Main Page/SlicerCommunity-2000-2005
Contents
- 1 2005
- 1.1 Magnetic Resonance Imaging and 3-Dimensional Analysis of External Anal Sphincter Anatomy
- 1.2 Group-Slicer: A Collaborative Extension of 3D Slicer
- 1.3 2D Rigid Registration of MR Scans using the 1D Binary Projections
- 1.4 Preoperative Hepatic 3D Models: Virtual Liver Resection using Three-dimensional Imaging Technique
- 1.5 Three-dimensional Reconstruction and Volumetry of Intracranial Haemorrhage and its Mass Effect
- 1.6 Vaginal Thickness, Cross-Sectional Area, and Perimeter in Women with and Those without Prolapse
- 1.7 Registration and Fusion of CT and MRI of the Temporal Bone
- 1.8 Open-configuration MR-guided Microwave Thermocoagulation Therapy for Metastatic Liver Tumors from Breast Cancer]
- 1.9 Quantification of Airway Diameters and 3D Airway Tree Rendering from Dynamic Hyperpolarized 3He Magnetic Resonance Imaging
- 1.10 A Finite Element Method Model to Simulate Laser Interstitial Thermo Therapy in Anatomical Inhomogeneous Regions
- 1.11 The Application of DTI to Investigate White Matter Abnormalities in Schizophrenia
- 2 2004
- 2.1 A Statistically Based Flow for Image Segmentation
- 2.2 Decreases in Ventricular Volume Correlate with Decreases in Ventricular Pressure in Idiopathic Normal Pressure Hydrocephalus Patients Who Experienced Clinical Improvement after Implantation with Adjustable Valve Shunts
- 2.3 Spatial Motion Constraints in Medical Robot using Virtual Fixtures Generated by Anatomy
- 2.4 Clinical Validation of the Normalized Mutual Information Method for Registration of CT and MR Images in Radiotherapy of Brain Tumors
- 2.5 Diffusion-tensor Imaging–guided Tracking of Fibers of the Pyramidal Tract Combined with Intraoperative Cortical Stimulation Mapping in Patients with Gliomas
- 2.6 Abnormal Association Between Reduced Magnetic Mismatch Field to Speech Sounds and Smaller Left Planum Temporale Volume in Schizophrenia
- 3 2003
- 3.1 Genetic Contribution to Cartilage Volume in Women: A Classical Twin Study
- 3.2 Advanced Computer Assistance for Magnetic Resonance-guided Microwave Thermocoagulation of Liver Tumors
- 3.3 The Association of Cartilage Volume with Knee Pain
- 3.4 Three-dimensional Reconstruction of Magnetic Resonance Images of the Anal Sphincter and Correlation between Sphincter Volume and Pressure
- 3.5 Surgical Navigation in the Open MRI
- 3.6 The Virtual Craniofacial Patient: 3D Jaw Modeling and Animation
- 4 2002
- 5 2001
- 6 2000
2005
Magnetic Resonance Imaging and 3-Dimensional Analysis of External Anal Sphincter Anatomy
|
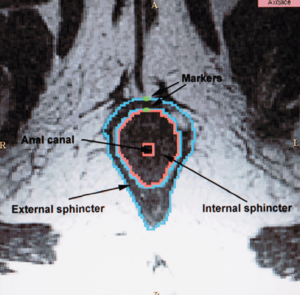
Publication: Obstet Gynecol. 2005 Dec;106(6):1259-65. PMID: 16319250 | PDF Authors: Hsu Y, Fenner DE, Weadock WJ, DeLancey JO. Institution: Pelvic Floor Research Group, Division of Gynecology, Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor, MI, USA. Background/Purpose: To use magnetic resonance images of living women and 3-dimensional modeling software to identify the component parts and characteristic features of the external anal sphincter (EAS) that have visible separation or varying origins and insertions. Methods: Detailed structural analysis of anal sphincter anatomy was performed on 3 pelvic magnetic resonance imaging (MRI) data sets selected for image clarity from ongoing studies involving nulliparous women. The relationships of anal sphincter structures seen in axial, sagittal, and coronal planes were examined using the 3D Slicer 2.1b1 software package. The following were requirements for sphincter elements to be considered separate: 1) a clear and consistently visible separation or 2) a different origin or insertion. The characteristic features identified in this way were then evaluated in images from an additional 50 nulliparas for the frequency of feature visibility. There were 3 components of the EAS that met criteria as being "separate" structures. The main body (EAS-M) is separated from the subcutaneous external anal sphincter (SQ-EAS) by a clear division that could be observed in all (100%) of the MRI scans reviewed. The wing-shaped end (EAS-W) has fibers that do not cross the midline ventrally, but have lateral origins near the ischiopubic ramus. This EAS-W component was visible in 76% of the nulliparas reviewed. Three distinct external anal sphincter components can be identified by MRI in the majority of nulliparous women. Funding:
|
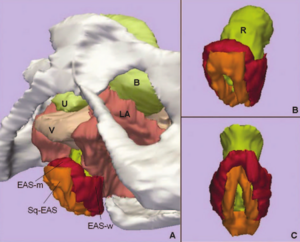 A. Inferior, left three-quarter view of model showing relationship of external anal sphincter complex to the bones and pelvic organs. B. Inferior, left three-quarter view of the external anal sphincter complex. External anal sphincter is in red; note the lateral wing portion of the external anal sphincter. Subcutaneous external anal sphincter is in orange. C. Posterior view of the external anal sphincter complex showing the circumferential nature of both the external anal sphincter and the subcutaneous external anal sphincter. U, urethra; B, bladder; V, vagina; LA, levator ani muscle; R, Rectum; EAS-M, main body of external anal sphincter; EAS-W, lateral wing portion of the external anal sphincter; SQ-EAS, subcutaneous external anal sphincter. |
Group-Slicer: A Collaborative Extension of 3D Slicer
|
Publication: J Biomed Inform. 2005 Dec;38(6):431-42. PMID: 16337568 | PDF Authors: Simmross-Wattenberg F, Carranza-Herrezuelo N, Palacios-Camarero C, Casaseca-de-la-Higuera P, Martín-Fernández MA, Aja-Fernández S, Ruiz-Alzola J, Westin C-F, Alberola-López C. Institution: Laboratorio de Procesado de Imagen, ETSI Telecomunicacion, Universidad de Valladolid, Valladolid, Spain. Background/Purpose: In this paper, we describe a first step towards a collaborative extension of the well-known 3D Slicer; this platform is nowadays used as a standalone tool for both surgical planning and medical intervention. We show how this tool can be easily modified to make it collaborative so that it may constitute an integrated environment for expertise exchange as well as a useful tool for academic purposes. Funding:
|
2D Rigid Registration of MR Scans using the 1D Binary Projections
|
Publication: Enformatika Transactions on Engineering, Computing and Technology, November 2005; 9:157-61. | PDF Author: Panos D. Kotsas Institution: Department of Automated Control and System Engineering, University of Sheffield, UK. Background/Purpose: This research deals with the application of a signal intensity independent registration criterion for 2D rigid body registration of medical images using 1D binary projections. The criterion is defined as the weighted ratio of two projections. The ratio is computed on a pixel per pixel basis and weighting is performed by setting the ratios between one and zero pixels to a standard high value. The mean squared value of the weighted ratio is computed over the union of the one areas of the two projections and it is minimized using the Chebyshev polynomial approximation using n=5 points. The sum of x and y parallel projections is used for translational adjustment and a range of parallel projections between 40-50 deg (depending on the orientation of the image) for rotational adjustment. MR-MR registration experiments were performed and gave mean errors well below 1deg and 1 pixel (0.12 deg and 0.47 pixels for the example given in Enformatika Publication). The method is to be extended for surface matching. |
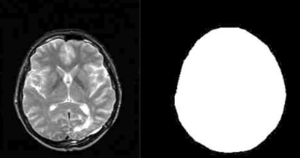 T2 MR scan (contrast enhanced) and mask created with 3D Slicer software |
Preoperative Hepatic 3D Models: Virtual Liver Resection using Three-dimensional Imaging Technique
|
Publication: Eur J Radiol. 2005 Nov;56(2):179-84. PMID: 15890482 Authors: Numminen K, Sipilä O, Mäkisalo H. Institution: Helsinki Medical Imaging Center, Department of Radiology, Helsinki University Central Hospital, Helsinki, Finland. Background/Purpose: Emerging new techniques for liver resections set new requirements for the preoperative imaging and planning. Open surgery is a three-dimensional procedure and planning of the resection line may be difficult when basing on conventional two-dimensional CTs or MRIs, although all the information is there. With multidetector-row CT (MDCT), thin slices can be obtained with excellent temporal resolution, and precise three-dimensional (3D) models can be created. We regard 3D imaging technique useful in most liver resections. It improves the surgeon's knowledge of liver anatomy and makes even more complicated liver resections safe. Better knowledge of three-dimensional appearances of liver structures may further improve the results of curative liver surgery. However, before becoming a routine clinical procedure, research and development are still needed. Also, careful testing and evaluation of the methods have to be performed. In the future, 3D models will probably play an important role in the preoperative planning of liver resections. |
 A 76-year-old man with hepatocellular carcinoma. MDCT image shows large tumor in liver segments 5-8 (a). Semi-automatic segmentation based on thresholding, morphological operations and connected component labelling is utilized to create a triangulated surface model. Segmented structures can be visualized with different colors and opacities. 3D model from portal veins (b), from hepatic veins (c), liver tumor (d) and liver parenchyma (e). The model can be studied freely from any direction on the computer screen (f). Resection line is configured immediately right to the middle hepatic vein (g). Vessels crossing the resection line can be visualized and easily found when performing right-sided lobectomy (h). |
Three-dimensional Reconstruction and Volumetry of Intracranial Haemorrhage and its Mass Effect
|
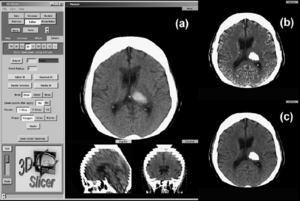
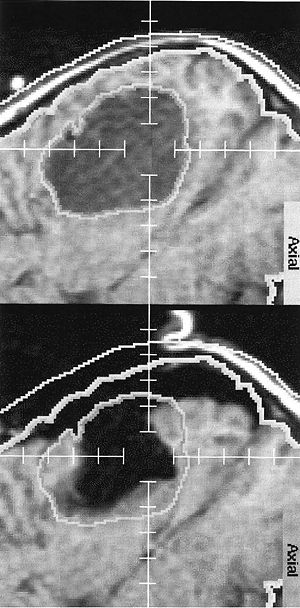
Publication: Neuroradiology. 2005 Jun;47(6):417-24. PMID: 15856213 | PDF Authors: Strik HM, Borchert H, Fels C, Knauth M, Rienhoff O, Bähr M, Verhey JF. Institution: Department of Neurology, Medical School, University of Göttingen, Germany. Background/Purpose: Intracerebral haemorrhage still causes considerable disability and mortality. The studies on conservative and operative management are inconclusive, probably due to inexact volumetry of the haemorrhage. We investigated whether three-dimensional (3D), voxel-based volumetry of the haemorrhage and its mass effect is feasible with routine computed tomography (CT) scans. The volumes of the haemorrhage, ventricles, midline shift, the intracranial volume and ventricular compression in CT scans of 12 patients with basal ganglia haemorrhage were determined with the 3D Slicer software. Indices of haemorrhage and intracranial or ventricular volume were calculated and correlated with the clinical data. The intended measures could be determined with an acceptable intra-individual variability. The 3D volumetric data tended to correlate better with the clinical course than the conventionally assessed distance of midline shift and volume of haemorrhage. 3D volumetry of intracranial haemorrhage and its mass effect is feasible with routine CT examination. Prospective studies should assess its value for clinical studies on intracranial space-occupying diseases. |
Vaginal Thickness, Cross-Sectional Area, and Perimeter in Women with and Those without Prolapse
|
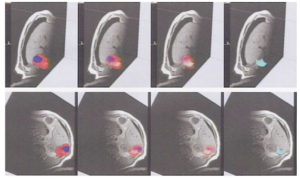
Publication: Obstet Gynecol. 2005 May;105(5 Pt1):1012-7. PMID: 15863538 | PDF Authors: Hsu Y, Chen L, Delancey JO, Ashton-Miller JA. Institution: Division of Gynecology, Department of Obstetrics and Gynecology, University of Michigan Medical School, Ann Arbor, MI, USA. Background/Purpose: Use axial magnetic resonance imaging to test the null hypothesis that no difference exists in apparent vaginal thickness between women with and those without prolapse. Magnetic resonance imaging studies of 24 patients with prolapse at least 2 cm beyond the introitus were selected from an ongoing study comparing women with prolapse with normal control subjects. The magnetic resonance scans of 24 women with prolapse (cases) and 24 women without prolapse (controls) were selected from those of women of similar age, race, and parity. The magnetic resonance files were imported into an experimental modeling program, and 3-dimensional models of each vagina were created. The minimum transverse plane cross-sectional area, mid-sagittal plane diameter, and transverse plane perimeter of each vaginal model were calculated. Neither the mean age (cases 58.6 years ± standard deviation [SD] 14.4 versus controls 59.4 years ± SD 13.2) nor the mean body mass index (cases 24.1 kg/m2± SD 3.3, controls 25.7 kg/m2± SD 3.7) differed significantly between groups. Minimum mid-sagittal vaginal diameters did not differ between groups. Patients with prolapse had larger minimum vaginal cross-sectional areas than controls (5.71 cm2± standard error of the mean [SEM] 0.25 versus 4.76 cm2± SEM 0.20, respectively; P = .005). The perimeter of the vagina was also larger in the prolapse group (11.10 cm ± SEM 0.24) compared with controls (9.96 cm ± SEM 0.22) P = .001. Subgroup analysis of patients with endogenous or exogenous estrogen showed prolapse patients had larger vaginal cross-sectional area (P = .030); in patients without estrogen group differences were not significant (P = .099). Vaginal thickness is similar in women with and those without pelvic organ prolapse. The vaginal perimeter and cross-sectional areas are 11% and 20% larger in prolapse patients, respectively. Estrogen status did not affect differences found between groups. Funding:
|
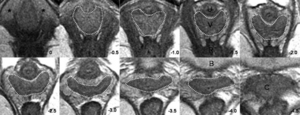 Axial slices at 5-mm intervals arranged caudal to cephalad starting from the image in the upper left (image 0). Vaginal tracings were made from above the level of the vestibular bulbs (VB), represented by asterisks (*), caudally (image 0) to below where the cervix (C) could be seen (image -4.0). U, urethra; V, vagina; R, rectum; B, bladder. |
Registration and Fusion of CT and MRI of the Temporal Bone
|
Publication: J Comput Assist Tomogr. 2005 May-Jun;29(3):305-10. PMID: 15891495 | PDF Authors: Bartling S, Peldschus K, Rodt T, Kral F, Matthies H, Kikinis R, Becker H. Institution: Department of Neuroradiology, Hannover Medical School, Hannover, Germany. Background/Purpose: CT and MRI of the skull base and the Temporal provides complimentary information. A registration and fusion of CT and MRI may improve diagnosis, because features only seen in one modality can be assessed with respect to the information gathered from the other modality. A manual, rigid registration method - basically overlaying two volumes in one space - as implemented in 3D Slicer was used. Threshold based fusion methods resulted in MRI overlaying co-registered CT. Landmarks have been used to assess target registration error - registration accuracy was within the range of the voxel size of either modality. A range of different pathological conditions was used to demonstrate the potential benefits of this methods. |
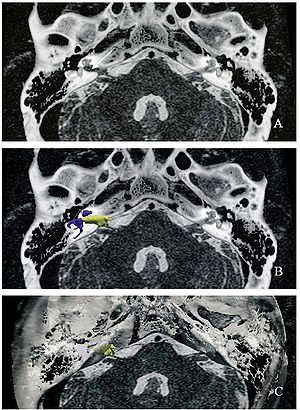 Acoustic schwannoma in the right internal auditory canal (arrow) in registered and fused CT and MRI of the temporal bone. For surgical planning, the MRI-given tumor (yellow) and critical CT-given surgical landmarks such as the labyrinth (blue) and the facial nerve canal (gray) as well as the bony skull base (white) can be displayed together. |
Open-configuration MR-guided Microwave Thermocoagulation Therapy for Metastatic Liver Tumors from Breast Cancer]
|
Publication: Breast Cancer. 2005;12(1):26-31. PMID: 15657520 | PDF Authors: Abe H, Kurumi Y, Naka S, Shiomi H, Umeda T, Naitoh H, Endo Y, Hanasawa K, Morikawa S, Tani T. Institution: Division of General Surgery, Department of Surgery, Shiga University of Medical Science, Seta-Tsukinowa, Otsu, Shiga, Japan. Background/Purpose: Liver metastases from breast cancer are associated with a poor prognosis, however, local control with microwave thermocoagulation therapy has been used in certain subgroups of these patients in the past decade. In this study, open-configuration magnetic resonance (MR) -guided microwave thermocoagulation therapy was used for metastatic liver tumors from breast cancer, and the efficacy of this treatment was assessed. Methods: Between June 2000 and April 2004, we used MR-guided microwave thermocoagulation therapy on 11 nodules in 8 patients with metastatic liver tumors from breast cancer. The procedure was carried out under general anesthesia. A 0.5 T open-configuration MR system and a microwave coagulator were used. Near-real-time MR images and real-time temperature images were collected and displayed on the monitor. The MR-compatible thoracoscope was used and combined with MR imaging guidance. Navigation software, a 3D Slicer, was installed and customized. The customized navigation software displayed near-real-time MR images. The percutaneous puncture into the tumors was successful in all cases. No mortality or major complications occurred as a result of the procedures. Five of the 8 patients are alive with new metastatic foci with a mean observation period of 25.9 months. We developed several devices to allow safe, easy, and accurate MR-guided microwave thermocoagulation therapy of liver tumors. Open-configuration MR-guided microwave thermocoagulation therapy appears to be a feasible method for tumor ablation of metastatic liver tumors from breast cancer. |
Quantification of Airway Diameters and 3D Airway Tree Rendering from Dynamic Hyperpolarized 3He Magnetic Resonance Imaging
|
Publication: Magn Reson Med. 2005 Feb;53(2):474-8. PMID: 15678546 | PDF Authors: Lewis TA, Tzeng YS, McKinstry EL, Tooker AC, Hong K, Sun Y, Mansour J, Handler Z, Albert MS. Institution: Brigham and Womem's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: As another step toward extracting quantitative information from hyperpolarized 3He MRI, airway diameters in humans were measured from projection images and multislice images of the lungs. Values obtained were in good agreement with the Weibel lung morphometry model. The measurement of airway caliber can now be achieved without the use of ionizing radiation. Furthermore, it was demonstrated that 3D airway tree renderings could be constructed from the multislice data. Both the measurement of airway diameters and the rendering of 3D airway information hold promise for the clinical assessment of bronchoconstrictive diseases such as asthma and the associated evaluation of treatment effectiveness. Work is being done to address the uncertainties of the manually intensive methods we have developed. Funding:
|
 Airway tree constructed from stacking dynamic multislice data sets in 3D Slicer. |
A Finite Element Method Model to Simulate Laser Interstitial Thermo Therapy in Anatomical Inhomogeneous Regions
|
Publication: Biomed Eng Online. 2005 Jan 4;4(1):2. PMID: 15631630 | PDF Authors: Mohammed Y, Verhey JF. Institution: Department of Medical Informatics, University of Goettingen, Goettingen, Germany. Background/Purpose: Laser Interstitial ThermoTherapy (LITT) is a well established surgical method. The use of LITT is so far limited to homogeneous tissues, e.g. the liver. One of the reasons is the limited capability of existing treatment planning models to calculate accurately the damage zone. The treatment planning in inhomogeneous tissues, especially of regions near main vessels, poses still a challenge. In order to extend the application of LITT to a wider range of anatomical regions new simulation methods are needed. The model described with this article enables efficient simulation for predicting damaged tissue as a basis for a future laser-surgical planning system. Previously we described the dependency of the model on geometry. With the presented paper including two video files we focus on the methodological, physical and mathematical background of the model. |
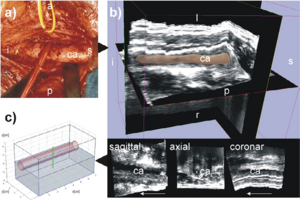 The geometry used. The left carotid artery is shown in this figure labelled with ca. The following letters indicate the orientation: s for superior, i for inferior, p for posterior, a for anterior, l for left, r for right. (a) is a photo of the human anatomy in the neck area. The carotid artery is shown here after moving the vein to the cranial direction. (b) shows the corresponding freehand 3D ultrasound dataset of the human neck region acquired axially. The 3D image in the top of (b) shows the 3D ultrasound volume together with the carotid artery segmented with 3D Slicer software [17]. The 3D model is displayed with 40% transparency. (c) displays the model used in the simulation approximated according to the geometry of the human neck shown in (a) and (b). The segmentation of the 3D ultrasound dataset in (b), is available as a video stream, too, showing the geometry of the carotid artery. |
The Application of DTI to Investigate White Matter Abnormalities in Schizophrenia
|
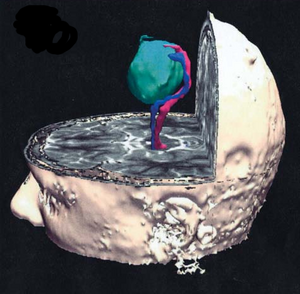
Publication: Ann. N.Y. Acad. Sci. 2005; 1064:134-48. PMID: 16394153 | PDF Authors: Kubicki M, Westin C-F, McCarley RW, Shenton ME. Institution: Clinical Neuroscience Division, Laboratory of Neuroscience, Boston VA Healthcare System–Brockton Division, Department of Psychiatry, Harvard Medical School, Brockton, MA, USA. Background/Purpose: Schizophrenia is a serious and disabling mental disorder that affects approximately 1% of the general population, with often devastating effects on the psychological and financial resources of the patient, family, and larger community. The etiology of schizophrenia is not known, although it likely involves several interacting biological and environmental factors that predispose an individual to schizophrenia. However, although the underlying pathology remains unknown, it has been believed that brain abnormalities would ultimately be linked to the etiology of schizophrenia. This theory was rekindled in the 1970s, when the first computer-assisted tomography (CT) study showed enlarged lateral ventricles in schizophrenia. Since that time, there have been many improvements in MR acquisition and image processing, including the introduction of positron emission tomography (PET), followed by functional MR (fMRI), and diffusion tensor imaging (DTI). These advances have led to an appreciation of the critical role that brain abnormalities play in schizophrenia. While structural MRI has proven to be useful in investigating and detecting gray matter abnormalities in schizophrenia, the investigation of white matter has proven to be more challenging as white matter appears homogeneous on conventional MRI and the fibers connecting different brain regions cannot be appreciated. With the development of DTI, we are now able to investigate white matter abnormalities in schizophrenia. Funding:
|
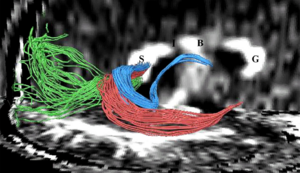 Fibers traveling through the splenium of the corpus callosum are shown, where fibers connecting the left and right occipital lobe are displayed in green, fibers interconnecting lateral temporal regions are displayed in red, and fibers connecting medial temporal regions are displayed in blue. Additionally, the genu of the corpus callosum is labeled as “G”, the body as “B”, the isthmus as “I”, and the splenium as “S”. |
2004
A Statistically Based Flow for Image Segmentation
|
Publication: Med Image Anal. 2004 Sep;8(3):267-74. PMID: 15450221 | PDF Authors: Pichon E, Tannenbaum A, Kikinis R. Institution: School of Electrical & Computer Engineering, Georgia Institute of Technology, Atlanta, GA, USA. Background/Purpose: In this paper we present a new algorithm for 3D medical image segmentation. The algorithm is versatile, fast, relatively simple to implement, and semi-automatic. It is based on minimizing a global energy defined from a learned non-parametric estimation of the statistics of the region to be segmented. Implementation details are discussed, and source code is freely available as part of the 3D Slicer project. In addition, a new unified set of validation metrics is proposed. Results on artificial and real MRI images show that the algorithm performs well on large brain structures both in terms of accuracy and robustness to noise. Funding:
|
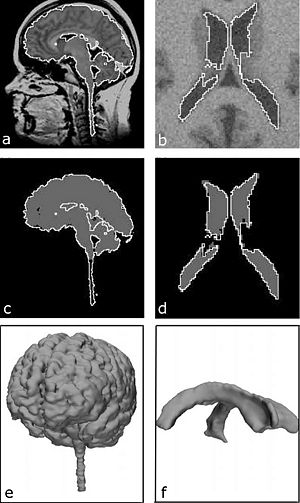 Results on real and noisy simulated datasets (left and right respectively): (a) sagittal slice of real dataset and proposed segmentation (WM GM); (b) axial slice of artificial dataset and proposed segmentation (ventricle); (c) expert segmentation (gray) and proposed segmentation (white); (d) underlying ground truth (gray) and proposed segmentation (white); (e) rendered surface of proposed segmentation (WM GM); (f) rendered surface of proposed segmentation (ventricle). |
Decreases in Ventricular Volume Correlate with Decreases in Ventricular Pressure in Idiopathic Normal Pressure Hydrocephalus Patients Who Experienced Clinical Improvement after Implantation with Adjustable Valve Shunts
|
Publication: Neurosurgery. 2004 Sep;55(3):582-92. PMID: 15335425 | PDF Authors: McConnell KA, Zou KH, Chabrerie AV, Bailey NO, Black PM. Institution: Department of Neurosurgery, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: This retrospective study examined whether changes in ventricular volume correspond with changes in adjustable valve pressure settings in a cohort of patients who received shunts to treat idiopathic normal pressure hydrocephalus. We also examined whether these pressure-volume curves and other patient variables would co-occur with a positive clinical response to shunting. Methods: We selected 51 patients diagnosed with idiopathic normal pressure hydrocephalus who had undergone implantation of a Codman Hakim programmable valve (Medos S.A., Le Locle, Switzerland). Clinical data were gathered from the patients. Funding:
|
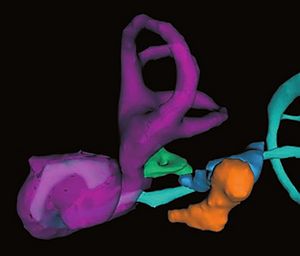
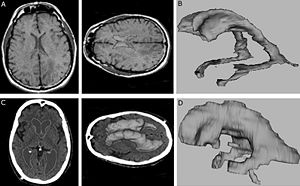 3D Slicer software segmentation of the ventricular system of a subject without hydrocephalus (A) used to produce the three-dimensional model of a normal, nonhydrocephalic ventricular system (B). C and D, 3D Slicer software segmentation of the ventricular system of a subject with INPH (C) used to produce the three-dimensional model of a hydrocephalic ventricular system (D). |
Spatial Motion Constraints in Medical Robot using Virtual Fixtures Generated by Anatomy
|
Publication: Proceedings of the 2004 IEEE International Conference on Robotics & Automation, ICRA 2004. | PDF Authors: Li M, Taylor RH. Institution: Department of Computer Science, NSF Engineering Research Center for Computer Integrated Surgical Systems and Technology, Johns Hopkins University, Baltimore, MD, USA. Background/Purpose: In Ear, Nose and Throat (ENT) surgery, the operating volume is very limited. This is especially true in sinus surgery, when the instrument passes through the nasal and sinus cavity to reach the pathological area. The nasal and sinus bones impose geometric constraints on the work volume. During the surgery, the surgeon needs to control the motion of the instrument tip to accomplish some delicate procedure; meanwhile he/she needs to avoid hitting anatomic constraints. In this paper, we present a method to assist the path following task in a constrained area. The system reads the user’s force input and combines it with the planned tip-trajectory to create the tip motion constraints; meanwhile it generates the tool-shaft boundary constraints based on a 3D geometric model. We map instrument tip motion and boundary information to joint displacements via robot kinematics, and then use a constrained quadratic optimization algorithm to compute the optimal set of corresponding joint displacements. In the preliminary study, we show that robot guidance using cooperative control and virtual fixtures derived from complex geometry can assist users in skilled manipulation tasks, while maintaining desirable properties such as collision avoidance and safety. Funding:
|
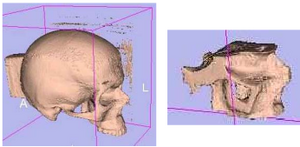 3D Slicer surface models of test phantom. (left) whole skull surface model and, (right) the model of nasal cavity portion used to generate constraints |
Clinical Validation of the Normalized Mutual Information Method for Registration of CT and MR Images in Radiotherapy of Brain Tumors
|
Publication: J Appl Clin Med Phys. 2004 Summer;5(3):66-79. PMID: 15753941 | PDF Authors: Veninga T, Huisman H, van der Maazen RW, Huizenga H. Institution: Department of Radiation Oncology, University Medical Center Nijmegen, The Netherlands. Background/Purpose: Image registration integrates information of different imaging modalities and has the potential to improve target volume determination in radiotherapy planning. This paper describes the implementation and validation of a 3D fully automated registration procedure in the process of radiotherapy treatment planning of brain tumors. 15 Patients with various brain tumors received CT and MR brain imaging before the start of radiotherapy. The normalized mutual information (NMI) method was used for image registration. Registration accuracy was estimated by performing statistical analysis of coordinate differences between CT and MR anatomical landmarks along the x-, y- and z-axes. Second, a visual validation protocol was developed to validate the quality of individual registration solutions and this protocol was tested in a series of 36 CT-MR registration procedures with intentionally applied registration errors. The mean coordinate differences between CT and MR landmarks along the x- and y-axes were in general within 0.5 mm. The mean coordinate differences along the z-axis were within 1.0 mm, which is of the same magnitude as the applied slice thickness in scanning. Second, the detection of intentionally applied registration errors by employment of a standardized visual validation protocol resulted in low false-negative and low false-positive rates. Application of the NMI method for the brain results in excellent automatic registration accuracy and the method has been incorporated in daily routine within our institute. A standardized validation protocol is proposed that ensures the quality of individual registrations by detecting registration errors with high sensitivity and specificity. This protocol is proposed for the validation of other linear registration methods. |
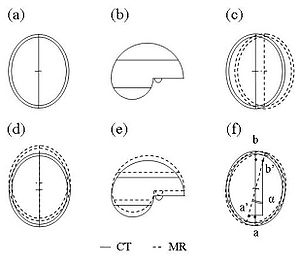 For the purpose of individual quality assurance (QA) of image registration, an independent visual validation protocol was developed, using 3D Slicer, a freely available software program for visualization and processing of medical data. All image data were transferred to 3D Slicer in DICOM format. The validation protocol consists of a stepwise procedure for an estimate of translation errors along the three orthogonal axes (Trx, Try, and Trz) as well as rotation errors around these three axes (Rx, Ry, and Rz). |
Diffusion-tensor Imaging–guided Tracking of Fibers of the Pyramidal Tract Combined with Intraoperative Cortical Stimulation Mapping in Patients with Gliomas
|
Publication: J Neurosurg. 2004 Jul;101(1):66-72. PMID: 15255253 | PDF Authors: Berman JI, Berger MS, Mukherjee P, Henry RG. Institution: Department of Radiology, University of California at San Francisco, CA, USA. Background/Purpose: The goal of this study was to use diffusion-tensor (DT) magnetic resonance (MR) imaging to track fibers combined with cortical stimulation mapping to delineate descending motor pathways. Subcortical localization of motor path-ways in relation to a glioma may provide critical information to guide tumor resection and prevent surgical morbidity. Methods: Eleven adult patients harboring gliomas underwent MR imaging 1 day prior to image-guided intraoperative cortical motor mapping and tumor resection. Screens depicting 27 cortical motor sites on a surgical navigation system were saved to launch DT imaging of fiber tracks of descending motor pathways. The position and organization of motor tracts were visualized by fiber tracking. Tracks from 16 motor stimulation sites followed descending pathways from the precentral gyrus, through the corona radiata and internal capsule, and into the cerebral peduncle. These tracks were also observed on DT images to diverge along crossing white matter bundles (four patients) and to terminate or deviate in regions of peritumoral vasogenic edema (five patients). The use of precise intraoperative cortical mapping information and DT images of fiber tracks can reveal the course of motor pathways beneath the cortex. The subcortical fiber tracks generated are consistent with the known anatomical course and somatotopic organization of the motor tract in relation to its cortical origins. Tracking fibers by using DT imaging in combination with functional localization has the potential to reduce surgical morbidity by revealing subcortical connections of the functional cortex. Funding:
|
Abnormal Association Between Reduced Magnetic Mismatch Field to Speech Sounds and Smaller Left Planum Temporale Volume in Schizophrenia
|
Publication: NeuroImage 2004; 22:720-7. PMID: 15193600 | PDF Authors: Yamasue H, Yamada H, Yumoto M, Kamio S, Kudo N, Uetsuki M, Abe O, Fukuda R, Aoki S, Ohtomo K, Iwanami A, Kato N, Kasai K. Institution: Department of Neuropsychiatry, Graduate School of Medicine, University of Tokyo, Bunkyo, Tokyo, Japan. Background/Purpose: Schizophrenia is associated with language-related dysfunction. A previous study [Schizophr. Res. 59 (2003c) 159] has shown that this abnormality is present at the level of automatic discrimination of change in speech sounds, as revealed by magnetoencephalographic recording of auditory mismatch field in response to across-category change in vowels. Here, we investigated the neuroanatomical substrate for this physiological abnormality. Thirteen patients with schizophrenia and 19 matched control subjects were examined using magnetoencephalography (MEG) and high-resolution magnetic resonance imaging (MRI) to evaluate both mismatch field strengths in response to change between vowel /a/ and /o/, and gray matter volumes of Heschl's gyrus (HG) and planum temporale (PT). The magnetic global field power of mismatch response to change in phonemes showed a bilateral reduction in patients with schizophrenia. The gray matter volume of left planum temporale, but not right planum temporale or bilateral Heschl's gyrus, was significantly smaller in patients with schizophrenia compared with that in control subjects. Furthermore, the phonetic mismatch strength in the left hemisphere was significantly correlated with left planum temporale gray matter volume in patients with schizophrenia only. These results suggest that structural abnormalities of the planum temporale may underlie the functional abnormalities of fundamental language-related processing in schizophrenia. Funding:
|
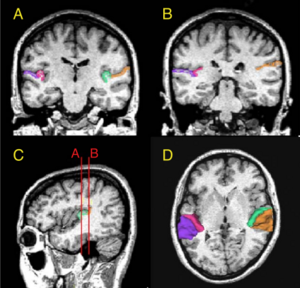 (A and B) Delineation of Heschl’s gyrus and planum temporale in a coronal slice in rostral and caudal part of regions of interest, respectively, based on MRI data of a control subject. The gray matter of Heschl’s gyrus is labeled green on subject left and wine-red on subject right. The gray matter of planum temporale is orange on subject left and violet on subject right. (C) Sagittal view of the Heschl’s gyrus and planum temporale in the left hemisphere. The coronal lines A and B correspond to the planes of panels A and B, respectively. (D) Three-dimensional reconstruction of Heschl’s gyrus and planum temporale gray matter superimposed on the axial plane. Each region is labeled using the same color as that in panels A, B and C. |
2003
Genetic Contribution to Cartilage Volume in Women: A Classical Twin Study
|
Publication: Rheumatology (Oxford). 2003 Dec;42(12):1495-500. PMID: 12832711 | PDF Authors: Hunter DJ, Snieder H, March L, Sambrook PN. Institution: Institute of Bone and Joint Research, Royal North Shore Hospital, University of Sydney, Australia. Background/Purpose: A classical twin study was performed to assess the relative contribution of genetic and environmental factors to cartilage volume. Methods: The subjects were 136 adult female twins: 31 monozygotic and 37 dizygotic twin pairs. The subjects had a T2-weighted fat-saturated sagittal gradient echo MRI performed of their right knee. Femoral, tibial and patella cartilage volumes were measured using 3D Slicer software that facilitates semi-automatic segmentation, generation of three-dimensional surface models and quantitative analysis. The intraclass correlations were calculated, and maximum-likelihood model fitting was used to estimate genetic and environmental variance components. All variables were adjusted for age, BMI and femoral condyle size. The intraclass correlations for all of the cartilage volumes assessed were higher in monozygotic than dizygotic twin pairs. The heritabilities (95% confidence intervals) obtained from model fitting were: femoral, 61% (36-77%); tibial, 76% (56-87%); patella, 66% (47-79%); and total cartilage volume, 73% (51-85%). This study provides evidence for the importance of genetic factors in determining cartilage volume. Identifying heritability is the first step on the way to finding specific genes, which may improve our insight in the pathophysiology of cartilage disorders including the etiology of complex diseases such as osteoarthritis. Funding:
|
Advanced Computer Assistance for Magnetic Resonance-guided Microwave Thermocoagulation of Liver Tumors
|
Publication: Acad Radiol. 2003 Dec;10(12):1442-9. PMID: 14697012 | PDF Authors: Morikawa S, Inubushi T, Kurumi Y, Naka S, Sato K, Demura K, Tani T, Haque HA, Tokuda J, Hata N. Institution: Molecular Neuroscience Research Center, Shiga University of Medical Science, Seta Tsukinowa-cho, Ohtsu, Shiga, Japan. Background/Purpose: The purpose of this study was to utilize computer assistance effectively for both easy and accurate magnetic resonance (MR) image-guided microwave thermocoagulation therapy of liver tumors. An open configuration MR scanner and a microwave coagulator at 2.45 GHz were used. A navigation software, 3D Slicer, was customized to combine fluoroscopic MR images and preoperative MR images for the navigation. New functions to display MR temperature maps with simple parameter setting, and to record and display the coagulated areas by multiple microwave ablations in the 3-dimensional space (footprinting), were also introduced into the software. The VGA signal of the computer display was directly transferred to the surgeon's monitor. The customized software could be used for both accurate image navigation and convenient and easy temperature monitoring. Because repeated punctures and ablations are usually required in this procedure, the footprinting function made targeting of the tumors both easy and accurate and was quite effective in achieving the necessary and sufficient treatment. Furthermore, clear display on the surgeon's monitor, which was obtained by direct transfer of the VGA signal, enabled precise image navigation. The newly developed computer assistance was quite useful and helpful for this MR-guided procedure. |
The Association of Cartilage Volume with Knee Pain
|
Publication: Osteoarthritis Cartilage. 2003 Oct;11(10):725-9. PMID: 13129691 | PDF Authors: Hunter DJ, March L, Sambrook PN. Institution: Institute of Bone and Joint Research, Royal North Shore Hospital, Sydney, Australia. Background/Purpose: Whilst the characteristic pathologic feature of OA is the loss of hyaline cartilage, prior studies have demonstrated a poor relationship between severity of reported knee pain and degree of radiographic change. The aim of this study was to examine the association between knee symptoms and MRI cartilage volume. DESIGN: A cross-sectional study was performed to assess the association between knee symptoms and MRI cartilage volume in an unselected, community based population. The subjects were 133 postmenopausal females. The subjects had a T2-weighted fat saturated sagittal gradient-echo MRI performed of their right knee. Femoral, tibial and patella cartilage volumes were measured using 3D Slicer, a software that facilitates semi-automatic segmentation, generation of 3D surface models and quantitative analysis. Qualitative data relating to symptoms, stiffness, pain, physical dysfunction and the quality of life using the WOMAC were recorded. The statistical analyses conducted to determine measures of association between knee pain/symptoms and cartilage volume were correlation, multiple regression and inter-quartile regression. Assessment of the association between patella cartilage volume and the WOMAC domains showed an inverse relationship between patella cartilage volume and pain, function and global score in a model including body mass index, physical activity and leg extensor power (all P=0.01). Inter-quartile regression comparing the lowest 25% with highest 25% patella cartilage volume demonstrated a stronger inverse relationship (P=0.005). This study suggests that alterations in patella volume are associated with pain, function and global scores of the WOMAC. In participants with more knee pain, there was an association with severity of patella cartilage reduction. Other MRI cartilage volume features were not strongly associated with WOMAC sub-scores. |
Three-dimensional Reconstruction of Magnetic Resonance Images of the Anal Sphincter and Correlation between Sphincter Volume and Pressure
|
Publication: Am J Obstet Gynecol. 2003 Jul;189(1):130-5. PMID: 12861151 | PDF Authors: Cornella JL, Hibner M, Fenner DE, Kriegshauser JS, Hentz J, Magrina JF. Institution: Mayo Graduate School of Medicine, Rochester, MN, USA. Background/Purpose: The purpose of this study was to assess the correlation between internal and external anal sphincter volumes and manometric anal pressures. Ten healthy nulliparous women underwent anal sphincter magnetic resonance imaging and anal manometry measurement. A 3-dimensional reconstruction of magnetic resonance images was accomplished with the use of 3D Slicer. Sphincter volumes were measured 3 times by the same observer for each of 10 patients. The intrarater reliability was measured with the use of the intraclass correlation coefficient (ICC = sigma2(patients)/(sigma 2(patients) + sigma2(error))) from a 2-way analysis of variance model with terms for patient and measurement trial. Measurements that were recorded on anal manometry included squeeze length, length of the high-pressure zone, and maximal resting and squeeze pressures. The mean volumes (± SD) were 18.77 ± 4.64 cm3, 13.82 ± 3.8 cm3, and 32.36 ± 8.37 cm3 for internal, external, and combined sphincters, respectively. Intrarater reliability was 98% for external sphincter volume (95% CI, 94%-99%), 98% for internal sphincter volume (95% CI, 94%-99%), and 99% for total volume (95% CI, 97%-100%). On the 3-dimensional images, the internal sphincter was found to be cylindric in shape, with an ellipse as a base. It is elongated in the anterior and posterior direction and flattened on the sides. The external sphincter was found to be funnel-shaped, being narrower caudad and widening in the cephalad direction. Similar to the internal sphincter, the external sphincter is elongated in the anteroposterior diameter. Volumes of the internal, external, and combined sphincters did not correlate with the maximum pressures at rest and squeeze. Correlations higher than r = 0.5 were observed for all 3 sphincter volume measurements versus high pressure zone at squeeze. The highest correlation, r = 0.66, was for internal sphincter volume versus high pressure zone at squeeze Three-dimensional reconstruction of the rectal sphincter musculature can be performed easily with 3-dimensional software. Measurements of the sphincter volumes have excellent intrarater reliability. Sphincter volumes do not correlate with pressures at rest or squeeze, but the internal sphincter volume correlates with the length of the high pressure zone at squeeze. Contrary to current generalized concepts, it is possible that the internal sphincter may play some role in generating the squeeze pressure. More research is necessary in applying 3-dimensional magnetic resonance image reconstruction in patients with different parity and continence status. Reconstruction of magnetic resonance images of the rectal sphincter musculature may prove to be beneficial in planning the treatment of patients with fecal incontinence. |
|
Publication: Acta Neurochir Suppl. 2003;85:121-5. PMID: 12570147 | PDF Authors: Nabavi A, Gering DT, Kacher DF, Talos IF, Wells WM, Kikinis R, Black PM, Jolesz FA. Institution: Department of Neurosurgery, University Kiel, Kiel, Germany. Background/Purpose: The introduction of MRI into neurosurgery has opened multiple avenues, but also introduced new challenges. The open-configuration intraoperative MRI installed at the Brigham and Women's Hospital in 1996 has been used for more than 500 open craniotomies and beyond 100 biopsies. Furthermore the versatile applicability, employing the same principles, is evident by its frequent use in other areas of the body. However, while intraoperative scanning in the SignaSP yielded unprecedented imaging during neurosurgical procedures their usage for navigation proved bulky and unhandy. To be fully integrated into the procedure, acquisition and display of intraoperative data have to be dynamic and primarily driven by the surgeon performing the procedure. To use the benefits of computer-assisted navigation systems together with immediate availability of intraoperative imaging we developed a software package. 3D Slicer has been used routinely for biopsies and open craniotomies. The system is stable and reliable. Pre- and intraoperative data can be visualized to plan and perform surgery, as well as to accommodate for intraoperative deformations, "brain shift", by providing online data acquisition. Funding:
|
The Virtual Craniofacial Patient: 3D Jaw Modeling and Animation
|
Publication: Stud Health Technol Inform. 2003;94:65-71. PMID: 15455866 | PDF Authors: Enciso R, Memon A, Fidaleo DA, Neumann U, Mah J. Institution: Craniofacial Virtual Reality Laboratory, University of Southern California, CA, USA. Background/Purpose: Recent developments in technology and software are providing better data and methods to facilitate research in biomedical modeling and simulation. In the area of segmentation, original methods involved the time-consuming task of manually tracing structures from slice to slice. This process is now possible with significantly less interaction from the user. Programs such as 3D Slicer, Mimics (Materialise N.V., Heverlee, Belgium) and Amira 2.3 (TGS) provide semi-automatic image-processing-based segmentation and modeling from CT images. These programs use the Generalized Marching Cubes algorithm to create a polygonal wireframe mesh of the segmented area and export a model in STL or other formats. Funding:
|
2002
A 3D Fiber Model of the Human Brainstem
|
Publication: Comput Med Imaging Graph. 2002 Nov-Dec;26(6):439-44. PMID: 12453507 | PDF Authors: Axer H, Leunert M, Mürköster M, Grässel D, Larsen L, Griffin LD, Graf v Keyserlingk D. Institution: Department of Neurology, Friedrich-Schiller-University, Jena, Germany. Background/Purpose: A new neuroanatomic approach to evaluate the fiber orientation in gross histological sections of the human brain was developed. Serial sections of a human brainstem were used to derive fiber orientation maps by analysis of polarized light sequences of these sections. Fiber inclination maps visualize angles of inclination, and fiber direction maps show angles of direction. These angles define vectors which can be visualized as RGB-colors. The serial sections were aligned to each other using the minimized Euclidian distance as fit criterion. In the 3D data set of the human brainstem the major fiber tracts were segmented, and three-dimensional models of these fiber tracts were generated. The presented results demonstrate that two kinds of fiber atlases are feasible: a fiber orientation atlas representing a vector in each voxel, which shows the nerve fiber orientation, and a volume-based atlas representing the major fiber tracts. These models can be used for the evaluation of diffusion tensor data as well as for neurosurgical planning. |
3D Visualization of the Middle Ear and Adjacent Structures Using Reconstructed Multi-slice CT Datasets, Correlating 3D Images and Virtual Endoscopy to the 2D Cross-sectional Images
|
Publication: Neuroradiology. 2002 Sep;44(9):783-90. PMID: 12221454 | PDF Authors: Rodt T, Ratiu P, Becker H, Bartling S, Kacher DF, Anderson M, Jolesz FA, Kikinis R. Institution: Department of Neuroradiology, Hannover Medical School, Hannover, Germany. Background/Purpose: The 3D imaging of the middle ear facilitates better understanding of the patient's anatomy. Cross-sectional slices, however, often allow a more accurate evaluation of anatomical structures, as some detail may be lost through post-processing. In order to demonstrate the advantages of combining both approaches, we performed computed tomography (CT) imaging in two normal and 15 different pathological cases, and the 3D models were correlated to the cross-sectional CT slices. Reconstructed CT datasets were acquired by multi-slice CT. Post-processing was performed using the in-house software 3D Slicer, applying thresholding and manual segmentation. 3D models of the individual anatomical structures were generated and displayed in different colors. The display of relevant anatomical and pathological structures was evaluated in the greyscale 2D slices, 3D images, and the 2D slices showing the segmented 2D anatomy in different colors for each structure. Correlating 2D slices to the 3D models and virtual endoscopy helps to combine the advantages of each method. As generating 3D models can be extremely time-consuming, this approach can be a clinically applicable way of gaining a 3D understanding of the patient's anatomy by using models as a reference. Furthermore, it can help radiologists and otolaryngologists evaluating the 2D slices by adding the correct 3D information that would otherwise have to be mentally integrated. The method can be applied to radiological diagnosis, surgical planning, and especially, to teaching. |
2001
Serial Intraoperative Magnetic Resonance Imaging of Brain Shift
|
Publication: Neurosurgery. 2001 Apr;48(4):787-97. PMID: 11322439 | PDF Authors: Nabavi A, Black PM, Gering DT, Westin C-F, Mehta V, Pergolizzi RS Jr, Ferrant M, Warfield SK, Hata N, Schwartz RB, Wells WM III, Kikinis R, Jolesz FA. Institution: Division of Neurosurgery, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: A major shortcoming of image-guided navigational systems is the use of preoperatively acquired image data, which does not account for intraoperative changes in brain morphology. The occurrence of these surgically induced volumetric deformations ("brain shift") has been well established. Maximal measurements for surface and midline shifts have been reported. There has been no detailed analysis, however, of the changes that occur during surgery. The use of intraoperative magnetic resonance imaging provides a unique opportunity to obtain serial image data and characterize the time course of brain deformations during surgery. The vertically open intraoperative magnetic resonance imaging system (SignaSP, 0.5 T; GE Medical Systems, Milwaukee, WI) permits access to the surgical field and allows multiple intraoperative image updates without the need to move the patient. We developed volumetric display software, the 3D Slicer, that allows quantitative analysis of the degree and direction of brain shift. For 25 patients, four or more intraoperative volumetric image acquisitions were extensively evaluated. Serial acquisitions allow comprehensive sequential descriptions of the direction and magnitude of intraoperative deformations. Brain shift occurs at various surgical stages and in different regions. Surface shift occurs throughout surgery and is mainly attributable to gravity. Subsurface shift occurs during resection and involves collapse of the resection cavity and intraparenchymal changes that are difficult to model. Brain shift is a continuous dynamic process that evolves differently in distinct brain regions. Therefore, only serial imaging or continuous data acquisition can provide consistently accurate image guidance. Furthermore, only serial intraoperative magnetic resonance imaging provides an accurate basis for the computational analysis of brain deformations, which might lead to an understanding and eventual simulation of brain shift for intraoperative guidance. Funding:
|
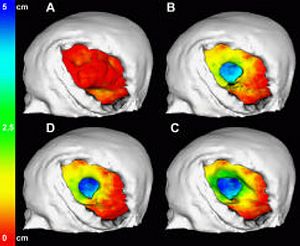 Color-coded models for the evaluation of successive surface deformations. The brain surfaces were extracted from the 3D volume SPGRs for all time points. The surface displacement from stage to stage was automatically calculated and color-coded. The color encodes depths from red (0 mm) to green (2.5 cm) to blue (5 cm). The color-coding was projected onto the model of the brain at that respective stage of the surgery. |
2000
Image-guided Therapy and Intraoperative MRI in Neurosurgery
|
Publication: Minim Invasive Ther Allied Technol. 2000;9(3-4):277-86. PMID: 20156025 Authors: Nabavi A, Mamisch CT, Gering DT, Kacher DF, Pergolizzi RS, Wells WM 3rd, Kikinis R, Black PM, Jolesz FA. Institution: Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Computer-assisted 3D planning, navigation and the possibilities offered by intra-operative imaging updates have made a large impact on neurological surgery. Three-dimensional rendering of complex medical image information, as well as co-registration of multimodal sources has reached a highly sophisticated level. When introduced into surgical navigation however, this pre-operative data is unable to account for intra-operative changes, ('brain-shift'). To update structural information during surgery, an open-configured, intra-operative MRI (Signa SP, 0.5 T) was realized at our institution in 1995. The design, advantages, limitations and current applications of this system are discussed, with emphasis on the integration of imaging into procedures. We also introduce our integrated platform for intra-operative visualization and navigation, the 3D Slicer. Funding:
|