (PEIT) for liver tumors. Until now, typical abdominal interventions have been performed using the US guidance approach. Identification of the lesion by these methods has often been difficult, especially when tumors were small and US images were unclear. To improve the treatment with better lesion identification, 3D navigation based on MRI or CT is crucial. Particularly, MRI-based navigation systems have been preferred in respect of avoidance of ionizing radiation. To our knowledge, this is the first trial of abdominal needle insertion intervention under local anaesthesia using simultaneous MRI and US navigation. To accomplish this purpose, the semi-automatic fiducial registration is required. While scanning the abdominal area and using the optical tracking system, partial loss of the markers often occurs, leading to the prolongation of the limited intervention time. The proposed method combats this problem. In this paper, we elucidate whether the MRI and US integrated navigation assists in reliable needle insertion and reduce the time required to determine the needle insertion path in abdominal interventions. |
Diffusion Tensor Imaging Reveals White Matter Reorganization in Early Blind Humans
|
Publication: Cereb Cortex. 2006 Nov;16(11):1653-61. PMID: 16400157 | PDF Authors: Shimony JS, Burton H, Epstein AA, McLaren DG, Sun SW, Snyder AZ. Institution: Mallinckrodt Institute of Radiology, Washington University School of Medicine, St Louis, MO, USA. Background/Purpose: Multiple functional methods including functional magnetic resonance imaging, transcranial magnetic stimulation, and positron emission tomography have shown cortical reorganization in response to blindness. We investigated microanatomical correlates of this reorganization using diffusion tensor imaging and diffusion tensor tractography (DTT). Five early blind (EB) were compared with 7 normally sighted (NS) persons. DTT showed marked geniculocalcarine tract differences between EB and NS participants. All EB participants showed evidence of atrophy of the geniculocortical tracts. Connections between visual cortex and the orbital frontal and temporal cortices were relatively preserved in the EB group. Importantly, no additional tracts were found in any EB participant. Significant alterations of average diffusivity and relative anisotropy were found in the white matter (WM) of the occipital lobe in the EB group. These observations suggest that blindness leads to a reorganization of cerebral WM and plausibly support the hypothesis that visual cortex functionality in blindness is primarily mediated by corticocortical as opposed to thalamocortical connections. Funding:
|
Molar Crown Thickness, Volume, and Development in South African Middle Stone Age Humans
|
Publication: South African Journal of Science. 2006;102(11-12):513-517. | PDF Authors: Smith TM, Olejniczak AJ, Tafforeau P, Reid DJ, Grine FE, Hublin JJ. Institution: Department of Human Evolution, Max Planck Institute for Evolutionary Anthropology, Leipzig, Germany. Background/Purpose: One highly debated issue in palaeoanthropology is that of modern human origins, particularly the issue of when 'anatomically modern humans' (AMH) from the African Middle Stone Age became fully modern. While studies of cranial and external dental morphology suggest a modern transition occurred 150 000-200 000 years ago, little is known about dental development or enamel thickness in AMH. Studies of early members of the genus Homo suggest that the modern, prolonged condition of tooth growth arose late in human evolution, and that the enamel thickness of earlier hominins may not be homologous to the modern condition. This study represents the first integrated investigation of molar crown enamel thickness, volume, and development in fossil hominins, aimed at determining whether differences between AMH and living populations can be detected in these traits. Using high-resolution micro-computed tomography, we demonstrate similarities in enamel thickness and crown volumes between fossil and modern populations. Additionally, long-period growth line numbers and estimates of crown formation times for AMH molars fall within modern human ranges. These findings suggest that tooth structure and growth have remained constant for more than 60 000 years, despite the known geographical, technological, and ecological diversity that characterizes later stages of human evolution. |
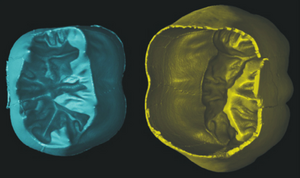 Virtually separated coronal dentine (left) and enamel cap (right) of the right lower first molar illustrated in Figs 1 and 3. A small amount of enamel is missing on the lingual cervix. The volume and surface area of each of these tissues was calculated, which was used to calculate the 3D average and relative enamel thickness (see text). |
A 3D Model Simulating Sediment Transport, Erosion and Deposition within a Network of Channel Belts and an Associated Floodplain
|
Publication: PowerPoint Presentation PDF Authors: Karssenberg D, Bridge J. Institution: Utrecht University, The Netherlands. |
Molecular Diffusion in MRI: Technical Application of Fiber Tracking
|
Publication: PowerPoint Presentation PPT Author: Martha Liliana Mora V. Institution: Rey Juan Carlos University, Madrid, Spain. |
Quantification of Levator Ani Cross-sectional Area Differences between Women with and Those without Prolapse
|
Publication: Obstet Gynecol. 2006 Oct;108(4):879-83. PMID: 17012449 | PDF Authors: Hsu Y, Chen L, Huebner M, Ashton-Miller JA, DeLancey JO. Institution: University of Michigan, Ann Arbor, MI, USA. Background/Purpose: Compare levator ani cross-sectional area as a function of prolapse and muscle defect status. Thirty women with prolapse and 30 women with normal pelvic support were selected from an ongoing case-control study of prolapse. For each of the two groups, 10 women were selected from three categories of levator defect severity: none, minor, and major identified on supine magnetic resonance scans. Using those scans, three-dimensional (3D) models of the levator ani muscles were made using 3D Slicer, a modeling program, and cross-sections of the pubic portion were calculated perpendicular to the muscle fiber direction using another program, I-DEAS. An analysis of variance was performed. The ventral component of the levator muscle of women with major defects had a 36% smaller cross-sectional area, and women with minor defects had a 29% smaller cross-sectional area compared with the women with no defects (P < .001). In the dorsal component, there were significant differences in cross-sectional area according to defect status (P = .03); women with major levator defects had the largest cross-sectional area compared with the other defect groups. For each defect severity category (none, minor, major), there were no significant differences in cross-sectional area between women with and those without prolapse. Women with visible levator ani defects on magnetic resonance imaging had significantly smaller cross-sectional areas in the ventral component of the pubic portion of the muscle compared with women with intact muscles. Women with major levator ani defects had larger cross-sectional areas in the dorsal component than women with minor or no defects. Funding:
|
 3D Slicer models. A. Three-fourths view of the levator ani muscle and pubic bone. B. Levator ani with pubic bones removed. C. Lateral view of muscle. |
Liver Metastases: 3D Shape-based Analysis of CT Scans for Detection of Local Recurrence After Radiofrequency Ablation
|
Publication: Radiology. 2006 Oct;241(1):243-50. PMID: 16928977 | PDF Authors: Bricault I, Kikinis R, Morrison PR, Vansonnenberg E, Tuncali K, Silverman SG. Institution: Department of Radiology, University Hospital Michallon, Grenoble, France. Background/Purpose: The purpose of this pilot study was to determine retrospectively the diagnostic performance of a computer-aided three-dimensional (3D) analytic tool for assessing local recurrences of liver metastases by quantifying shape changes in ablated tumors on computed tomographic (CT) scans for follow-up of radiofrequency (RF) ablation. Positron emission tomographic and long-term CT follow-up images were reference standards. Fifty-six follow-up CT scans of 12 liver metastases (mean size, 4.0 cm) in nine patients treated with RF ablation were retrospectively analyzed. After the 1st month following RF ablation, the 3D analytic tool helped quantify ablated tumor shape variations and revealed recurrences even in the absence of abnormal enhancement (sensitivity, seven of seven; specificity, three of five). The 3D tool would have revealed a recurrence before it was reported clinically in two patients. Although results are preliminary, a 3D analytic tool based on shape may be useful in assessing RF ablation results. Funding:
|
Atlas Guided Identification of Brain Structures by Combining 3D Segmentation and SVM Classification
|
Publication: Int Conf Med Image Comput Comput Assist Interv. 2006 Oct;9(Pt 2):209-16. PMID: 17354774 | PDF Authors: Akselrod-Ballin A, Galun M, Gomori MJ, Basri R, Brandt A. Institution: Department of Computer Science and Applied Math, Weizmann Institute of Science, Rehovot, Israel. Background/Purpose: This study presents a novel automatic approach for the identification of anatomical brain structures in magnetic resonance images (MRI). The method combines a fast multiscale multi-channel three dimensional (3D) segmentation algorithm providing a rich feature vocabulary together with a support vector machine (SVM) based classifier. The segmentation produces a full hierarchy of segments, expressed by an irregular pyramid with only linear time complexity. The pyramid provides a rich, adaptive representation of the image, enabling detection of various anatomical structures at different scales. A key aspect of the approach is the thorough set of multiscale measures employed throughout the segmentation process which are also provided at its end for clinical analysis. These features include in particular the prior probability knowledge of anatomic structures due to the use of an MRI probabilistic atlas. An SVM classifier is trained based on this set of features to identify the brain structures. We validated the approach using a gold standard real brain MRI data set. Comparison of the results with existing algorithms displays the promise of our approach. Funding:
|
Development of a CAD (Computer Assisted Detection) System to Detect Lung Nodules in CT Scans
|
Publication: PDF Authors: Tommasi E, De Nunzio G. Institution: Departments of Physics and Material Science, University of Lecce, Italy. Background/Purpose: We implemented a piece of software to segment lung tissue in CT thoracic images. We gave particular attention to the study of the ilhus pulmonis (region of entrance of bronchi and vessels in the lung parenchima). It is a delicate region in segmentation. We used 3D Slicer to visualize the different steps of the algorithm, checking their correctness. Through a segmentation technique, known as “region growing”, we obtained the delineation of the respiratory apparatus domain in the CT scans. This algorithm is completely three-dimensional. Its output consists in the 3D mask of the respiratory apparatus. We used 3D Slicer to visualize it. Then through an alternative version of region growing, based on a wavefront simulation algorithm, we obtained the segmentation of the external bronchi. We also used the opacity proprieties to put in evidence the internal structures of lungs (such as vessels). |
Dynamic Simulation of Joints using Multi-Scale Modeling
|
Author: Trent M. Guess Institution: Mechanical Engineering, University of Missouri, Kansas City, MO, USA. Background/Purpose:
Funding:
|
Quasi-isometric Flattening of Curved Surfaces for Medical Imaging
|
Researchers: Zeevi YY, Saucan E, Appleboim E. Institution: Department of Electrical-Engineering, Technion-Israel Institute of Technology, Haifa, Israel. Description: CT/MRI-scans of human brain-cortex/colon are flattened in a quasi-isometric manner in order to keep angles/length/area as minimally distorted as possible. 3D-surfaces are created out of real data scans, using 3D Slicer. Funding:
|
A Translation Station for Imaging
|
Publication: RSNA 2006; Authors: Mongkolwat P, Lechner T, Kogan A, Talbot S, Johnson B, Channin DS. Institution: Imaging Informatics Section, Northwestern University, Chicago, IL, USA. Background/Purpose: While providing clinical feedback to the basic sciences. In imaging informatics, this means enabling collaborations between radiologists and computer scientists. Commercial workstations do not allow for experimentation nor do they evolve fast enough. Research imaging packages, while innovative, do not provide for clinical activities or regulatory compliance. We added IHE workflow functionality, hanging protocols and other clinical functions to the 3D Slicer research platform. We leveraged the functionality and methodology of the Insight and Visualization Toolkits, and the DCM4CHE tools. A research mode allows for the evaluation of experimental algorithms against a PACS while protecting patient confidentiality. This combined functionality allows researchers to develop algorithms against clinical cases while at the same allowing clinicians to explore and validate these developments. |
User-guided 3D Active Contour Segmentation of Anatomical Structures: Significantly Improved Efficiency and Reliability
|
Publication: Neuroimage. 2006 Jul 1;31(3):1116-28. PMID: 16545965 | PDF Authors: Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, Gerig G. Institution: Penn Image Computing and Science Laboratory, Department of Radiology, University of Pennsylvania, PA, USA. Background/Purpose: Active contour segmentation and its robust implementation using level set methods are well-established theoretical approaches that have been studied thoroughly in the image analysis literature. Despite the existence of these powerful segmentation methods, the needs of clinical research continue to be fulfilled, to a large extent, using slice-by-slice manual tracing. To bridge the gap between methodological advances and clinical routine, we developed an open source application called ITK-SNAP, which is intended to make level set segmentation easily accessible to a wide range of users, including those with little or no mathematical expertise. This paper describes the methods and software engineering philosophy behind this new tool and provides the results of validation experiments performed in the context of an ongoing child autism neuroimaging study. The validation establishes SNAP intrarater and interrater reliability and overlap error statistics for the caudate nucleus and finds that SNAP is a highly reliable and efficient alternative to manual tracing. Analogous results for lateral ventricle segmentation are provided. Funding:
|
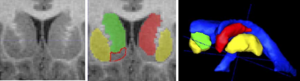 Two and three-dimensional views of the caudate nucleus. Coronal slice of the caudate: original T1-weighted MRI (left) and overlay of segmented structures (middle). Right and left caudate are shown shaded in green and red; left and right putamen are sketched in yellow, laterally exterior to the caudates. The nucleus accumbens is sketched in red outline. Note the lack of contrast at the boundary between the caudate and the nucleus accumbens, and the fine-scale cell bridges between the caudate and the putamen. At right is a 3D view of the caudate and putamen relative to the lateral ventricles. |
Habitual Use of the Primate Forelimb is Reflected in the Material Properties of Subchondral Bone in the Distal Radius
|
Publication: J Anat. 2006 Jun; 208(6):659-70. PMID: 16761969 | PDF Authors: Carlson KJ, Patel BA. Institution: Department of Anatomical Sciences, School of Medicine, Stony Brook University, NY, USA. Background/Purpose: Bone mineral density is directly proportional to compressive strength, which affords an opportunity to estimate in vivo joint load history from the subchondral cortical plate of articular surfaces in isolated skeletal elements. Subchondral bone experiencing greater compressive loads should be of relatively greater density than subchondral bone experiencing less compressive loading. Distribution of the densest areas, either concentrated or diffuse, also may be influenced by the extent of habitual compressive loading. We evaluated subchondral bone in the distal radius of several primates whose locomotion could be characterized in one of three general ways (quadrupedal, suspensory or bipedal), each exemplifying a different manner of habitual forelimb loading (i.e. compression, tension or non-weight-bearing, respectively). We employed computed tomography osteoabsorptiometry (CT-OAM) to acquire optical densities from whichfalse-color maps were constructed. The false-color maps were used to evaluate patterns in subchondral density (i.e. apparent density). Suspensory apes and bipedal humans had both smaller percentage areas and less well-defined concentrations of regions of high apparent density relative to quadrupedal primates. Quadrupedal primates exhibited a positive allometric effect of articular surface size on high-density area, whereas suspensory primates exhibited an isometric effect and bipedal humans exhibited no significant relationship between the two. A significant difference between groups characterized by predominantly compressive forelimb loading regimes vs. tensile or non-weight-bearing regimes indicates that subchondral apparent density in the distal radial articular surface distinguishes modes of habitually supporting of body mass. Funding:
|
Appearance of the Levator Ani Muscle Subdivisions in Magnetic Resonance Images
|
Publication: Obstet Gynecol. 2006 May;107(5):1064-9. PMID: 16648412 | PDF Authors: Margulies RU, Hsu Y, Kearney R, Stein T, Umek WH, DeLancey JO. Institution: University of Michigan, Ann Arbor, MI, USA. Background/Purpose: Identify and describe the separate appearance of 5 levator ani muscle subdivisions seen in axial, coronal, and sagittal magnetic resonance imaging (MRI) scan planes. Magnetic resonance scans of 80 nulliparous women with normal pelvic support were evaluated. Characteristic features of each Terminologia Anatomica-listed levator ani component were determined for each scan plane. Muscle component visibility was based on pre- established criteria in axial, coronal, and sagittal scan planes: 1) clear and consistently visible separation or 2) different origin or insertion. Visibility of each of the levator ani subdivisions in each scan plane was assessed in 25 nulliparous women. In the axial plane, the puborectal muscle can be seen lateral to the pubovisceral muscle and decussating dorsal to the rectum. The course of the puboperineal muscle near the perineal body is visualized in the axial plane. The coronal view is perpendicular to the fiber direction of the puborectal and pubovisceral muscles and shows them as “clusters” of muscle on either side of the vagina. The sagittal plane consistently demonstrates the puborectal muscle passing dorsal to the rectum to form a sling that can consistently be seen as a “bump.” This plane is also parallel to the pubovisceral muscle fiber direction and shows the puboperineal muscle. The subdivisions of the levator ani muscle are visible in MRI scans, each with distinct morphology and characteristic features. Funding:
|
Virtual Cystoscopy - A Surgical Planning and Guidance Tool
|
Publication: Arch Ital Urol Androl. 2006 Mar;78(1):23-4. PMID: 16752884 Authors: Braticevici B, Onu M, Bengus F. Institution: Clinical Hospital, Bucharest, Romania. Background/Purpose: Image guided-surgery systems facilitates surgical planning phases of endoscopic procedures. In this paper, we used a software package for 3D surface model generation and vizualization of the urinary bladder, based on magnetic resonance (MR) cross sectional images of the pelvis. The patients group consisted in 6 patients diagnosed with urinary bladder tumor. They were submitted to MRI exam. Twelve consecutive cross sectional images of the pelvis were aquired (TR (repetition time) = 600 msec, TE (echo time) = 19 msec, slice thickness = 6 divided by 7 mm, FOV (field of view) = 36 cm. All these images were transferred to a personal computer running the 3D Slicer software. We obtained, for each patient, a 3D model of the pelvis including the urinary bladder. In This way, the surgical enviroment was simulated and we are able to investigate the bladder by virtual cystoscopy. The virtual endoscopy may be used as a tool in the preoperative training and in surgical planning. |
Measurement of the Pubic Portion of the Levator Ani Muscle in Women with Unilateral Defects in 3D Models from MR Images
|
Publication: Int J Gynaecol Obstet. 2006 Mar;92(3):234-41. PMID: 16442111 | PDF Authors: Chen L, Hsu Y, Ashton-Miller JA, DeLancey JO. Institution: Department of Biomedical Engineering, University of Michigan, Ann Arbor, MI, USA. Background/Purpose: Develop a method to quantify the cross-sectional area of the pubic portion of the levator ani muscle, validate the method in women with unilateral muscle defects, and report preliminary findings in those women. Multi-planar proton density magnetic resonance images of 12 women with a unilateral defect in the pubic portion of their levator ani were selected from a larger study of levator ani muscle anatomy in women with and without genital prolapse. Three-dimensional bilateral models of the levator ani were reconstructed, using 3D Slicer v.2.1b1, and divided into iliococcygeal and pubic portions. Muscle cross-sectional areas were calculated at four equally spaced locations perpendicular to a line drawn from the pubic origin to the visceral insertion using the I-DEAS computer modeling software. The cross-sectional area of the muscle on the side with the defect was smaller than the normal side at all the four locations. The average bilateral difference was up to 81% at location 1 (nearest pubic origin). Almost all of the volume difference (13.7%, P=0.0004) was attributable to a reduction in the pubic portion (24.6%, P<0.0001), not the iliococcygeal portion (P=0.64), of the muscle. A method was developed to quantify cross-sectional area of the pubic portion of the levator ani perpendicular to the intact muscle direction. Significant bilateral cross-sectional area differences were found between intact and defective muscles in women with a unilateral defect. Funding:
|
Finite-element-method (FEM) Model Generation of Time-resolved 3D Echocardiographic Geometry Data for Mitral-valve Volumetry
|
Publication: Biomed Eng Online. 2006 Mar 3;5:17. PMID: 16512925 | PDF Authors: Verhey JF, Nathan NS, Rienhoff O, Kikinis R, Rakebrandt F, D'Ambra MN. Institution: MVIP ImagingProducts GmbH, Nörten-Hardenberg, Germany. Background/Purpose: Mitral Valve (MV) 3D structural data can be easily obtained using standard transesophageal echocardiography (TEE) devices but quantitative pre- and intraoperative volume analysis of the MV is presently not feasible in the cardiac operation room (OR). Finite element method (FEM) modeling is necessary to carry out precise and individual volume analysis and in the future will form the basis for simulation of cardiac interventions. Methods: With the present retrospective pilot study we describe a method to transfer MV geometric data into 3D Slicer 2 software, an open-source medical visualization and analysis software package. A newly developed software program (ROIExtract) allowed selection of a region-of-interest (ROI) from the TEE data and data transformation for use in 3D Slicer. FEM models for quantitative volumetric studies were generated. ROI selection permitted the visualization and calculations required to create a sequence of volume rendered models of the MV allowing time-based visualization of regional deformation. Quantitation of tissue volume, especially important in myxomatous degeneration can be carried out. Rendered volumes are shown in 3D as well as in time-resolved 4D animations. The visualization of the segmented MV may significantly enhance clinical interpretation. This method provides an infrastructure for the study of image guided assessment of clinical findings and surgical planning. For complete pre- and intraoperative 3D MV FEM analysis, three input elements are necessary: 1. time-gated, reality-based structural information, 2. continuous MV pressure and 3. instantaneous tissue elastance. The present process makes the first of these elements available. Volume defect analysis is essential to fully understand functional and geometrical dysfunction of but not limited to the valve. 3D Slicer was used for semi-automatic valve border detection and volume-rendering of clinical 3D echocardiographic data. FEM based models were also calculated. A Philips/HP Sonos 5500 ultrasound device stores volume data as time-resolved 4D volume data sets. Data sets for three subjects were used. Since 3D Slicer does not process time-resolved data sets, we employed a standard movie maker to animate the individual time-based models and visualizations. Calculation time and model size were minimized. Pressures were also easily available. We speculate that calculation of instantaneous elastance may be possible using instantaneous pressure values and tissue deformation data derived from the animated FEM. Funding:
|
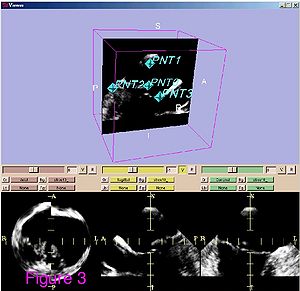 Ultrasound data of after preprocessing. The ultrasound data are shown from patient 1. Shown is a standard visualization of one time step during the heart cycle with 3D Slicer software. The three planes for each spatial direction are shown in the lower three frames. In the frame above one plane is shown together with the set of four fiducials. These four points are defined for all time steps. |
Range of Curvilinear Distraction Devices Required for Treatment of Mandibular Deformities
|
Publication: J Oral Maxillofac Surg. 2006 Feb;64(2):259-64. PMID: 16413898 | PDF Authors: Ritter L, Yeshwant K, Seldin EB, Kaban LB, Gateno J, Keeve E, Kikinis R, Troulis MJ. Institution: Department of Oral and Maxillofacial Surgery, Massachusetts General Hospital, Boston, MA, USA. Background/Purpose: The purpose of this study was to determine the range of fixed trajectory curvilinear distraction devices required to correct a variety of severe mandibular deformities. Preoperative computed tomography (CT) scans from 18 patients with mandibular deformities were imported into a CT-based software program (Osteoplan). Three-dimensional virtual models of the individual skulls were made with landmarks to track movements. An ideal treatment plan was created for each patient. Upper and lower boundaries for the dimensions of curvilinear distractors were established based on manufacturing and geometric constraints. Then, anatomically acceptable distractor attachment points were identified on the models using proximal and distal grids. Treatment plans were simulated for a series of distractors with varying radii of curvature, elongations (arc-length of device), and placements along the grids. The outcomes using these distractors were compared with the ideal treatment plans. Discrepancies were quantified in millimeters by comparing landmarks in the simulated versus ideal movements. Approximately 400,000 simulated 3-dimensional movements, based on the distractor parameters and variations in placement were computationally evaluated for the 18 cases. It was determined that, by varying distractor placement, a family of 5 distractors, with 3, 5, 7, and 10 cm radii of curvature and a straight-line device, could be used to treat all 18 cases to within 1.8 mm of error. The results of this study indicate that a family of 5 curvilinear distractors may suffice to treat a broad range of mandibular deformities. Funding:
|
Preliminary Study on Digitized Nasal and Temporal Bone Anatomy
|
Publication: Clin Anat. 2006 Jan;19(1):32-6. PMID: 16283638 | PDF Authors: Li XP, Han DM, Xia Y, Zhou GH. Institution: ENT Department, Beijing Tongren Hospital Affiliated with Capital University of Medical Sciences, Beijing, China. Background/Purpose: The purpose of this study was to explore a feasible method for the reconstruction of the nasal and temporal bone structures of the Chinese virtual human project and provide a more accurate and facilitated way view them three-dimensionally (3D). The 3D Slicer software was used to reconstruct the anatomic structures of the human nose and temporal bone. Segmentation and extraction of the contours of the ROI (region of interest) in each single slice were conducted and the processed volume data was transferred into the 3D Slicer. After resegmentation, a set of labeled maps of the ROI were produced. Based on these maps, the 3D surface models of the tissues of interest were constructed. Four groups of paranasal sinuses, nasal septa, middle and inferior turbinates, temporal bones, tympanic cavities, mastoid air cells, sigmoid sinuses, and internal carotid arteries were reconstructed successfully. These models show spatial relationships and orientation between them. The results show that the 3D Slicer may be used for the 3D visualization of parts of anatomic structures in the nose and temporal bone based on the first Chinese virtual human data, and thus, can facilitate the observation and understanding of the anatomic structures in this area. Funding:
|
Developmental Response to Cold Stress in Cranial Morphology of Rattus: Implications for the Interpretation of Climatic Adaptation in Fossil Hominins
|
Publication: Proceedings of the Royal Society B: Biological Sciences 2006; 273:2605-10. | PDF Authors: Rae TC, Viðarsdottir US, Jeffery N, Steegmann AT Jr. Institution: Evolutionary Anthropology Research Group, Department of Anthropology, University of Durham, UK. Background/Purpose: Adaptation to climate occupies a central position in biological anthropology. The demonstrable relationship between temperature and morphology in extant primates (including humans) forms the basis of the interpretation of the Pleistocene hominin Homo neanderthalensis as a cold-adapted species. There are contradictory signals, however, in the pattern of primate craniofacial changes associated with climatic conditions. To determine the direction and extent of craniofacial change associated with temperature, and to understand the proximate mechanisms underlying cold adaptations in vertebrates in general, dry crania rom previous experiments on cold- and warm-reared rats were investigated using computed tomography scanning and three-dimensional digitization of cranial landmarks. Aspects of internal and external cranial morphology were compared using standard statistical and geometric morphometric techniques. The results suggest that the developmental response to cold stress produces subtle but significant changes in facial shape, and a relative decrease in the volume of the maxillary sinuses (and nasal cavity), both of which are independent of the size of the skull or postcranium. These changes are consistent with comparative studies of temperate climate primates, but contradict previous interpretations of cranial morphology of Pleistocene Hominini. |
A Ceratopsid Dinosaur Parietal from New Mexico and Its Implications for Ceratopsid Biogeography and Systematics
|
Publication: Journal of Vertebrate Paleontology 2006; 26:1018-20. | PDF Authors: Farke AA, Williamson TE. Institution: Department of Anatomical Sciences, Stony Brook University, NY, USA. Background/Purpose: Ceratopsid (horned dinosaur) cranial material is relatively common in the Upper Cretaceous Naashoibito Member of the Kirtland Formation, San Juan Basin, New Mexico. However, the specimens are fragmentary, making identification problematic. Previously, it has been suggested that the Naashoibito specimens represent Torosaurus utahensis, a chasmosaurine taxon originally known from the North Horn Formation of Utah. This identification has been used to support a Lancian age for the Naashoibito Member and the Alamo Wash local fauna of the Kirtland Formation (e.g., Lehman, 1981; Lucas et al., 1987). Others (e.g., Lehman, 1990) have synonomized T. utahensis with Torosaurus latus, a taxon otherwise known only from the late Maastrichtian Lance and Hell Creek formations. Recent work has upheld the validity of T. utahensis (Sullivan et al., 2005). However, Sullivan and colleagues (2005) have also argued that no previously described ceratopsid specimens from the Naashoibito Member are identifiable beyond the level of Chasmosaurinae indeterminate and therefore are not useful for assessing biostratigraphic correlations and ceratopsid biogeography. Here we describe a partial chasmosaurine ceratopsid parietal from the Naashoibito Member of the Kirtland Formation. Although other fragmentary parietals have been recovered from this unit (e.g., Lehman, 1981; Lucas et al., 1987), the new specimen exhibits unusual morphology: an epoccipital element positioned along the midline. This feature has previously been reported only in Triceratops, a taxon not known from south of the Denver Basin. The occurrence of such a feature in a ceratopsid from New Mexico has implications for ceratopsian systematics and biogeography. Funding:
|
2005
Magnetic Resonance Imaging and 3-Dimensional Analysis of External Anal Sphincter Anatomy
|
Publication: Obstet Gynecol. 2005 Dec;106(6):1259-65. PMID: 16319250 | PDF Authors: Hsu Y, Fenner DE, Weadock WJ, DeLancey JO. Institution: Pelvic Floor Research Group, Division of Gynecology, Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor, MI, USA. Background/Purpose: To use magnetic resonance images of living women and 3-dimensional modeling software to identify the component parts and characteristic features of the external anal sphincter (EAS) that have visible separation or varying origins and insertions. Methods: Detailed structural analysis of anal sphincter anatomy was performed on 3 pelvic magnetic resonance imaging (MRI) data sets selected for image clarity from ongoing studies involving nulliparous women. The relationships of anal sphincter structures seen in axial, sagittal, and coronal planes were examined using the 3D Slicer 2.1b1 software package. The following were requirements for sphincter elements to be considered separate: 1) a clear and consistently visible separation or 2) a different origin or insertion. The characteristic features identified in this way were then evaluated in images from an additional 50 nulliparas for the frequency of feature visibility. There were 3 components of the EAS that met criteria as being "separate" structures. The main body (EAS-M) is separated from the subcutaneous external anal sphincter (SQ-EAS) by a clear division that could be observed in all (100%) of the MRI scans reviewed. The wing-shaped end (EAS-W) has fibers that do not cross the midline ventrally, but have lateral origins near the ischiopubic ramus. This EAS-W component was visible in 76% of the nulliparas reviewed. Three distinct external anal sphincter components can be identified by MRI in the majority of nulliparous women. Funding:
|
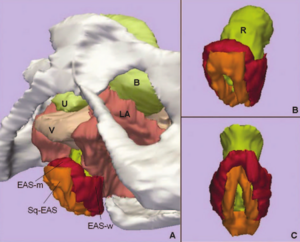 A. Inferior, left three-quarter view of model showing relationship of external anal sphincter complex to the bones and pelvic organs. B. Inferior, left three-quarter view of the external anal sphincter complex. External anal sphincter is in red; note the lateral wing portion of the external anal sphincter. Subcutaneous external anal sphincter is in orange. C. Posterior view of the external anal sphincter complex showing the circumferential nature of both the external anal sphincter and the subcutaneous external anal sphincter. U, urethra; B, bladder; V, vagina; LA, levator ani muscle; R, Rectum; EAS-M, main body of external anal sphincter; EAS-W, lateral wing portion of the external anal sphincter; SQ-EAS, subcutaneous external anal sphincter. |
Group-Slicer: A Collaborative Extension of 3D Slicer
|
Publication: J Biomed Inform. 2005 Dec;38(6):431-42. PMID: 16337568 | PDF Authors: Simmross-Wattenberg F, Carranza-Herrezuelo N, Palacios-Camarero C, Casaseca-de-la-Higuera P, Martín-Fernández MA, Aja-Fernández S, Ruiz-Alzola J, Westin C-F, Alberola-López C. Institution: Laboratorio de Procesado de Imagen, ETSI Telecomunicacion, Universidad de Valladolid, Valladolid, Spain. Background/Purpose: In this paper, we describe a first step towards a collaborative extension of the well-known 3D Slicer; this platform is nowadays used as a standalone tool for both surgical planning and medical intervention. We show how this tool can be easily modified to make it collaborative so that it may constitute an integrated environment for expertise exchange as well as a useful tool for academic purposes. Funding:
|
2D Rigid Registration of MR Scans using the 1D Binary Projections
|
Publication: Enformatika Transactions on Engineering, Computing and Technology, November 2005; 9:157-61. | PDF Author: Panos D. Kotsas Institution: Department of Automated Control and System Engineering, University of Sheffield, UK. Background/Purpose: This research deals with the application of a signal intensity independent registration criterion for 2D rigid body registration of medical images using 1D binary projections. The criterion is defined as the weighted ratio of two projections. The ratio is computed on a pixel per pixel basis and weighting is performed by setting the ratios between one and zero pixels to a standard high value. The mean squared value of the weighted ratio is computed over the union of the one areas of the two projections and it is minimized using the Chebyshev polynomial approximation using n=5 points. The sum of x and y parallel projections is used for translational adjustment and a range of parallel projections between 40-50 deg (depending on the orientation of the image) for rotational adjustment. MR-MR registration experiments were performed and gave mean errors well below 1deg and 1 pixel (0.12 deg and 0.47 pixels for the example given in Enformatika Publication). The method is to be extended for surface matching. |
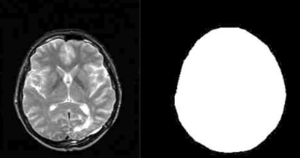 T2 MR scan (contrast enhanced) and mask created with 3D Slicer software |
Preoperative Hepatic 3D Models: Virtual Liver Resection using Three-dimensional Imaging Technique
|
Publication: Eur J Radiol. 2005 Nov;56(2):179-84. PMID: 15890482 Authors: Numminen K, Sipilä O, Mäkisalo H. Institution: Helsinki Medical Imaging Center, Department of Radiology, Helsinki University Central Hospital, Helsinki, Finland. Background/Purpose: Emerging new techniques for liver resections set new requirements for the preoperative imaging and planning. Open surgery is a three-dimensional procedure and planning of the resection line may be difficult when basing on conventional two-dimensional CTs or MRIs, although all the information is there. With multidetector-row CT (MDCT), thin slices can be obtained with excellent temporal resolution, and precise three-dimensional (3D) models can be created. We regard 3D imaging technique useful in most liver resections. It improves the surgeon's knowledge of liver anatomy and makes even more complicated liver resections safe. Better knowledge of three-dimensional appearances of liver structures may further improve the results of curative liver surgery. However, before becoming a routine clinical procedure, research and development are still needed. Also, careful testing and evaluation of the methods have to be performed. In the future, 3D models will probably play an important role in the preoperative planning of liver resections. |
 A 76-year-old man with hepatocellular carcinoma. MDCT image shows large tumor in liver segments 5-8 (a). Semi-automatic segmentation based on thresholding, morphological operations and connected component labelling is utilized to create a triangulated surface model. Segmented structures can be visualized with different colors and opacities. 3D model from portal veins (b), from hepatic veins (c), liver tumor (d) and liver parenchyma (e). The model can be studied freely from any direction on the computer screen (f). Resection line is configured immediately right to the middle hepatic vein (g). Vessels crossing the resection line can be visualized and easily found when performing right-sided lobectomy (h). |
Three-dimensional Reconstruction and Volumetry of Intracranial Haemorrhage and its Mass Effect
|
Publication: Neuroradiology. 2005 Jun;47(6):417-24. PMID: 15856213 | PDF Authors: Strik HM, Borchert H, Fels C, Knauth M, Rienhoff O, Bähr M, Verhey JF. Institution: Department of Neurology, Medical School, University of Göttingen, Germany. Background/Purpose: Intracerebral haemorrhage still causes considerable disability and mortality. The studies on conservative and operative management are inconclusive, probably due to inexact volumetry of the haemorrhage. We investigated whether three-dimensional (3D), voxel-based volumetry of the haemorrhage and its mass effect is feasible with routine computed tomography (CT) scans. The volumes of the haemorrhage, ventricles, midline shift, the intracranial volume and ventricular compression in CT scans of 12 patients with basal ganglia haemorrhage were determined with the 3D Slicer software. Indices of haemorrhage and intracranial or ventricular volume were calculated and correlated with the clinical data. The intended measures could be determined with an acceptable intra-individual variability. The 3D volumetric data tended to correlate better with the clinical course than the conventionally assessed distance of midline shift and volume of haemorrhage. 3D volumetry of intracranial haemorrhage and its mass effect is feasible with routine CT examination. Prospective studies should assess its value for clinical studies on intracranial space-occupying diseases. |
Vaginal Thickness, Cross-Sectional Area, and Perimeter in Women with and Those without Prolapse
|
Publication: Obstet Gynecol. 2005 May;105(5 Pt1):1012-7. PMID: 15863538 | PDF Authors: Hsu Y, Chen L, Delancey JO, Ashton-Miller JA. Institution: Division of Gynecology, Department of Obstetrics and Gynecology, University of Michigan Medical School, Ann Arbor, MI, USA. Background/Purpose: Use axial magnetic resonance imaging to test the null hypothesis that no difference exists in apparent vaginal thickness between women with and those without prolapse. Magnetic resonance imaging studies of 24 patients with prolapse at least 2 cm beyond the introitus were selected from an ongoing study comparing women with prolapse with normal control subjects. The magnetic resonance scans of 24 women with prolapse (cases) and 24 women without prolapse (controls) were selected from those of women of similar age, race, and parity. The magnetic resonance files were imported into an experimental modeling program, and 3-dimensional models of each vagina were created. The minimum transverse plane cross-sectional area, mid-sagittal plane diameter, and transverse plane perimeter of each vaginal model were calculated. Neither the mean age (cases 58.6 years ± standard deviation [SD] 14.4 versus controls 59.4 years ± SD 13.2) nor the mean body mass index (cases 24.1 kg/m2± SD 3.3, controls 25.7 kg/m2± SD 3.7) differed significantly between groups. Minimum mid-sagittal vaginal diameters did not differ between groups. Patients with prolapse had larger minimum vaginal cross-sectional areas than controls (5.71 cm2± standard error of the mean [SEM] 0.25 versus 4.76 cm2± SEM 0.20, respectively; P = .005). The perimeter of the vagina was also larger in the prolapse group (11.10 cm ± SEM 0.24) compared with controls (9.96 cm ± SEM 0.22) P = .001. Subgroup analysis of patients with endogenous or exogenous estrogen showed prolapse patients had larger vaginal cross-sectional area (P = .030); in patients without estrogen group differences were not significant (P = .099). Vaginal thickness is similar in women with and those without pelvic organ prolapse. The vaginal perimeter and cross-sectional areas are 11% and 20% larger in prolapse patients, respectively. Estrogen status did not affect differences found between groups. Funding:
|
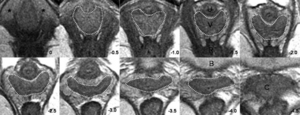 Axial slices at 5-mm intervals arranged caudal to cephalad starting from the image in the upper left (image 0). Vaginal tracings were made from above the level of the vestibular bulbs (VB), represented by asterisks (*), caudally (image 0) to below where the cervix (C) could be seen (image -4.0). U, urethra; V, vagina; R, rectum; B, bladder. |
Registration and Fusion of CT and MRI of the Temporal Bone
|
Publication: J Comput Assist Tomogr. 2005 May-Jun;29(3):305-10. PMID: 15891495 | PDF Authors: Bartling S, Peldschus K, Rodt T, Kral F, Matthies H, Kikinis R, Becker H. Institution: Department of Neuroradiology, Hannover Medical School, Hannover, Germany. Background/Purpose: CT and MRI of the skull base and the Temporal provides complimentary information. A registration and fusion of CT and MRI may improve diagnosis, because features only seen in one modality can be assessed with respect to the information gathered from the other modality. A manual, rigid registration method - basically overlaying two volumes in one space - as implemented in 3D Slicer was used. Threshold based fusion methods resulted in MRI overlaying co-registered CT. Landmarks have been used to assess target registration error - registration accuracy was within the range of the voxel size of either modality. A range of different pathological conditions was used to demonstrate the potential benefits of this methods. |
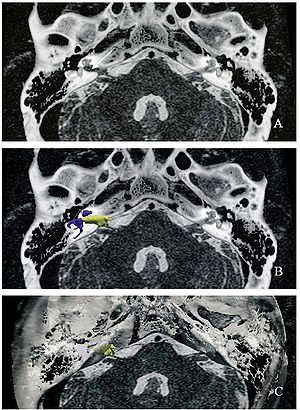 Acoustic schwannoma in the right internal auditory canal (arrow) in registered and fused CT and MRI of the temporal bone. For surgical planning, the MRI-given tumor (yellow) and critical CT-given surgical landmarks such as the labyrinth (blue) and the facial nerve canal (gray) as well as the bony skull base (white) can be displayed together. |
Open-configuration MR-guided Microwave Thermocoagulation Therapy for Metastatic Liver Tumors from Breast Cancer]
|
Publication: Breast Cancer. 2005;12(1):26-31. PMID: 15657520 | PDF Authors: Abe H, Kurumi Y, Naka S, Shiomi H, Umeda T, Naitoh H, Endo Y, Hanasawa K, Morikawa S, Tani T. Institution: Division of General Surgery, Department of Surgery, Shiga University of Medical Science, Seta-Tsukinowa, Otsu, Shiga, Japan. Background/Purpose: Liver metastases from breast cancer are associated with a poor prognosis, however, local control with microwave thermocoagulation therapy has been used in certain subgroups of these patients in the past decade. In this study, open-configuration magnetic resonance (MR) -guided microwave thermocoagulation therapy was used for metastatic liver tumors from breast cancer, and the efficacy of this treatment was assessed. Methods: Between June 2000 and April 2004, we used MR-guided microwave thermocoagulation therapy on 11 nodules in 8 patients with metastatic liver tumors from breast cancer. The procedure was carried out under general anesthesia. A 0.5 T open-configuration MR system and a microwave coagulator were used. Near-real-time MR images and real-time temperature images were collected and displayed on the monitor. The MR-compatible thoracoscope was used and combined with MR imaging guidance. Navigation software, a 3D Slicer, was installed and customized. The customized navigation software displayed near-real-time MR images. The percutaneous puncture into the tumors was successful in all cases. No mortality or major complications occurred as a result of the procedures. Five of the 8 patients are alive with new metastatic foci with a mean observation period of 25.9 months. We developed several devices to allow safe, easy, and accurate MR-guided microwave thermocoagulation therapy of liver tumors. Open-configuration MR-guided microwave thermocoagulation therapy appears to be a feasible method for tumor ablation of metastatic liver tumors from breast cancer. |
Quantification of Airway Diameters and 3D Airway Tree Rendering from Dynamic Hyperpolarized 3He Magnetic Resonance Imaging
|
Publication: Magn Reson Med. 2005 Feb;53(2):474-8. PMID: 15678546 | PDF Authors: Lewis TA, Tzeng YS, McKinstry EL, Tooker AC, Hong K, Sun Y, Mansour J, Handler Z, Albert MS. Institution: Brigham and Womem's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: As another step toward extracting quantitative information from hyperpolarized 3He MRI, airway diameters in humans were measured from projection images and multislice images of the lungs. Values obtained were in good agreement with the Weibel lung morphometry model. The measurement of airway caliber can now be achieved without the use of ionizing radiation. Furthermore, it was demonstrated that 3D airway tree renderings could be constructed from the multislice data. Both the measurement of airway diameters and the rendering of 3D airway information hold promise for the clinical assessment of bronchoconstrictive diseases such as asthma and the associated evaluation of treatment effectiveness. Work is being done to address the uncertainties of the manually intensive methods we have developed. Funding:
|
 Airway tree constructed from stacking dynamic multislice data sets in 3D Slicer. |
A Finite Element Method Model to Simulate Laser Interstitial Thermo Therapy in Anatomical Inhomogeneous Regions
|
Publication: Biomed Eng Online. 2005 Jan 4;4(1):2. PMID: 15631630 | PDF Authors: Mohammed Y, Verhey JF. Institution: Department of Medical Informatics, University of Goettingen, Goettingen, Germany. Background/Purpose: Laser Interstitial ThermoTherapy (LITT) is a well established surgical method. The use of LITT is so far limited to homogeneous tissues, e.g. the liver. One of the reasons is the limited capability of existing treatment planning models to calculate accurately the damage zone. The treatment planning in inhomogeneous tissues, especially of regions near main vessels, poses still a challenge. In order to extend the application of LITT to a wider range of anatomical regions new simulation methods are needed. The model described with this article enables efficient simulation for predicting damaged tissue as a basis for a future laser-surgical planning system. Previously we described the dependency of the model on geometry. With the presented paper including two video files we focus on the methodological, physical and mathematical background of the model. |
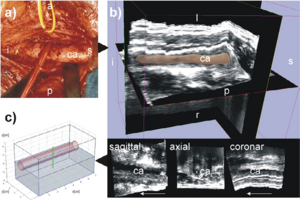 The geometry used. The left carotid artery is shown in this figure labelled with ca. The following letters indicate the orientation: s for superior, i for inferior, p for posterior, a for anterior, l for left, r for right. (a) is a photo of the human anatomy in the neck area. The carotid artery is shown here after moving the vein to the cranial direction. (b) shows the corresponding freehand 3D ultrasound dataset of the human neck region acquired axially. The 3D image in the top of (b) shows the 3D ultrasound volume together with the carotid artery segmented with 3D Slicer software [17]. The 3D model is displayed with 40% transparency. (c) displays the model used in the simulation approximated according to the geometry of the human neck shown in (a) and (b). The segmentation of the 3D ultrasound dataset in (b), is available as a video stream, too, showing the geometry of the carotid artery. |
The Application of DTI to Investigate White Matter Abnormalities in Schizophrenia
|
Publication: Ann. N.Y. Acad. Sci. 2005; 1064:134-48. PMID: 16394153 | PDF Authors: Kubicki M, Westin C-F, McCarley RW, Shenton ME. Institution: Clinical Neuroscience Division, Laboratory of Neuroscience, Boston VA Healthcare System–Brockton Division, Department of Psychiatry, Harvard Medical School, Brockton, MA, USA. Background/Purpose: Schizophrenia is a serious and disabling mental disorder that affects approximately 1% of the general population, with often devastating effects on the psychological and financial resources of the patient, family, and larger community. The etiology of schizophrenia is not known, although it likely involves several interacting biological and environmental factors that predispose an individual to schizophrenia. However, although the underlying pathology remains unknown, it has been believed that brain abnormalities would ultimately be linked to the etiology of schizophrenia. This theory was rekindled in the 1970s, when the first computer-assisted tomography (CT) study showed enlarged lateral ventricles in schizophrenia. Since that time, there have been many improvements in MR acquisition and image processing, including the introduction of positron emission tomography (PET), followed by functional MR (fMRI), and diffusion tensor imaging (DTI). These advances have led to an appreciation of the critical role that brain abnormalities play in schizophrenia. While structural MRI has proven to be useful in investigating and detecting gray matter abnormalities in schizophrenia, the investigation of white matter has proven to be more challenging as white matter appears homogeneous on conventional MRI and the fibers connecting different brain regions cannot be appreciated. With the development of DTI, we are now able to investigate white matter abnormalities in schizophrenia. Funding:
|
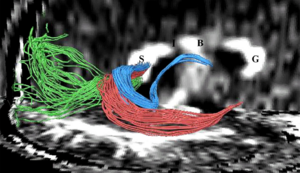 Fibers traveling through the splenium of the corpus callosum are shown, where fibers connecting the left and right occipital lobe are displayed in green, fibers interconnecting lateral temporal regions are displayed in red, and fibers connecting medial temporal regions are displayed in blue. Additionally, the genu of the corpus callosum is labeled as “G”, the body as “B”, the isthmus as “I”, and the splenium as “S”. |
2004
A Statistically Based Flow for Image Segmentation
|
Publication: Med Image Anal. 2004 Sep;8(3):267-74. PMID: 15450221 | PDF Authors: Pichon E, Tannenbaum A, Kikinis R. Institution: School of Electrical & Computer Engineering, Georgia Institute of Technology, Atlanta, GA, USA. Background/Purpose: In this paper we present a new algorithm for 3D medical image segmentation. The algorithm is versatile, fast, relatively simple to implement, and semi-automatic. It is based on minimizing a global energy defined from a learned non-parametric estimation of the statistics of the region to be segmented. Implementation details are discussed, and source code is freely available as part of the 3D Slicer project. In addition, a new unified set of validation metrics is proposed. Results on artificial and real MRI images show that the algorithm performs well on large brain structures both in terms of accuracy and robustness to noise. Funding:
|
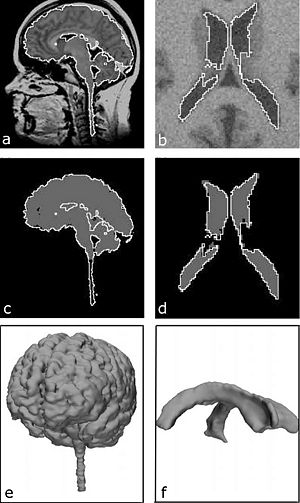 Results on real and noisy simulated datasets (left and right respectively): (a) sagittal slice of real dataset and proposed segmentation (WM GM); (b) axial slice of artificial dataset and proposed segmentation (ventricle); (c) expert segmentation (gray) and proposed segmentation (white); (d) underlying ground truth (gray) and proposed segmentation (white); (e) rendered surface of proposed segmentation (WM GM); (f) rendered surface of proposed segmentation (ventricle). |
Decreases in Ventricular Volume Correlate with Decreases in Ventricular Pressure in Idiopathic Normal Pressure Hydrocephalus Patients Who Experienced Clinical Improvement after Implantation with Adjustable Valve Shunts
|
Publication: Neurosurgery. 2004 Sep;55(3):582-92. PMID: 15335425 | PDF Authors: McConnell KA, Zou KH, Chabrerie AV, Bailey NO, Black PM. Institution: Department of Neurosurgery, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: This retrospective study examined whether changes in ventricular volume correspond with changes in adjustable valve pressure settings in a cohort of patients who received shunts to treat idiopathic normal pressure hydrocephalus. We also examined whether these pressure-volume curves and other patient variables would co-occur with a positive clinical response to shunting. Methods: We selected 51 patients diagnosed with idiopathic normal pressure hydrocephalus who had undergone implantation of a Codman Hakim programmable valve (Medos S.A., Le Locle, Switzerland). Clinical data were gathered from the patients. Funding:
|
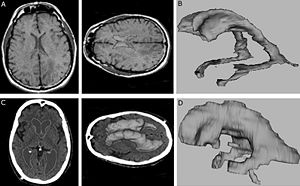 3D Slicer software segmentation of the ventricular system of a subject without hydrocephalus (A) used to produce the three-dimensional model of a normal, nonhydrocephalic ventricular system (B). C and D, 3D Slicer software segmentation of the ventricular system of a subject with INPH (C) used to produce the three-dimensional model of a hydrocephalic ventricular system (D). |
Spatial Motion Constraints in Medical Robot using Virtual Fixtures Generated by Anatomy
|
Publication: Proceedings of the 2004 IEEE International Conference on Robotics & Automation, ICRA 2004. | PDF Authors: Li M, Taylor RH. Institution: Department of Computer Science, NSF Engineering Research Center for Computer Integrated Surgical Systems and Technology, Johns Hopkins University, Baltimore, MD, USA. Background/Purpose: In Ear, Nose and Throat (ENT) surgery, the operating volume is very limited. This is especially true in sinus surgery, when the instrument passes through the nasal and sinus cavity to reach the pathological area. The nasal and sinus bones impose geometric constraints on the work volume. During the surgery, the surgeon needs to control the motion of the instrument tip to accomplish some delicate procedure; meanwhile he/she needs to avoid hitting anatomic constraints. In this paper, we present a method to assist the path following task in a constrained area. The system reads the user’s force input and combines it with the planned tip-trajectory to create the tip motion constraints; meanwhile it generates the tool-shaft boundary constraints based on a 3D geometric model. We map instrument tip motion and boundary information to joint displacements via robot kinematics, and then use a constrained quadratic optimization algorithm to compute the optimal set of corresponding joint displacements. In the preliminary study, we show that robot guidance using cooperative control and virtual fixtures derived from complex geometry can assist users in skilled manipulation tasks, while maintaining desirable properties such as collision avoidance and safety. Funding:
|
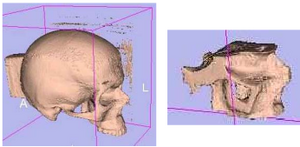 3D Slicer surface models of test phantom. (left) whole skull surface model and, (right) the model of nasal cavity portion used to generate constraints |
Clinical Validation of the Normalized Mutual Information Method for Registration of CT and MR Images in Radiotherapy of Brain Tumors
|
Publication: J Appl Clin Med Phys. 2004 Summer;5(3):66-79. PMID: 15753941 | PDF Authors: Veninga T, Huisman H, van der Maazen RW, Huizenga H. Institution: Department of Radiation Oncology, University Medical Center Nijmegen, The Netherlands. Background/Purpose: Image registration integrates information of different imaging modalities and has the potential to improve target volume determination in radiotherapy planning. This paper describes the implementation and validation of a 3D fully automated registration procedure in the process of radiotherapy treatment planning of brain tumors. 15 Patients with various brain tumors received CT and MR brain imaging before the start of radiotherapy. The normalized mutual information (NMI) method was used for image registration. Registration accuracy was estimated by performing statistical analysis of coordinate differences between CT and MR anatomical landmarks along the x-, y- and z-axes. Second, a visual validation protocol was developed to validate the quality of individual registration solutions and this protocol was tested in a series of 36 CT-MR registration procedures with intentionally applied registration errors. The mean coordinate differences between CT and MR landmarks along the x- and y-axes were in general within 0.5 mm. The mean coordinate differences along the z-axis were within 1.0 mm, which is of the same magnitude as the applied slice thickness in scanning. Second, the detection of intentionally applied registration errors by employment of a standardized visual validation protocol resulted in low false-negative and low false-positive rates. Application of the NMI method for the brain results in excellent automatic registration accuracy and the method has been incorporated in daily routine within our institute. A standardized validation protocol is proposed that ensures the quality of individual registrations by detecting registration errors with high sensitivity and specificity. This protocol is proposed for the validation of other linear registration methods. |
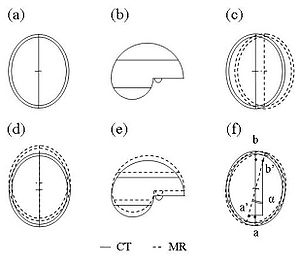 For the purpose of individual quality assurance (QA) of image registration, an independent visual validation protocol was developed, using 3D Slicer, a freely available software program for visualization and processing of medical data. All image data were transferred to 3D Slicer in DICOM format. The validation protocol consists of a stepwise procedure for an estimate of translation errors along the three orthogonal axes (Trx, Try, and Trz) as well as rotation errors around these three axes (Rx, Ry, and Rz). |
Diffusion-tensor Imaging–guided Tracking of Fibers of the Pyramidal Tract Combined with Intraoperative Cortical Stimulation Mapping in Patients with Gliomas
|
Publication: J Neurosurg. 2004 Jul;101(1):66-72. PMID: 15255253 | PDF Authors: Berman JI, Berger MS, Mukherjee P, Henry RG. Institution: Department of Radiology, University of California at San Francisco, CA, USA. Background/Purpose: The goal of this study was to use diffusion-tensor (DT) magnetic resonance (MR) imaging to track fibers combined with cortical stimulation mapping to delineate descending motor pathways. Subcortical localization of motor path-ways in relation to a glioma may provide critical information to guide tumor resection and prevent surgical morbidity. Methods: Eleven adult patients harboring gliomas underwent MR imaging 1 day prior to image-guided intraoperative cortical motor mapping and tumor resection. Screens depicting 27 cortical motor sites on a surgical navigation system were saved to launch DT imaging of fiber tracks of descending motor pathways. The position and organization of motor tracts were visualized by fiber tracking. Tracks from 16 motor stimulation sites followed descending pathways from the precentral gyrus, through the corona radiata and internal capsule, and into the cerebral peduncle. These tracks were also observed on DT images to diverge along crossing white matter bundles (four patients) and to terminate or deviate in regions of peritumoral vasogenic edema (five patients). The use of precise intraoperative cortical mapping information and DT images of fiber tracks can reveal the course of motor pathways beneath the cortex. The subcortical fiber tracks generated are consistent with the known anatomical course and somatotopic organization of the motor tract in relation to its cortical origins. Tracking fibers by using DT imaging in combination with functional localization has the potential to reduce surgical morbidity by revealing subcortical connections of the functional cortex. Funding:
|
Abnormal Association Between Reduced Magnetic Mismatch Field to Speech Sounds and Smaller Left Planum Temporale Volume in Schizophrenia
|
Publication: NeuroImage 2004; 22:720-7. PMID: 15193600 | PDF Authors: Yamasue H, Yamada H, Yumoto M, Kamio S, Kudo N, Uetsuki M, Abe O, Fukuda R, Aoki S, Ohtomo K, Iwanami A, Kato N, Kasai K. Institution: Department of Neuropsychiatry, Graduate School of Medicine, University of Tokyo, Bunkyo, Tokyo, Japan. Background/Purpose: Schizophrenia is associated with language-related dysfunction. A previous study [Schizophr. Res. 59 (2003c) 159] has shown that this abnormality is present at the level of automatic discrimination of change in speech sounds, as revealed by magnetoencephalographic recording of auditory mismatch field in response to across-category change in vowels. Here, we investigated the neuroanatomical substrate for this physiological abnormality. Thirteen patients with schizophrenia and 19 matched control subjects were examined using magnetoencephalography (MEG) and high-resolution magnetic resonance imaging (MRI) to evaluate both mismatch field strengths in response to change between vowel /a/ and /o/, and gray matter volumes of Heschl's gyrus (HG) and planum temporale (PT). The magnetic global field power of mismatch response to change in phonemes showed a bilateral reduction in patients with schizophrenia. The gray matter volume of left planum temporale, but not right planum temporale or bilateral Heschl's gyrus, was significantly smaller in patients with schizophrenia compared with that in control subjects. Furthermore, the phonetic mismatch strength in the left hemisphere was significantly correlated with left planum temporale gray matter volume in patients with schizophrenia only. These results suggest that structural abnormalities of the planum temporale may underlie the functional abnormalities of fundamental language-related processing in schizophrenia. Funding:
|
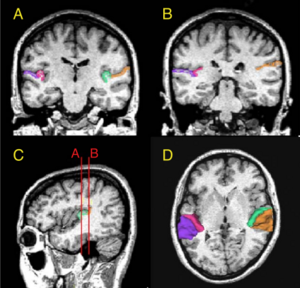 (A and B) Delineation of Heschl’s gyrus and planum temporale in a coronal slice in rostral and caudal part of regions of interest, respectively, based on MRI data of a control subject. The gray matter of Heschl’s gyrus is labeled green on subject left and wine-red on subject right. The gray matter of planum temporale is orange on subject left and violet on subject right. (C) Sagittal view of the Heschl’s gyrus and planum temporale in the left hemisphere. The coronal lines A and B correspond to the planes of panels A and B, respectively. (D) Three-dimensional reconstruction of Heschl’s gyrus and planum temporale gray matter superimposed on the axial plane. Each region is labeled using the same color as that in panels A, B and C. |
2003
Genetic Contribution to Cartilage Volume in Women: A Classical Twin Study
|
Publication: Rheumatology (Oxford). 2003 Dec;42(12):1495-500. PMID: 12832711 | PDF Authors: Hunter DJ, Snieder H, March L, Sambrook PN. Institution: Institute of Bone and Joint Research, Royal North Shore Hospital, University of Sydney, Australia. Background/Purpose: A classical twin study was performed to assess the relative contribution of genetic and environmental factors to cartilage volume. Methods: The subjects were 136 adult female twins: 31 monozygotic and 37 dizygotic twin pairs. The subjects had a T2-weighted fat-saturated sagittal gradient echo MRI performed of their right knee. Femoral, tibial and patella cartilage volumes were measured using 3D Slicer software that facilitates semi-automatic segmentation, generation of three-dimensional surface models and quantitative analysis. The intraclass correlations were calculated, and maximum-likelihood model fitting was used to estimate genetic and environmental variance components. All variables were adjusted for age, BMI and femoral condyle size. The intraclass correlations for all of the cartilage volumes assessed were higher in monozygotic than dizygotic twin pairs. The heritabilities (95% confidence intervals) obtained from model fitting were: femoral, 61% (36-77%); tibial, 76% (56-87%); patella, 66% (47-79%); and total cartilage volume, 73% (51-85%). This study provides evidence for the importance of genetic factors in determining cartilage volume. Identifying heritability is the first step on the way to finding specific genes, which may improve our insight in the pathophysiology of cartilage disorders including the etiology of complex diseases such as osteoarthritis. Funding:
|
Advanced Computer Assistance for Magnetic Resonance-guided Microwave Thermocoagulation of Liver Tumors
|
Publication: Acad Radiol. 2003 Dec;10(12):1442-9. PMID: 14697012 | PDF Authors: Morikawa S, Inubushi T, Kurumi Y, Naka S, Sato K, Demura K, Tani T, Haque HA, Tokuda J, Hata N. Institution: Molecular Neuroscience Research Center, Shiga University of Medical Science, Seta Tsukinowa-cho, Ohtsu, Shiga, Japan. Background/Purpose: The purpose of this study was to utilize computer assistance effectively for both easy and accurate magnetic resonance (MR) image-guided microwave thermocoagulation therapy of liver tumors. An open configuration MR scanner and a microwave coagulator at 2.45 GHz were used. A navigation software, 3D Slicer, was customized to combine fluoroscopic MR images and preoperative MR images for the navigation. New functions to display MR temperature maps with simple parameter setting, and to record and display the coagulated areas by multiple microwave ablations in the 3-dimensional space (footprinting), were also introduced into the software. The VGA signal of the computer display was directly transferred to the surgeon's monitor. The customized software could be used for both accurate image navigation and convenient and easy temperature monitoring. Because repeated punctures and ablations are usually required in this procedure, the footprinting function made targeting of the tumors both easy and accurate and was quite effective in achieving the necessary and sufficient treatment. Furthermore, clear display on the surgeon's monitor, which was obtained by direct transfer of the VGA signal, enabled precise image navigation. The newly developed computer assistance was quite useful and helpful for this MR-guided procedure. |
The Association of Cartilage Volume with Knee Pain
|
Publication: Osteoarthritis Cartilage. 2003 Oct;11(10):725-9. PMID: 13129691 | PDF Authors: Hunter DJ, March L, Sambrook PN. Institution: Institute of Bone and Joint Research, Royal North Shore Hospital, Sydney, Australia. Background/Purpose: Whilst the characteristic pathologic feature of OA is the loss of hyaline cartilage, prior studies have demonstrated a poor relationship between severity of reported knee pain and degree of radiographic change. The aim of this study was to examine the association between knee symptoms and MRI cartilage volume. DESIGN: A cross-sectional study was performed to assess the association between knee symptoms and MRI cartilage volume in an unselected, community based population. The subjects were 133 postmenopausal females. The subjects had a T2-weighted fat saturated sagittal gradient-echo MRI performed of their right knee. Femoral, tibial and patella cartilage volumes were measured using 3D Slicer, a software that facilitates semi-automatic segmentation, generation of 3D surface models and quantitative analysis. Qualitative data relating to symptoms, stiffness, pain, physical dysfunction and the quality of life using the WOMAC were recorded. The statistical analyses conducted to determine measures of association between knee pain/symptoms and cartilage volume were correlation, multiple regression and inter-quartile regression. Assessment of the association between patella cartilage volume and the WOMAC domains showed an inverse relationship between patella cartilage volume and pain, function and global score in a model including body mass index, physical activity and leg extensor power (all P=0.01). Inter-quartile regression comparing the lowest 25% with highest 25% patella cartilage volume demonstrated a stronger inverse relationship (P=0.005). This study suggests that alterations in patella volume are associated with pain, function and global scores of the WOMAC. In participants with more knee pain, there was an association with severity of patella cartilage reduction. Other MRI cartilage volume features were not strongly associated with WOMAC sub-scores. |
Three-dimensional Reconstruction of Magnetic Resonance Images of the Anal Sphincter and Correlation between Sphincter Volume and Pressure
|
Publication: Am J Obstet Gynecol. 2003 Jul;189(1):130-5. PMID: 12861151 | PDF Authors: Cornella JL, Hibner M, Fenner DE, Kriegshauser JS, Hentz J, Magrina JF. Institution: Mayo Graduate School of Medicine, Rochester, MN, USA. Background/Purpose: The purpose of this study was to assess the correlation between internal and external anal sphincter volumes and manometric anal pressures. Ten healthy nulliparous women underwent anal sphincter magnetic resonance imaging and anal manometry measurement. A 3-dimensional reconstruction of magnetic resonance images was accomplished with the use of 3D Slicer. Sphincter volumes were measured 3 times by the same observer for each of 10 patients. The intrarater reliability was measured with the use of the intraclass correlation coefficient (ICC = sigma2(patients)/(sigma 2(patients) + sigma2(error))) from a 2-way analysis of variance model with terms for patient and measurement trial. Measurements that were recorded on anal manometry included squeeze length, length of the high-pressure zone, and maximal resting and squeeze pressures. The mean volumes (± SD) were 18.77 ± 4.64 cm3, 13.82 ± 3.8 cm3, and 32.36 ± 8.37 cm3 for internal, external, and combined sphincters, respectively. Intrarater reliability was 98% for external sphincter volume (95% CI, 94%-99%), 98% for internal sphincter volume (95% CI, 94%-99%), and 99% for total volume (95% CI, 97%-100%). On the 3-dimensional images, the internal sphincter was found to be cylindric in shape, with an ellipse as a base. It is elongated in the anterior and posterior direction and flattened on the sides. The external sphincter was found to be funnel-shaped, being narrower caudad and widening in the cephalad direction. Similar to the internal sphincter, the external sphincter is elongated in the anteroposterior diameter. Volumes of the internal, external, and combined sphincters did not correlate with the maximum pressures at rest and squeeze. Correlations higher than r = 0.5 were observed for all 3 sphincter volume measurements versus high pressure zone at squeeze. The highest correlation, r = 0.66, was for internal sphincter volume versus high pressure zone at squeeze Three-dimensional reconstruction of the rectal sphincter musculature can be performed easily with 3-dimensional software. Measurements of the sphincter volumes have excellent intrarater reliability. Sphincter volumes do not correlate with pressures at rest or squeeze, but the internal sphincter volume correlates with the length of the high pressure zone at squeeze. Contrary to current generalized concepts, it is possible that the internal sphincter may play some role in generating the squeeze pressure. More research is necessary in applying 3-dimensional magnetic resonance image reconstruction in patients with different parity and continence status. Reconstruction of magnetic resonance images of the rectal sphincter musculature may prove to be beneficial in planning the treatment of patients with fecal incontinence. |
|
Publication: Acta Neurochir Suppl. 2003;85:121-5. PMID: 12570147 | PDF Authors: Nabavi A, Gering DT, Kacher DF, Talos IF, Wells WM, Kikinis R, Black PM, Jolesz FA. Institution: Department of Neurosurgery, University Kiel, Kiel, Germany. Background/Purpose: The introduction of MRI into neurosurgery has opened multiple avenues, but also introduced new challenges. The open-configuration intraoperative MRI installed at the Brigham and Women's Hospital in 1996 has been used for more than 500 open craniotomies and beyond 100 biopsies. Furthermore the versatile applicability, employing the same principles, is evident by its frequent use in other areas of the body. However, while intraoperative scanning in the SignaSP yielded unprecedented imaging during neurosurgical procedures their usage for navigation proved bulky and unhandy. To be fully integrated into the procedure, acquisition and display of intraoperative data have to be dynamic and primarily driven by the surgeon performing the procedure. To use the benefits of computer-assisted navigation systems together with immediate availability of intraoperative imaging we developed a software package. 3D Slicer has been used routinely for biopsies and open craniotomies. The system is stable and reliable. Pre- and intraoperative data can be visualized to plan and perform surgery, as well as to accommodate for intraoperative deformations, "brain shift", by providing online data acquisition. Funding:
|
The Virtual Craniofacial Patient: 3D Jaw Modeling and Animation
|
Publication: Stud Health Technol Inform. 2003;94:65-71. PMID: 15455866 | PDF Authors: Enciso R, Memon A, Fidaleo DA, Neumann U, Mah J. Institution: Craniofacial Virtual Reality Laboratory, University of Southern California, CA, USA. Background/Purpose: Recent developments in technology and software are providing better data and methods to facilitate research in biomedical modeling and simulation. In the area of segmentation, original methods involved the time-consuming task of manually tracing structures from slice to slice. This process is now possible with significantly less interaction from the user. Programs such as 3D Slicer, Mimics (Materialise N.V., Heverlee, Belgium) and Amira 2.3 (TGS) provide semi-automatic image-processing-based segmentation and modeling from CT images. These programs use the Generalized Marching Cubes algorithm to create a polygonal wireframe mesh of the segmented area and export a model in STL or other formats. Funding:
|
2002
A 3D Fiber Model of the Human Brainstem
|
Publication: Comput Med Imaging Graph. 2002 Nov-Dec;26(6):439-44. PMID: 12453507 | PDF Authors: Axer H, Leunert M, Mürköster M, Grässel D, Larsen L, Griffin LD, Graf v Keyserlingk D. Institution: Department of Neurology, Friedrich-Schiller-University, Jena, Germany. Background/Purpose: A new neuroanatomic approach to evaluate the fiber orientation in gross histological sections of the human brain was developed. Serial sections of a human brainstem were used to derive fiber orientation maps by analysis of polarized light sequences of these sections. Fiber inclination maps visualize angles of inclination, and fiber direction maps show angles of direction. These angles define vectors which can be visualized as RGB-colors. The serial sections were aligned to each other using the minimized Euclidian distance as fit criterion. In the 3D data set of the human brainstem the major fiber tracts were segmented, and three-dimensional models of these fiber tracts were generated. The presented results demonstrate that two kinds of fiber atlases are feasible: a fiber orientation atlas representing a vector in each voxel, which shows the nerve fiber orientation, and a volume-based atlas representing the major fiber tracts. These models can be used for the evaluation of diffusion tensor data as well as for neurosurgical planning. |
3D Visualization of the Middle Ear and Adjacent Structures Using Reconstructed Multi-slice CT Datasets, Correlating 3D Images and Virtual Endoscopy to the 2D Cross-sectional Images
|
Publication: Neuroradiology. 2002 Sep;44(9):783-90. PMID: 12221454 | PDF Authors: Rodt T, Ratiu P, Becker H, Bartling S, Kacher DF, Anderson M, Jolesz FA, Kikinis R. Institution: Department of Neuroradiology, Hannover Medical School, Hannover, Germany. Background/Purpose: The 3D imaging of the middle ear facilitates better understanding of the patient's anatomy. Cross-sectional slices, however, often allow a more accurate evaluation of anatomical structures, as some detail may be lost through post-processing. In order to demonstrate the advantages of combining both approaches, we performed computed tomography (CT) imaging in two normal and 15 different pathological cases, and the 3D models were correlated to the cross-sectional CT slices. Reconstructed CT datasets were acquired by multi-slice CT. Post-processing was performed using the in-house software 3D Slicer, applying thresholding and manual segmentation. 3D models of the individual anatomical structures were generated and displayed in different colors. The display of relevant anatomical and pathological structures was evaluated in the greyscale 2D slices, 3D images, and the 2D slices showing the segmented 2D anatomy in different colors for each structure. Correlating 2D slices to the 3D models and virtual endoscopy helps to combine the advantages of each method. As generating 3D models can be extremely time-consuming, this approach can be a clinically applicable way of gaining a 3D understanding of the patient's anatomy by using models as a reference. Furthermore, it can help radiologists and otolaryngologists evaluating the 2D slices by adding the correct 3D information that would otherwise have to be mentally integrated. The method can be applied to radiological diagnosis, surgical planning, and especially, to teaching. |
2001
Serial Intraoperative Magnetic Resonance Imaging of Brain Shift
|
Publication: Neurosurgery. 2001 Apr;48(4):787-97. PMID: 11322439 | PDF Authors: Nabavi A, Black PM, Gering DT, Westin C-F, Mehta V, Pergolizzi RS Jr, Ferrant M, Warfield SK, Hata N, Schwartz RB, Wells WM III, Kikinis R, Jolesz FA. Institution: Division of Neurosurgery, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: A major shortcoming of image-guided navigational systems is the use of preoperatively acquired image data, which does not account for intraoperative changes in brain morphology. The occurrence of these surgically induced volumetric deformations ("brain shift") has been well established. Maximal measurements for surface and midline shifts have been reported. There has been no detailed analysis, however, of the changes that occur during surgery. The use of intraoperative magnetic resonance imaging provides a unique opportunity to obtain serial image data and characterize the time course of brain deformations during surgery. The vertically open intraoperative magnetic resonance imaging system (SignaSP, 0.5 T; GE Medical Systems, Milwaukee, WI) permits access to the surgical field and allows multiple intraoperative image updates without the need to move the patient. We developed volumetric display software, the 3D Slicer, that allows quantitative analysis of the degree and direction of brain shift. For 25 patients, four or more intraoperative volumetric image acquisitions were extensively evaluated. Serial acquisitions allow comprehensive sequential descriptions of the direction and magnitude of intraoperative deformations. Brain shift occurs at various surgical stages and in different regions. Surface shift occurs throughout surgery and is mainly attributable to gravity. Subsurface shift occurs during resection and involves collapse of the resection cavity and intraparenchymal changes that are difficult to model. Brain shift is a continuous dynamic process that evolves differently in distinct brain regions. Therefore, only serial imaging or continuous data acquisition can provide consistently accurate image guidance. Furthermore, only serial intraoperative magnetic resonance imaging provides an accurate basis for the computational analysis of brain deformations, which might lead to an understanding and eventual simulation of brain shift for intraoperative guidance. Funding:
|
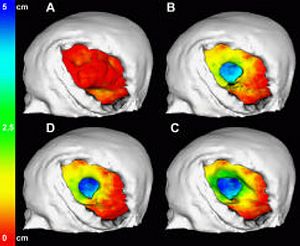 Color-coded models for the evaluation of successive surface deformations. The brain surfaces were extracted from the 3D volume SPGRs for all time points. The surface displacement from stage to stage was automatically calculated and color-coded. The color encodes depths from red (0 mm) to green (2.5 cm) to blue (5 cm). The color-coding was projected onto the model of the brain at that respective stage of the surgery. |
2000
Image-guided Therapy and Intraoperative MRI in Neurosurgery
|
Publication: Minim Invasive Ther Allied Technol. 2000;9(3-4):277-86. PMID: 20156025 Authors: Nabavi A, Mamisch CT, Gering DT, Kacher DF, Pergolizzi RS, Wells WM 3rd, Kikinis R, Black PM, Jolesz FA. Institution: Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Computer-assisted 3D planning, navigation and the possibilities offered by intra-operative imaging updates have made a large impact on neurological surgery. Three-dimensional rendering of complex medical image information, as well as co-registration of multimodal sources has reached a highly sophisticated level. When introduced into surgical navigation however, this pre-operative data is unable to account for intra-operative changes, ('brain-shift'). To update structural information during surgery, an open-configured, intra-operative MRI (Signa SP, 0.5 T) was realized at our institution in 1995. The design, advantages, limitations and current applications of this system are discussed, with emphasis on the integration of imaging into procedures. We also introduce our integrated platform for intra-operative visualization and navigation, the 3D Slicer. Funding:
|
Go to 2020 :: 2019 :: 2018 :: 2017 :: 2016 :: 2015 :: 2014-2011:: 2010-2005