Difference between revisions of "Main Page/SlicerCommunity"
| Line 174: | Line 174: | ||
Conclusions: | Conclusions: | ||
This work describes an easily accessible virtual bronchoscopy system for navigation in the lung. The system provides the user with a complete set of tools that facilitate navigation towards user-selected regions of interest. Results from ex vivo and in vivo studies showed that the system opens the way for potential future work with virtual navigation for safe and reliable airway disease diagnosis. | This work describes an easily accessible virtual bronchoscopy system for navigation in the lung. The system provides the user with a complete set of tools that facilitate navigation towards user-selected regions of interest. Results from ex vivo and in vivo studies showed that the system opens the way for potential future work with virtual navigation for safe and reliable airway disease diagnosis. | ||
| + | |} | ||
| + | |||
| + | ==Visualization of the 3D Dosimetry for a Leipzig Brachytherapy Applicator Using 3D Slicer== | ||
| + | |||
| + | {|width="100%" | ||
| + | | | ||
| + | '''Publication:''' IJ Brachytherapy 2016 May-June; 15(S1):S148. | [[media:Deshazer-Brachytherapy2016.pdf| PDF]] | ||
| + | |||
| + | '''Authors:''' Deshazer G, Merck D, Collins S, Puthawala YM, Cobian JG. | ||
| + | |||
| + | '''Institution:''' Diagnostic Imaging, Rhode Island Hospital, Providence, RI, USA. | ||
| + | |||
| + | '''Background/Purpose:''' Surface brachytherapy (BT) is an alternative to electron beam | ||
| + | therapy (EBRT) for the treatment of superficial skin lesions. Elekta’s | ||
| + | (Elekta AB, Stockholm, Sweden) high dose-rate (HDR) BT solution | ||
| + | utilizes conical surface applicators (Leipzig) connected to an 192-Ir | ||
| + | remote afterloader with treatment planning accomplished using | ||
| + | nomograms derived from Monte Carlo simulations. Since this approach | ||
| + | provides no 3D dosimetry, prospective and retrospective analysis of the | ||
| + | treatment volume and normal tissue coverage is not possible. To facilitate | ||
| + | such analysis, we have developed a work flow for 3D Slicer [1] and | ||
| + | SlicerRT [2] plug-in to import, view and calculate dose-volume | ||
| + | histograms (DVH) for this BT application. | ||
| + | Method: A HDR surface BT treatment plan for a superficial nose lesion was | ||
| + | selected from our clinical database for this proof-of-principle study. A 3D | ||
| + | CT dataset of the patient, with a fiducial marker placed on the area of | ||
| + | palpable disease, was acquired at the beginning of the BT course to | ||
| + | ascertain the required depth of treatment, 3mm. Using this information, a | ||
| + | clinical treatment volume (CTV) was created to roughly approximate | ||
| + | desired clinical coverage. Matlab (The MathWorks, Inc., Natick, MA) | ||
| + | was used to create a 3D dose-rate distribution using the Leipzig ‘‘H2’’ | ||
| + | applicator dose specifications presented by Perez-Calatayud et al. [1]. | ||
| + | This distribution was scaled according to the delivered source dose rate | ||
| + | and treatment prescription, 0.32 cGy h-1 U-1 and 400 cGy x 10, | ||
| + | respectively. The dose distribution was imported into 3D Slicer and | ||
| + | registered to the image set manually, using the known geometry of the | ||
| + | applicator and radio-opaque fiducial marker as landmarks. Isodose | ||
| + | visualization and DVH were calculated for the CTV using SlicerRT. | ||
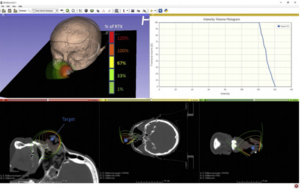
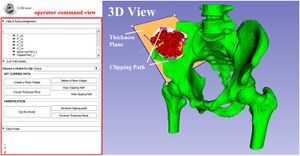
| + | Results: Figure 1 shows the relative 3D isodose distribution and resultant | ||
| + | CTV DVH using this method. For this application, 100% of the | ||
| + | hypothetical CTV receives prescription dose. The homogenous 3D dose | ||
| + | distribution is able to be visualized on synthetic 2D axial, coronal and | ||
| + | sagittal planes. | ||
| + | Conclusion: This proof-of-principle investigation demonstrated the ability | ||
| + | to visualize 3D dose distributions and calculate resultant DVH for | ||
| + | segmented structures using a widely-available, non-commercial software | ||
| + | package. With further development, this method has potential for | ||
| + | providing more accurate spatial dose estimates for patient treatments and | ||
| + | advance superficial HDR BT treatment planning to align with the current, | ||
| + | clinically-utilized 3D treatment planning paradigms used for | ||
| + | gynecological, prostate and breast HDR BT. Furthermore, this technique | ||
| + | may serve as a platform for the development and verification of modelbased, | ||
| + | inhomogenous dose calculation algorithms for superficial BT | ||
| + | applications. | ||
| + | |||
| + | |align="right"|[[image:Deshazer-Brachytherapy2016-fig.png|thumb|300px| relative 3D isodose distribution and resultant CTV DVH using this method. For this application, 100% of the | ||
| + | hypothetical CTV receives prescription dose. The homogenous 3D dose distribution is able to be visualized on synthetic 2D axial, coronal and sagittal planes.]] | ||
|} | |} | ||
Revision as of 16:56, 12 August 2016
Home < Main Page < SlicerCommunityContents
- 1 3D Slicer Enabled Research
- 2 2016
- 2.1 Evaluating the Utility of "3D Slicer" as a Fast and Independent Tool to Assess Intrafractional Organ Dose Variations in Gynecological Brachytherapy
- 2.2 Quantification of Diaphragm Mechanics in Pompe Disease using Dynamic 3D MRI
- 2.3 Development of a Nomogram Combining Clinical Staging with 18F-FDG PET/CT Image Features in Non-small-cell Lung Cancer Stage I-III.
- 2.4 Patient and Aneurysm Characteristics Associated with Rupture Risk of Multiple Intracranial Aneurysms in the Anterior Circulation System
- 2.5 Subregional Shape Alterations in the Amygdala in Patients with Panic Disorder
- 2.6 3D Mandibular Superimposition: Comparison of Regions of Reference for Voxel-Based Registration
- 2.7 Morphological and Volumetric Assessment of Cerebral Ventricular System with 3D Slicer Software
- 2.8 Pre-clinical Validation of Virtual Bronchoscopy using 3D Slicer
- 2.9 Visualization of the 3D Dosimetry for a Leipzig Brachytherapy Applicator Using 3D Slicer
- 2.10 Common 3-dimensional Coordinate System for Assessment of Directional Changes
- 2.11 3D Printing and 3D Slicer - Powerful Tools in Understanding and Treating Structural Lung Disease
- 2.12 STN-DBS Reduces Saccadic Hypometria but Not Visuospatial Bias in Parkinson's Disease Patients
- 2.13 Low-cost Interactive Image-based Virtual Endoscopy for the Diagnosis and Surgical Planning of Suprasellar Arachnoid Cysts
- 2.14 A Method for the Assessment of Time-varying Brain Shift during Navigated Epilepsy Surgery
- 2.15 Deformable Image Registration with a Featurelet Algorithm: Implementation as a 3D Slicer Extension and Validation
- 2.16 Accuracy of Lesion Boundary Tracking in Navigated Breast Tumor Excision
- 2.17 Effects of Voxelization on Dose Volume Histogram Accuracy
- 2.18 Extracted Magnetic Resonance Texture Features Discriminate between Phenotypes and are Associated with Overall Survival in Glioblastoma Multiforme Patients
- 2.19 Real-time Self-calibration of a Tracked Augmented Reality Display
- 2.20 Accuracy of Open-Source Software Segmentation and Paper-based Printed Three-Dimensional Models
- 2.21 Validation of a Novel Geometric Coordination Registration using Manual and Semi-automatic Registration in Cone-beam Computed Tomogram
- 2.22 Multi Texture Analysis of Colorectal Cancer Continuum using Multispectral Imagery
- 2.23 Cranial Anatomy and Palaeoneurology of the Archosaur Riojasuchus tenuisceps from the Los Colorados Formation, La Rioja, Argentina
- 2.24 Diffusion Tensor Imaging Assessment of Microstructural Brainstem Integrity in Chiari Malformation Type I.
- 2.25 Large Area 3-D Optical Coherence Tomography Imaging of Lumpectomy Specimens for Radiation Treatment Planning
- 2.26 Development and Evaluation of an Open-Source 3D Virtual Simulator with Integrated Motion-Tracking as a Teaching Tool for Pedicle Screw Insertion
- 2.27 Effect of Decompressive Craniectomy on Perihematomal Edema in Patients with Intracerebral Hemorrhage
- 2.28 Current Smoking Status is Associated with Lower Quantitative CT Measures of Emphysema and Gas Trapping
- 2.29 A Proposed Method for Accurate 3D Analysis of Cochlear Implant Migration using Fusion of Cone Beam CT
- 2.30 Boolean Combinations of Implicit Functions for Model Clipping in Computer-Assisted Surgical Planning
- 2.31 Three-Dimensional Visualization of the Distribution of Melanin-Concentrating Hormone Producing Neurons in the Mouse Hypothalamus
- 2.32 In Vivo Visualization of the Facial Nerve in Patients with Acoustic Neuroma using Diffusion Tensor Imaging-Based Fiber Tracking
- 2.33 Optic Nerve Tractography Prediction of Visual Deficit in Pituitary Macroadenoma
3D Slicer Enabled Research
3D Slicer is a free open source software package distributed under a BSD style license. The majority of funding for the development of 3D slicer comes from a number of grants and contracts from the National Institutes of Health. See Slicer Acknowledgments for more information.
This page focuses on research that was done outside of our immediate collaboration community. That community is represented in the publication database.
We invite you to provide information on how you are using 3D Slicer to produce peer-reviewed research. Information about the scientific impact of this tool is helpful in raising funding for the continued support.
2015 :: 2014-2011 :: 2010-2005
2016
Evaluating the Utility of "3D Slicer" as a Fast and Independent Tool to Assess Intrafractional Organ Dose Variations in Gynecological Brachytherapy
|
Publication: Brachytherapy. 2016 Jul-Aug;15(4):514-23. PMID: 27180127 Authors: Siavashpour Z, Aghamiri MR, Jaberi R, Dehghan-Manshadi HR, Sedaghat M, Kirisits C. Institution: Department of Medical Radiation Engineering, Shahid Beheshti University, Tehran, Iran. Background/Purpose: To demonstrate the utility of 3D Slicer for easy treatment verification by comparing dose-volume histograms (DVHs) calculated on pretreatment and posttreatment images. Methods and Materials: Thirty cervical cancer patients were CT scanned twice: first for treatment planning and a second time after the dose delivery. The initial plan was manually duplicated on the posttreatment image set in Flexiplan treatment planning system, and DVH parameters were calculated. Pretreatment and posttreatment images, organ structures, and plan data were exported from the treatment planning system to 3D Slicer to validate DVH parameter calculation with 3D Slicer. The gamma analysis was used to compare Flexiplan and 3D Slicer DVHs. Posttreatment images were rigidly fused on the initial CT to automatically transfer the data of the pretreatment plan onto the posttreatment images. DVH parameters were calculated in 3D Slicer for both image sets, and their relative variations were compared. Results: In calculating DVH parameter variations, no significant differences were observed between Flexiplan and 3D Slicer. Where the registration accuracy was better than 0.03, they returned similar results for D2 cm3 of bladder, rectum, and sigmoid. Mean and standard deviation of DVH parameters were calculated on pretreatment and posttreatment images for several organs; both the manually duplicated plan and the automatically registered plan in SlicerRT returned comparable relative variations of these parameters. For 88% of the organs, more than 95% of the DVH dose bins passed the gamma analysis. Conclusions: We tested an automated DVH assessment method with an imaging freeware, 3D Slicer, for use in image-guided adaptive brachytherapy. SlicerRT is a viable verification tool to report and detect DVH variations between different contoured images series. |
Quantification of Diaphragm Mechanics in Pompe Disease using Dynamic 3D MRI
|
Publication: PLoS One. 2016 Jul 8;11(7):e0158912. PMID: 27391236| PDF Authors: Mogalle K, Perez-Rovira A, Ciet P, Wens SC, van Doorn PA, Tiddens HA, van der Ploeg AT, de Bruijne M. Institution: Biomedical Imaging Group Rotterdam, Departments of Medical Informatics & Radiology, Erasmus MC, Rotterdam, the Netherlands. Background/Purpose: Diaphragm weakness is the main reason for respiratory dysfunction in patients with Pompe disease, a progressive metabolic myopathy affecting respiratory and limb-girdle muscles. Since respiratory failure is the major cause of death among adult patients, early identification of respiratory muscle involvement is necessary to initiate treatment in time and possibly prevent irreversible damage. In this paper we investigate the suitability of dynamic MR imaging in combination with state-of-the-art image analysis methods to assess respiratory muscle weakness. Methods: The proposed methodology relies on image registration and lung surface extraction to quantify lung kinematics during breathing. This allows for the extraction of geometry and motion features of the lung that characterize the independent contribution of the diaphragm and the thoracic muscles to the respiratory cycle. Results: Results in 16 3D+t MRI scans (10 Pompe patients and 6 controls) of a slow expiratory maneuver show that kinematic analysis from dynamic 3D images reveals important additional information about diaphragm mechanics and respiratory muscle involvement when compared to conventional pulmonary function tests. Pompe patients with severely reduced pulmonary function showed severe diaphragm weakness presented by minimal motion of the diaphragm. In patients with moderately reduced pulmonary function, cranial displacement of posterior diaphragm parts was reduced and the diaphragm dome was oriented more horizontally at full inspiration compared to healthy controls. Conclusion: Dynamic 3D MRI provides data for analyzing the contribution of both diaphragm and thoracic muscles independently. The proposed image analysis method has the potential to detect less severe diaphragm weakness and could thus be used to determine the optimal start of treatment in adult patients with Pompe disease in prospect of increased treatment response. Funding:
|
 Mesh representation of 3D lung segmentation. A trained medical observer manually segmented right and left lung in both static scans (inspiration and expiration) of each subject by tracing the lung surface in every second axial slice using 3D Slicer. |
Development of a Nomogram Combining Clinical Staging with 18F-FDG PET/CT Image Features in Non-small-cell Lung Cancer Stage I-III.
|
Publication: Eur J Nucl Med Mol Imaging. 2016 Jul;43(8):1477-85. PMID: 26896298 Authors: Desseroit MC, Visvikis D, Tixier F, Majdoub M, Perdrisot R, Guillevin R, Cheze Le Rest, Hatt M. Institution: Nuclear Medicine, University Hospital, Poitiers, France. Background/Purpose: Our goal was to develop a nomogram by exploiting intratumor heterogeneity on CT and PET images from routine 18F-FDG PET/CT acquisitions to identify patients with the poorest prognosis. Methods: This retrospective study included 116 patients with NSCLC stage I, II or III and with staging 18F-FDG PET/CT imaging. Primary tumor volumes were delineated using the FLAB algorithm and 3D Slicer on PET and CT images, respectively. PET and CT heterogeneities were quantified using texture analysis. The reproducibility of the CT features was assessed on a separate test-retest dataset. The stratification power of the PET/CT features was evaluated using the Kaplan-Meier method and the log-rank test. The best standard metric (functional volume) was combined with the least redundant and most prognostic PET/CT heterogeneity features to build the nomogram. Results: PET entropy and CT zone percentage had the highest complementary values with clinical stage and functional volume. The nomogram improved stratification amongst patients with stage II and III disease, allowing identification of patients with the poorest prognosis (clinical stage III, large tumor volume, high PET heterogeneity and low CT heterogeneity). Conclusion: Intratumor heterogeneity quantified using textural features on both CT and PET images from routine staging18F-FDG PET/CT acquisitions can be used to create a nomogram with higher stratification power than staging alone. |
Patient and Aneurysm Characteristics Associated with Rupture Risk of Multiple Intracranial Aneurysms in the Anterior Circulation System
|
Publication: Acta Neurochir (Wien). 2016 Jul;158(7):1367-75. PMID: 27165300 Authors: Jiang H, Weng YX, Zhu Y, Shen J, Pan JW, Zhan RY. Institution: Department of Neurosurgery, The First Affiliated Hospital, School of Medicine, Zhejiang University, Zhejiang, China. Background/Purpose: Multiple intracranial aneurysms (MIAs) are associated with poorer outcomes after rupture than are single intracranial aneurysms (SIAs). Although the risk factors for intracranial aneurysm rupture have been widely investigated, few studies have focused on MIAs. Thus, the present study aimed to determine whether there are differences in the patient and aneurysm characteristics between those with ruptured and unruptured anterior circulation MIAs (AC-MIAs). Method: The present study included 97 patients with AC-MIAs (58 ruptured, 39 unruptured). Data regarding patient characteristics, aneurysm location, mirror aneurysms (MirAns), and bleb formations were collected from medical records and angiography images. Three-dimensional (3D) geometries generated with a 3D Slicer were evaluated to determine the range of morphological parameters. A univariate analysis was conducted to identify significant differences between the groups and receiver-operating characteristic (ROC) analyses were performed for each morphological parameter. Results: There are significantly fewer patients younger than 40 years of age in the ruptured group (P = 0.04); although the groups did not significantly differ with regard to smoking and hypertension, the ruptured group included significantly more current smokers who smoked more than 20 cigarettes per day (P = 0.025) and significantly more patients with a history of hypertension but an irregular use of anti-hypertensive medications (P = 0.043). Ruptured AC-MIAs were more likely to be located in the internal carotid artery (ICA) communicating artery (ICA C7) and anterior communicating artery (AComA; P = 0.000), to have formed a pair of MirAns (P = 0.001), and to have a bleb formation (P = 0.000). In terms of morphological parameters, the two groups differed significantly regarding aneurysm size (P = 0.000), neck width (P = 0.016), bottleneck factor (BNF; P = 0.000), height/width ratio (H/W; P = 0.031), aspect ratio (AR; P = 0.000) and size ratio (SR; P = 0.000). Additionally, the ROC analyses revealed that the optimal threshold size for rupture was 4.00 mm and that the SR had the highest area under the curve (AUC) value (0.826). Conclusions: The present study found that current smokers who smoked more than 20 cigarettes per day and those with hypertension but an irregular use of anti-hypertensive medications were more likely to suffer from rupture. Aneurysm location and bleb formation were closely related to the rupture of AC-MIAs, and SR was a better predictor of AC-MIAs rupture status than size, neck width, BNF, H/W and AR. These findings should be verified by future prospective follow-up studies of AC-MIAs. |
Subregional Shape Alterations in the Amygdala in Patients with Panic Disorder
|
Publication: PLoS One. 2016 Jun 23;11(6):e0157856. PMID: 27336300| PDF Authors: Yoon S, Kim JE, Kim GH, Kang HJ, Kim BR, Jeon S, Im JJ, Hyun H, Moon S, Lim SM, Lyoo IK. Institution: Ewha Brain Institute, Ewha Womans University, Seoul, South Korea. Background/Purpose: The amygdala has been known to play a pivotal role in mediating fear-related responses including panic attacks. Given the functionally distinct role of the amygdalar subregions, morphometric measurements of the amygdala may point to the pathophysiological mechanisms underlying panic disorder. The current study aimed to determine the global and local morphometric alterations of the amygdala related to panic disorder. Methods: Volumetric and surface-based morphometric approach to high-resolution three-dimensional T1-weighted images was used to examine the structural variations of the amygdala, with respect to extent and location, in 23 patients with panic disorder and 31 matched healthy individuals. Results: There were no significant differences in bilateral amygdalar volumes between patients with panic disorder and healthy individuals despite a trend-level right amygdalar volume reduction related to panic disorder (right, β = -0.23, p = 0.09, Cohen's d = 0.51; left, β = -0.18, p = 0.19, Cohen's d = 0.45). Amygdalar subregions were localized into three groups including the superficial, centromedial, and laterobasal groups based on the cytoarchitectonically defined probability map. Surface-based morphometric analysis revealed shape alterations in the laterobasal and centromedial groups of the right amygdala in patients with panic disorder (false discovery rate corrected p < 0.05). Conclusions: The current findings suggest that subregion-specific shape alterations in the right amygdala may be involved in the development and maintenance of panic disorder, which may be attributed to the cause or effects of amygdalar hyperactivation. Funding:
|
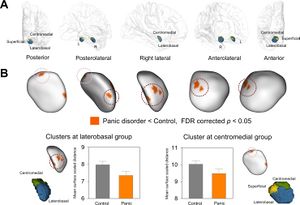 Clusters showing significant surface inward deformation in patients with panic disorder relative to healthy controls. (A) Surface rendering of cytoarchitectonically defined probabilistic maps of the superficial, centromedial, and laterobasal groups of the amygdala transposed onto the amygdalar template is presented. (B) Four clusters of inward deformation related to panic disorder at FDR corrected p < 0.05 are overlaid on the amygdalar template. Bar graphs show that mean surface scaled distance of clusters in the laterobasal and centromedial groups of the amygdala was lower in patients with panic disorder than in healthy individuals. Error bars indicate 95% confidence intervals. Abbreviations: FDR, false discovery rate. Surface rendering of amygdalar nuclei groups with 40% probability was performed using 3D Slicer and each nuclei group was manually transposed onto the amygdalar template (B). |
3D Mandibular Superimposition: Comparison of Regions of Reference for Voxel-Based Registration
|
Publication: PLoS One. 2016 Jun 23;11(6):e0157625. PMID: 27336366| PDF Authors: Ruellas AC, Yatabe MS, Souki BQ, Benavides E, Nguyen T, Luiz RR, Franchi L, Cevidanes LH. Institution: School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil. Background/Purpose: The aim was to evaluate three regions of reference (Björk, Modified Björk and mandibular Body) for mandibular registration testing them in a patients' CBCT sample. Methods: Mandibular 3D volumetric label maps were built from CBCTs taken before (T1) and after treatment (T2) in a sample of 16 growing subjects and labeled with eight landmarks. Registrations of T1 and T2 images relative to the different regions of reference were performed, and 3D surface models were generated. Seven mandibular dimensions were measured separately for each time-point (T1 and T2) in relation to a stable reference structure (lingual cortical of symphysis), and the T2-T1 differences were calculated. These differences were compared to differences measured between the superimposed T2 (generated from different regions of reference: Björk, Modified Björk and Mandibular Body) over T1 surface models. ICC and the Bland-Altman method tested the agreement of the changes obtained by nonsuperimposition measurements from the patients' sample, and changes between the overlapped surfaces after registration using the different regions of reference. Results: The Björk region of reference (or mask) did work properly only in 2 of 16 patients. Evaluating the two other masks (Modified Björk and Mandibular body) on patients' scans registration, the concordance and agreement of the changes obtained from superimpositions (registered T2 over T1) compared to results obtained from non superimposed T1 and T2 separately, indicated that Mandibular Body mask displayed more consistent results. Conclusions: The mandibular body mask (mandible without teeth, alveolar bone, rami and condyles) is a reliable reference for 3D regional registration. Funding:
|
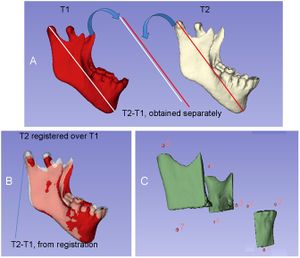 A) Representation of the measurements obtained independently from T1 and T2 and their difference; B) Representation of the T2-T1 differences based on mandibular registration; C) Partial 3D surface model of the mandible and representation of the 8 landmarks used for the measurements. A fully automated voxel-wise growing registration method was performed using 3D Slicer software. |
Morphological and Volumetric Assessment of Cerebral Ventricular System with 3D Slicer Software
|
Publication: J Med Syst. 2016 Jun;40(6):154. PMID: 27147517 Authors: Gonzalo Domínguez M, Hernández C, Ruisoto P, Juanes JA, Prats A, Hernández T. Institution: Medical Care Center in Zamora, Salamanca, Spain. Background/Purpose: We present a technological process based on the 3D Slicer software for the three-dimensional study of the brain's ventricular system with teaching purposes. It values the morphology of this complex brain structure, as a whole and in any spatial position, being able to compare it with pathological studies, where its anatomy visibly changes. 3D Slicer was also used to obtain volumetric measurements in order to provide a more comprehensive and detail representation of the ventricular system. We assess the potential this software has for processing high resolution images, taken from Magnetic Resonance and generate the three-dimensional reconstruction of ventricular system. |
Pre-clinical Validation of Virtual Bronchoscopy using 3D Slicer
|
Publication: Int J Comput Assist Radiol Surg. 2016 Jun 21. PMID: 27325238 Authors: Nardelli P, Jaeger A, O'Shea C, Khan KA, Kennedy MP, Cantillon-Murphy P. Institution: School of Engineering, University College Cork, College Road, Cork, Ireland. Background/Purpose: Lung cancer still represents the leading cause of cancer-related death, and the long-term survival rate remains low. Computed tomography (CT) is currently the most common imaging modality for lung diseases recognition. The purpose of this work was to develop a simple and easily accessible virtual bronchoscopy system to be coupled with a customized electromagnetic (EM) tracking system for navigation in the lung and which requires as little user interaction as possible, while maintaining high usability. Methods: The proposed method has been implemented as an extension to the open-source platform, 3D Slicer. It creates a virtual reconstruction of the airways starting from CT images for virtual navigation. It provides tools for pre-procedural planning and virtual navigation, and it has been optimized for use in combination with a [Formula: see text] of freedom EM tracking sensor. Performance of the algorithm has been evaluated in ex vivo and in vivo testing. Results: During ex vivo testing, nine volunteer physicians tested the implemented algorithm to navigate three separate targets placed inside a breathing pig lung model. In general, the system proved easy to use and accurate in replicating the clinical setting and seemed to help choose the correct path without any previous experience or image analysis. Two separate animal studies confirmed technical feasibility and usability of the system. Conclusions: This work describes an easily accessible virtual bronchoscopy system for navigation in the lung. The system provides the user with a complete set of tools that facilitate navigation towards user-selected regions of interest. Results from ex vivo and in vivo studies showed that the system opens the way for potential future work with virtual navigation for safe and reliable airway disease diagnosis. |
Visualization of the 3D Dosimetry for a Leipzig Brachytherapy Applicator Using 3D Slicer
|
Publication: IJ Brachytherapy 2016 May-June; 15(S1):S148. | PDF Authors: Deshazer G, Merck D, Collins S, Puthawala YM, Cobian JG. Institution: Diagnostic Imaging, Rhode Island Hospital, Providence, RI, USA. Background/Purpose: Surface brachytherapy (BT) is an alternative to electron beam therapy (EBRT) for the treatment of superficial skin lesions. Elekta’s (Elekta AB, Stockholm, Sweden) high dose-rate (HDR) BT solution utilizes conical surface applicators (Leipzig) connected to an 192-Ir remote afterloader with treatment planning accomplished using nomograms derived from Monte Carlo simulations. Since this approach provides no 3D dosimetry, prospective and retrospective analysis of the treatment volume and normal tissue coverage is not possible. To facilitate such analysis, we have developed a work flow for 3D Slicer [1] and SlicerRT [2] plug-in to import, view and calculate dose-volume histograms (DVH) for this BT application. Method: A HDR surface BT treatment plan for a superficial nose lesion was selected from our clinical database for this proof-of-principle study. A 3D CT dataset of the patient, with a fiducial marker placed on the area of palpable disease, was acquired at the beginning of the BT course to ascertain the required depth of treatment, 3mm. Using this information, a clinical treatment volume (CTV) was created to roughly approximate desired clinical coverage. Matlab (The MathWorks, Inc., Natick, MA) was used to create a 3D dose-rate distribution using the Leipzig ‘‘H2’’ applicator dose specifications presented by Perez-Calatayud et al. [1]. This distribution was scaled according to the delivered source dose rate and treatment prescription, 0.32 cGy h-1 U-1 and 400 cGy x 10, respectively. The dose distribution was imported into 3D Slicer and registered to the image set manually, using the known geometry of the applicator and radio-opaque fiducial marker as landmarks. Isodose visualization and DVH were calculated for the CTV using SlicerRT. Results: Figure 1 shows the relative 3D isodose distribution and resultant CTV DVH using this method. For this application, 100% of the hypothetical CTV receives prescription dose. The homogenous 3D dose distribution is able to be visualized on synthetic 2D axial, coronal and sagittal planes. Conclusion: This proof-of-principle investigation demonstrated the ability to visualize 3D dose distributions and calculate resultant DVH for segmented structures using a widely-available, non-commercial software package. With further development, this method has potential for providing more accurate spatial dose estimates for patient treatments and advance superficial HDR BT treatment planning to align with the current, clinically-utilized 3D treatment planning paradigms used for gynecological, prostate and breast HDR BT. Furthermore, this technique may serve as a platform for the development and verification of modelbased, inhomogenous dose calculation algorithms for superficial BT applications. |
Common 3-dimensional Coordinate System for Assessment of Directional Changes
|
Publication: Am J Orthod Dentofacial Orthop. 2016 May;149(5):645-56. PMID: 27131246 Authors: Ruellas AC, Tonello C, Gomes LR, Yatabe MS, Macron L, Lopinto J, Goncalves JR, Garib Carreira DG, Alonso N, Souki BQ, Coqueiro Rda S, Cevidanes LH. Institution: Federal University of Rio de Janeiro, Rio de Janeiro, Brazil. Background/Purpose: The aims of this study were to evaluate how head orientation interferes with the amounts of directional change in 3-dimensional (3D) space and to propose a method to obtain a common coordinate system using 3D surface models. Methods: Three-dimensional volumetric label maps were built for pretreatment (T1) and posttreatment (T2) from cone-beam computed tomography images of 30 growing subjects. Seven landmarks were labeled in all T1 and T2 volumetric label maps. Registrations of T1 and T2 images relative to the cranial base were performed, and 3D surface models were generated. All T1 surface models were moved by orienting the Frankfort horizontal, midsagittal, and transporionic planes to match the axial, sagittal, and coronal planes, respectively, at a common coordinate system in the 3D Slicer software (open-source, version 4.3.1). The matrix generated for each T1 model was applied to each corresponding registered T2 surface model, obtaining a common head orientation. The 3D differences between the T1 and registered T2 models, and the amounts of directional change in each plane of the 3D space, were quantified for before and after head orientation. Two assessments were performed: (1) at 1 time point (mandibular width and length), and (2) for longitudinal changes (maxillary and mandibular differences). The differences between measurements before and after head orientation were quantified. Statistical analysis was performed by evaluating the means and standard deviations with paired t tests (mandibular width and length) and Wilcoxon tests (longitudinal changes). For 16 subjects, 2 observers working independently performed the head orientations twice with a 1-week interval between them. Intraclass correlation coefficients and the Bland-Altman method tested intraobserver and interobserver agreements of the x, y, and z coordinates for 7 landmarks. Results: The 3D differences were not affected by the head orientation. The amounts of directional change in each plane of 3D space at 1 time point were strongly influenced by head orientation. The longitudinal changes in each plane of 3D space showed differences smaller than 0.5 mm. Excellent intraobserver and interobserver repeatability and reproducibility (>99%) were observed. Conclusions: The amount of directional change in each plane of 3D space is strongly influenced by head orientation. The proposed method of head orientation to obtain a common 3D coordinate system is reproducible. |
3D Printing and 3D Slicer - Powerful Tools in Understanding and Treating Structural Lung Disease
|
Publication: Chest. 2016 May;149(5):1136-42. PMID: 26976347. Authors: Cheng GZ, Jose Estepar RS, Folch E, Onieva JO, Gangadharan S, Majid A Institution: Division of Thoracic Surgery and Interventional Pulmonology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA. Background/Purpose: Recent advances in 3D printing industry has enabled clinicians to explore the use of 3D printing in pre-procedural planning, biomedical tissue modeling, and direct implantable device manufacturing. Despite the increase adoption of rapid prototyping and additive manufacturing techniques in the healthcare field, many physicians lack the technical skillset to utilize this exciting and useful technology. Additionally, the growth in the 3D printing sector brings an ever-increasing number of 3D printers and printable materials. Therefore, it is important for clinicians to keep abreast with this rapidly developing field in order to stand to benefit. In this Ahead of the Curve, we review the history of 3D printing from its inception to most recent biomedical applications. Additionally, we will address some of the major barriers to wider adoption of the technology in medical field. Finally, we will provide an initial guide on 3D modeling and printing by demonstrating how to design personalized airway prosthesis via 3D Slicer. We hope this will reduce the barrier to utilization and increase clinician participation in the 3D printing healthcare sector. |
STN-DBS Reduces Saccadic Hypometria but Not Visuospatial Bias in Parkinson's Disease Patients
|
Publication: Front Behav Neurosci. 2016 May 3;10:85. PMID: 27199693. | PDF Authors: Fischer P, Ossandón JP, Keyser J, Gulberti A, Wilming N, Hamel W, Köppen J, Buhmann C, Westphal M, Gerloff C, Moll CK, Engel AK, König P. Institution: nstitute of Cognitive Science, University of OsnabrückOsnabrück, Germany; Medical Research Council Brain Network Dynamics Unit, University of OxfordOxford, UK. Background/Purpose: In contrast to its well-established role in alleviating skeleto-motor symptoms in Parkinson's disease, little is known about the impact of deep brain stimulation (DBS) of the subthalamic nucleus (STN) on oculomotor control and attention. Eye-tracking data of 17 patients with left-hemibody symptom onset was compared with 17 age-matched control subjects. Free-viewing of natural images was assessed without stimulation as baseline and during bilateral DBS. To examine the involvement of ventral STN territories in oculomotion and spatial attention, we employed unilateral stimulation via the left and right ventralmost contacts respectively. When DBS was off, patients showed shorter saccades and a rightward viewing bias compared with controls. Bilateral stimulation in therapeutic settings improved saccadic hypometria but not the visuospatial bias. At a group level, unilateral ventral stimulation yielded no consistent effects. However, the evaluation of electrode position within normalized MNI coordinate space revealed that the extent of early exploration bias correlated with the precise stimulation site within the left subthalamic area. These results suggest that oculomotor impairments "but not higher-level exploration patterns" are effectively ameliorable by DBS in therapeutic settings. Our findings highlight the relevance of the STN topography in selecting contacts for chronic stimulation especially upon appearance of visuospatial attention deficits. |
Low-cost Interactive Image-based Virtual Endoscopy for the Diagnosis and Surgical Planning of Suprasellar Arachnoid Cysts
|
Publication: World Neurosurg. 2016 Apr;88:76-82. PMID: 26732948 Authors: Li Y, Zhao Y, Zhang J, Zhang Z, Dong G, Wang Q, Liu L, Yu X, Xu B, Chen X. Institution: Department of Neurosurgery, People's Liberation Army General Hospital, Beijing, China. Background/Purpose: OBJECTIVE: To investigate the feasibility and reliability of virtual endoscopy (VE) as a rapid, low-cost and interactive tool for suprasellar arachnoid cysts (SACs) diagnosis and surgical planning. Methods: 18 SACs patients treated with endoscopic ventriculocystostomy were recruited, and same number of endoscopic third ventriculostomy treated patients was randomly selected as VE reconstruction control group. After loading their DICOM data into free software 3D Slicer, VE reconstruction was independently performed by 3 blinded clinicians and the time required for each reconstruction was recorded. Other 3 blinded senior neurosurgeons interactively graded the visibility of VE by watching video recordings of endoscopic procedures. Based on the visibility scores, Receiver Operating Characteristic (ROC) curve analysis was used to investigate the reliability of VE to diagnose SACs, and the Bland-Altman plot was employed to assess the VE's reliability for surgical planning. In addition, intra-class correlation coefficient (ICC) was calculated to estimate the consistency among the results of 3 reconstructing performers. Results: All 3 independent reconstructing performers successfully completed VE simulation for all cases, and the average reconstructing time was 10.2±9.7 minutes. The area under ROC curve of cyst's visibility score was 0.96, implying its diagnostic value of SACs. Bland-Altman plot indicated good agreement between VE and intraoperative viewings, suggesting the VE's anatomical accuracy for surgical planning. In addition, ICC was 0.81, which revealed excellent inter-performer consistency of our simulation method. Conclusion: This study substantiated the feasibility and reliability of VE as a rapid, low-cost and interactive modality for SACs diagnosis and surgical planning. |
|
Publication: Int J Comput Assist Radiol Surg. 2016 Mar;11(3):473-81. PMID: 26183148 Authors: De Momi E, Ferrigno G, Bosoni G, Bassanini P, Blasi P, Casaceli G, Fuschillo D, Castana L, Cossu M, Lo Russo G, Cardinale F. Institution: Department of Electronics, Information and Bioengineering (DEIB), Politecnico di Milano, Milan, Italy. Background/Purpose: Image guidance is widely used in neurosurgery. Tracking systems (neuronavigators) allow registering the preoperative image space to the surgical space. The localization accuracy is influenced by technical and clinical factors, such as brain shift. This paper aims at providing quantitative measure of the time-varying brain shift during open epilepsy surgery, and at measuring the pattern of brain deformation with respect to three potentially meaningful parameters: craniotomy area, craniotomy orientation and gravity vector direction in the images reference frame. Methods: We integrated an image-guided surgery system with 3D Slicer, an open-source package freely available in the Internet. We identified the preoperative position of several cortical features in the image space of 12 patients, inspecting both the multiplanar and the 3D reconstructions. We subsequently repeatedly tracked their position in the surgical space. Therefore, we measured the cortical shift, following its time-related changes and estimating its correlation with gravity and craniotomy normal directions. Results: The mean of the median brain shift amount is 9.64 mm ([Formula: see text] mm). The brain shift amount resulted not correlated with respect to the gravity direction, the craniotomy normal, the angle between the gravity and the craniotomy normal and the craniotomy area. Conclusions:Our method, which relies on cortex surface 3D measurements, gave results, which are consistent with literature. Our measurements are useful for the neurosurgeon, since they provide a continuous monitoring of the intra-operative sinking or bulking of the brain, giving an estimate of the preoperative images validity versus time. |
Deformable Image Registration with a Featurelet Algorithm: Implementation as a 3D Slicer Extension and Validation
|
Publication: Proc. SPIE 9784, Medical Imaging 2016 Mar; Image Processing, 97844B. Authors: Renner A, Furtado H, Seppenwoolde Y, Birkfellner W, Georg D. Institution: Medical University, Vienna, Austria. Background/Purpose: A radiotherapy (RT) treatment can last for several weeks. In that time organ motion and shape changes introduce uncertainty in dose application. Monitoring and quantifying the change can yield a more precise irradiation margin definition and thereby reduce dose delivery to healthy tissue and adjust tumor targeting. Deformable image registration (DIR) has the potential to fulfill this task by calculating a deformation field (DF) between a planning CT and a repeated CT of the altered anatomy. Application of the DF on the original contours yields new contours that can be used for an adapted treatment plan. DIR is a challenging method and therefore needs careful user interaction. Without a proper graphical user interface (GUI) a misregistration cannot be easily detected by visual inspection and the results cannot be fine-tuned by changing registration parameters. To provide a DIR algorithm with such a GUI available for everyone, we created the extension Featurelet-Registration for the open source software platform 3D Slicer. The registration logic is an upgrade of an in-house-developed DIR method, which is a featurelet-based piecewise rigid registration. The so called "featurelets" are equally sized rectangular subvolumes of the moving image which are rigidly registered to rectangular search regions on the fixed image. The output is a deformed image and a deformation field. Both can be visualized directly in 3D Slicer facilitating the interpretation and quantification of the results. For validation of the registration accuracy two deformable phantoms were used. The performance was benchmarked against a demons algorithm with comparable results. © (2016) COPYRIGHT Society of Photo-Optical Instrumentation Engineers (SPIE). Downloading of the abstract is permitted for personal use only. |
|
Publication: Proc. SPIE 9786, Medical Imaging 2016 Mar; Image-Guided Procedures, Robotic Interventions, and Modeling, 97860Y Authors: Heffernan E, Ungi T, Vaughan T, Pezeshki P, Lasso A, Gauvin G, Rudan J, Engel CJ, Morin E, Fichtinger G. Institution: Queen's University, Kingston, Canada. Background/Purpose: An electromagnetic navigation system for tumor excision in breast conserving surgery has recently been developed. Preoperatively, a hooked needle is positioned in the tumor and the tumor boundaries are defined in the needle coordinate system. The needle is tracked electromagnetically throughout the procedure to localize the tumor. However, the needle may move and the tissue may deform, leading to errors in maintaining a correct excision boundary. It is imperative to quantify these errors so the surgeon can choose an appropriate resection margin. Methods: A commercial breast biopsy phantom with several inclusions was used. Location and shape of a lesion before and after mechanical deformation were determined using 3D ultrasound volumes. Tumor location and shape were estimated from initial contours and tracking data. The difference in estimated and actual location and shape of the lesion after deformation was quantified using the Hausdorff distance. Data collection and analysis were done using our 3D Slicer software application and PLUS toolkit. Results: The deformation of the breast resulted in 3.72 mm (STD 0.67 mm) average boundary displacement for an isoelastic lesion and 3.88 mm (STD 0.43 mm) for a hyperelastic lesion. The difference between the actual and estimated tracked tumor boundary was 0.88 mm (STD 0.20 mm) for the isoelastic and 1.78 mm (STD 0.18 mm) for the hyperelastic lesion. Conclusion: The average lesion boundary tracking error was below 2mm, which is clinically acceptable. We suspect that stiffness of the phantom tissue affected the error measurements. Results will be validated in patient studies. © (2016) COPYRIGHT Society of Photo-Optical Instrumentation Engineers (SPIE). Downloading of the abstract is permitted for personal use only. |
Effects of Voxelization on Dose Volume Histogram Accuracy
|
Publication: Proc. SPIE 9786, Medical Imaging 2016 Mar; Image-Guided Procedures, Robotic Interventions, and Modeling, 97862O. Authors: Sunderland K, Pinter C, Lasso A, Fichtinger G. Institution: Queen's University, Kingston, Canada. Background/Purpose: In radiotherapy treatment planning systems, structures of interest such as targets and organs at risk are stored as 2D contours on evenly spaced planes. In order to be used in various algorithms, contours must be converted into binary label map volumes using voxelization. The voxelization process results in lost information, which has little effect on the volume of large structures, but has significant impact on small structures, which contain few voxels. Volume differences for segmented structures affects metrics such as dose volume histograms (DVH), which are used for treatment planning. Our goal is to evaluate the impact of voxelization on segmented structures, as well as how factors like voxel size affects metrics, such as DVH. Methods: We create a series of implicit functions, which represent simulated structures. These structures are sampled at varying resolutions, and compared to label maps with high sub-millimeter resolutions. We generate DVH and evaluate voxelization error for the same structures at different resolutions by calculating the agreement acceptance percentage between the DVH. Results: We implemented tools for analysis as modules in the SlicerRT toolkit based on the 3D Slicer platform. We found that there were large DVH variation from the baseline for small structures or for structures located in regions with a high dose gradient, potentially leading to the creation of suboptimal treatment plans. Conclusion: This work demonstrates that label map and dose volume voxel size is an important factor in DVH accuracy, which must be accounted for in order to ensure the development of accurate treatment plans. |
Extracted Magnetic Resonance Texture Features Discriminate between Phenotypes and are Associated with Overall Survival in Glioblastoma Multiforme Patients
|
Publication: Med Biol Eng Comput. 2016 Mar 10. PMID: 26960324 Authors: Chaddad A, Tanougast C. Institution: Laboratory of Design, Optimization and Modeling (LCOMS), University of Lorraine, 7 rue marconi, Metz, 57070, France. Background/Purpose: GBM is a markedly heterogeneous brain tumor consisting of three main volumetric phenotypes identifiable on magnetic resonance imaging: necrosis (vN), active tumor (vAT), and edema/invasion (vE). The goal of this study is to identify the three glioblastoma multiforme (GBM) phenotypes using a texture-based gray-level co-occurrence matrix (GLCM) approach and determine whether the texture features of phenotypes are related to patient survival. MR imaging data in 40 GBM patients were analyzed. Phenotypes vN, vAT, and vE were segmented in a preprocessing step using 3D Slicer for rigid registration by T1-weighted imaging and corresponding fluid attenuation inversion recovery images. The GBM phenotypes were segmented using 3D Slicer tools. Texture features were extracted from GLCM of GBM phenotypes. Thereafter, Kruskal-Wallis test was employed to select the significant features. Robust predictive GBM features were identified and underwent numerous classifier analyses to distinguish phenotypes. Kaplan-Meier analysis was also performed to determine the relationship, if any, between phenotype texture features and survival rate. The simulation results showed that the 22 texture features were significant with p value <0.05. GBM phenotype discrimination based on texture features showed the best accuracy, sensitivity, and specificity of 79.31, 91.67, and 98.75 %, respectively. Three texture features derived from active tumor parts: difference entropy, information measure of correlation, and inverse difference were statistically significant in the prediction of survival, with log-rank p values of 0.001, 0.001, and 0.008, respectively. Among 22 features examined, three texture features have the ability to predict overall survival for GBM patients demonstrating the utility of GLCM analyses in both the diagnosis and prognosis of this patient population. |
Real-time Self-calibration of a Tracked Augmented Reality Display
|
Publication: Proc. SPIE 9786, Medical Imaging 2016 Mar; Image-Guided Procedures, Robotic Interventions, and Modeling, 97860F. Authors: Baum Z, Lasso A, Ungi T, Fichtinger G. Institution: Laboratory for Percutaneous Surgery, Queen's University, Kingston, Canada. Background/Purpose: Augmented reality systems have been proposed for image-guided needle interventions but they have not become widely used in clinical practice due to restrictions such as limited portability, low display refresh rates, and tedious calibration procedures. We propose a handheld tablet-based self-calibrating image overlay system. Methods: A modular handheld augmented reality viewbox was constructed from a tablet computer and a semi-transparent mirror. A consistent and precise self-calibration method, without the use of any temporary markers, was designed to achieve an accurate calibration of the system. Markers attached to the viewbox and patient are simultaneously tracked using an optical pose tracker to report the position of the patient with respect to a displayed image plane that is visualized in real-time. The software was built using the open-source 3D Slicer application platform's SlicerIGT extension and the PLUS toolkit. Results: The accuracy of the image overlay with image-guided needle interventions yielded a mean absolute position error of 0.99 mm (95th percentile 1.93 mm) in-plane of the overlay and a mean absolute position error of 0.61 mm (95th percentile 1.19 mm) out-of-plane. This accuracy is clinically acceptable for tool guidance during various procedures, such as musculoskeletal injections. Conclusion: A self-calibration method was developed and evaluated for a tracked augmented reality display. The results show potential for the use of handheld image overlays in clinical studies with image-guided needle interventions. |
Accuracy of Open-Source Software Segmentation and Paper-based Printed Three-Dimensional Models
|
Publication: J Craniomaxillofac Surg. 2016 Feb;44(2):202-9. PMID: 26748414 Authors: Szymor P, Kozakiewicz M, Olszewski R. Institution: Department of Maxillofacial Surgery, Medical University of Lodz, Lodz, Poland. Background/Purpose: In this study, we aimed to verify the accuracy of models created with the help of open-source 3D Slicer 3.6.3 software (Surgical Planning Lab, Harvard Medical School, Harvard University, Boston, MA, USA) and the Mcor Matrix 300 paper-based 3D printer. Our study focused on the accuracy of recreating the walls of the right orbit of a cadaveric skull. Cone beam computed tomography (CBCT) of the skull was performed (0.25-mm pixel size, 0.5-mm slice thickness). Acquired DICOM data were imported into 3D Slicer 3.6.3 software, where segmentation was performed. A virtual model was created and saved as an .STL file and imported into Netfabb Studio professional 4.9.5 software. Three different virtual models were created by cutting the original file along three different planes (coronal, sagittal, and axial). All models were printed with a Selective Deposition Lamination Technology Matrix 300 3D printer using 80 gsm A4 paper. The models were printed so that their cutting plane was parallel to the paper sheets creating the model. Each model (coronal, sagittal, and axial) consisted of three separate parts (∼200 sheets of paper each) that were glued together to form a final model. The skull and created models were scanned with a three-dimensional (3D) optical scanner (Breuckmann smart SCAN) and were saved as .STL files. Comparisons of the orbital walls of the skull, the virtual model, and each of the three paper models were carried out with GOM Inspect 7.5SR1 software. Deviations measured between the models analyzed were presented in the form of a color-labelled map and covered with an evenly distributed network of points automatically generated by the software. An average of 804.43 ± 19.39 points for each measurement was created. Differences measured in each point were exported as a .csv file. The results were statistically analyzed using Statistica 10, with statistical significance set at p < 0.05. The average number of points created on models for each measurement was 804.43 ± 19.39; however, deviation in some of the generated points could not be calculated, and those points were excluded from further calculations. From 94% to 99% of the measured absolute deviations were <1 mm. The mean absolute deviation between the skull and virtual model was 0.15 ± 0.11 mm, between the virtual and printed models was 0.15 ± 0.12 mm, and between the skull and printed models was 0.24 ± 0.21 mm. Using the optical scanner and specialized inspection software for measurements of accuracy of the created parts is recommended, as it allows one not only to measure 2-dimensional distances between anatomical points but also to perform more clinically suitable comparisons of whole surfaces. However, it requires specialized software and a very accurate scanner in order to be useful. Threshold-based, manually corrected segmentation of orbital walls performed with 3D Slicer software is accurate enough to be used for creating a virtual model of the orbit. The accuracy of the paper-based Mcor Matrix 300 3D printer is comparable to those of other commonly used 3-dimensional printers and allows one to create precise anatomical models for clinical use. The method of dividing the model into smaller parts and sticking them together seems to be quite accurate, although we recommend it only for creating small, solid models with as few parts as possible to minimize shift associated with gluing. |
Validation of a Novel Geometric Coordination Registration using Manual and Semi-automatic Registration in Cone-beam Computed Tomogram
|
Publication: Electronic Imaging, Image Processing: Machine Vision Applications IX, 2016 Feb; pp. 1-6(6). | PDF Authors: Lam W, Luk H, Ngan H, Hsung R, Goto T, Pow E. Institution: Faculty of Dentistry, The University of Hong Kong, Hong Kong, China. Background/Purpose: Cartesian coordinates define on a physical cubic corner (CC) with the corner tip as the origin and three corresponding line angles as (x, y, z)-axes. In its image (virtual) domains such as these obtained by cone-beam computed tomography (CBCT) and optical surface scanning, a single coordinate can then be registered based on the CC. The advantage of using a CC in registration is simple and accurate physical coordinate measurement. The accuracy of image-to-physical (IP) and image-to-image (II) transformations, measured by target registration error (TRE), can then be validated by comparing coordinates of target points in the virtual domains to that of the physical control. For the CBCT, the registration may be performed manually using a surgical planning software SimPlant Pro (manual registration (MR)) or semi-automatically using MeshLab and 3D Slicer (semiautomatic registration (SR)) matching the virtual display axes to the corresponding (x-y-z)-axes. This study aims to validate the use of CC as a surgical stereotactic marker by measuring TRE in MR and SR respectively. Mean TRE is 0.56 +/- 0.24 mm for MR and 0.39 +/- 0.21 mm for SR. The SR results in a more accurate registration than the MR and point-based registration with 20 fiducial points. TRE of the MR is less than 1.0 mm and still acceptable clinically. |
 Coordinate measurement in 3D Slicer (tangential linear distances to axes). |
Multi Texture Analysis of Colorectal Cancer Continuum using Multispectral Imagery
|
Publication: PLoS One. 2016 Feb 22;11(2):e0149893. PMID: 26901134 | PDF Authors: Chaddad A, Desrosiers C, Bouridane A, Toews M, Hassan L, Tanougast C. Institution: Laboratory for Imagery, Vision and Artificial Intelligence, Ecole de Technologie Superieure, Montreal, Quebec, Canada. Background/Purpose: This paper proposes to characterize the continuum of colorectal cancer (CRC) using multiple texture features extracted from multispectral optical microscopy images. Three types of pathological tissues (PT) are considered: benign hyperplasia, intraepithelial neoplasia and carcinoma. MATERIALS AND Methods: In the proposed approach, the region of interest containing PT is first extracted from multispectral images using active contour segmentation. This region is then encoded using texture features based on the Laplacian-of-Gaussian (LoG) filter, discrete wavelets (DW) and gray level co-occurrence matrices (GLCM). To assess the significance of textural differences between PT types, a statistical analysis based on the Kruskal-Wallis test is performed. The usefulness of texture features is then evaluated quantitatively in terms of their ability to predict PT types using various classifier models. Results: Preliminary results show significant texture differences between PT types, for all texture features (p-value < 0.01). Individually, GLCM texture features outperform LoG and DW features in terms of PT type prediction. However, a higher performance can be achieved by combining all texture features, resulting in a mean classification accuracy of 98.92%, sensitivity of 98.12%, and specificity of 99.67%. Conclusions: These results demonstrate the efficiency and effectiveness of combining multiple texture features for characterizing the continuum of CRC and discriminating between pathological tissues in multispectral images. |
 Examples of ground truth segmentation. (a) Original image. (b) Segmented image. (c) Labeled image. Labeled area in (c) corresponds to the ROI used for texture feature extraction.Ground truth segmentations, one segmentation per sample, were obtained manually using 3D Slicer. |
Cranial Anatomy and Palaeoneurology of the Archosaur Riojasuchus tenuisceps from the Los Colorados Formation, La Rioja, Argentina
|
Publication: PLoS One. 2016 Feb 5;11(2):e0148575. PMID: 26849433 | PDF Authors: von Baczko MB, Desojo JB. Institution: Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), Ciudad Autónoma de Buenos Aires, Buenos Aires, Argentina. Background/Purpose: Riojasuchus tenuisceps Bonaparte 1967 is currently known from four specimens, including two complete skulls, collected in the late 1960s from the upper levels of the Los Colorados Formation (Late Triassic), La Rioja, Argentina. Computed tomography (CT) scans of the skulls of the holotype and a referred specimen of Riojasuchus tenuisceps and the repreparation of the latter allows recognition of new features for a detailed analysis of its cranial anatomy and its comparison with a wide variety of other archosauriform taxa. The diagnosis of Riojasuchus tenuisceps is emended and two autapomorphies are identified on the skull: (1) a deep antorbital fossa with its anterior and ventral edges almost coinciding with the same edges of the maxilla itself and (2) a suborbital fenestra equal in size to the palatine-pterygoid fenestra. Also, the first digital 3D reconstruction of the encephalon of Riojasuchus tenuisceps was carried out to study its neuroanatomy, showing a shape and cranial nerve disposition consistent to that of other pseudosuchians. |
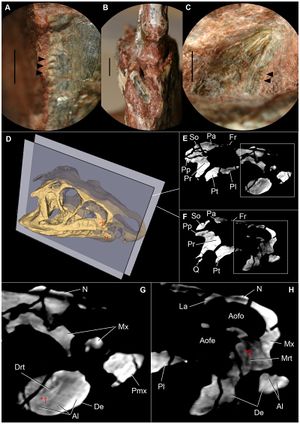 Details of dentition of Riojasuchus tenuisceps. (A) lateral detail of denticles on distal margin of maxillary tooth (PVL 3828); (B) anterior view of first dentary tooth (PVL 3827) broken at its base; (C) medial view of posterior dentary tooth (PVL 3828) with denticles on distal margin; (D) 3D reconstruction of the skull of PVL 3827 indicating selected slices; (E-F) selected slices of PVL 3827; (G) detail of slide E indicating a maxillary replacement tooth (Mrt) erupting; (H) detail of slide F pointing out a dentary replancement tooth (Drt); *1 and *2 indicate the position of each replacement tooth on the skull. Arrowheads point at denticles. Abbreviations: Al, alveoli; Aofe, antorbital fenestra; Aofo, antorbital fossa; De, dentary, Drt, dentary replacement tooth; Fr, frontal; N, nasal; Mrt, maxillary replacement tooth; Mx, maxilla; Pa, parietal; Pl, palatine; Pmx, premaxilla; Pp, paroccipital process; Pr, prootic; Pt, pterygoid; Q, quadrate; So, supraoccipital. Scale bar: 2mm. For the analysis of the CT images and 3D reconstruction, we used the open source software 3D Slicer v4.1.1. |
Diffusion Tensor Imaging Assessment of Microstructural Brainstem Integrity in Chiari Malformation Type I.
|
Publication: J Neurosurg. 2016 Feb 5:1-8. PMID: 26848913 | PDF Authors: Krishna V, Sammartino F, Yee P, Mikulis D, Walker M, Elias G, Hodaie M. Institution: Department of Neurosurgery, Ohio State University, Columbus, Ohio. Background/Purpose: OBJECTIVE The diagnosis of Chiari malformation Type I (CM-I) is primarily based on the degree of cerebellar tonsillar herniation even though it does not always correlate with symptoms. Neurological dysfunction in CM-I presumably results from brainstem compression. With the premise that conventional MRI does not reveal brain microstructural changes, this study examined both structural and microstructural neuroimaging metrics to distinguish patients with CM-I from age- and sex-matched healthy control subjects. METHODS Eight patients with CM-I and 16 controls were analyzed. Image postprocessing involved coregistration of anatomical T1-weighted with diffusion tensor images using 3D Slicer software. The structural parameters included volumes of the posterior fossa, fourth ventricle, and tentorial angle. Fractional anisotropy (FA) was calculated separately in the anterior and posterior compartments of the lower brainstem. RESULTS The mean age of patients in the CM-I cohort was 42.6 ± 10.4 years with mean tonsillar herniation of 12 mm (SD 0.7 mm). There were no significant differences in the posterior fossa volume (p = 0.06) or fourth ventricular volume between the 2 groups (p = 0.11). However, the FA in the anterior brainstem compartment was significantly higher in patients with CM-I preoperatively (p = 0.001). The FA values normalized after Chiari decompression except for persistently elevated FA in the posterior brainstem compartment in patients with CM-I and syrinx. CONCLUSIONS In this case-control study, microstructural alterations appear to be reliably associated with the diagnosis of CM-I, with a significantly elevated FA in the lower brainstem in patients with CM-I compared with controls. More importantly, the FA values normalized after decompressive surgery. These findings should be validated in future studies to determine the significance of diffusion tensor imaging-based assessment of brainstem microstructural integrity as an adjunct to the clinical assessment in patients with CM-I. |
Large Area 3-D Optical Coherence Tomography Imaging of Lumpectomy Specimens for Radiation Treatment Planning
|
Publication: Proc. SPIE 9689 2016 Feb; Photonic Therapeutics and Diagnostics XII, 968946. Authors: Wang C, Kim L, Barnard N, Khan A, Pierce MC. Institution: Rutgers, The State University of New Jersey NJ, USA. Background/Purpose: Our long term goal is to develop a high-resolution imaging method for comprehensive assessment of tissue removed during lumpectomy procedures. By identifying regions of high-grade disease within the excised specimen, we aim to develop patient-specific post-operative radiation treatment regimens. We have assembled a benchtop spectral-domain optical coherence tomography (SD-OCT) system with 1320 nm center wavelength. Automated beam scanning enables “sub-volumes” spanning 5 mm x 5 mm x 2 mm (500 A-lines x 500 B-scans x 2 mm in depth) to be collected in under 15 seconds. A motorized sample positioning stage enables multiple sub-volumes to be acquired across an entire tissue specimen. Sub-volumes are rendered from individual B-scans in 3D Slicer software and en face (XY) images are extracted at specific depths. These images are then tiled together using MosaicJ software to produce a large area en face view (up to 40 mm x 25 mm). After OCT imaging, specimens were sectioned and stained with HE, allowing comparison between OCT image features and disease markers on histopathology. This manuscript describes the technical aspects of image acquisition and reconstruction, and reports initial qualitative comparison between large area en face OCT images and HE stained tissue sections. Future goals include developing image reconstruction algorithms for mapping an entire sample, and registering OCT image volumes with clinical CT and MRI images for post-operative treatment planning. |
Development and Evaluation of an Open-Source 3D Virtual Simulator with Integrated Motion-Tracking as a Teaching Tool for Pedicle Screw Insertion
|
Publication: Orthopaedic Proceedings 2016 Feb; 98:Supp.5-16. Authors: Mclachlin S, Polley B, Beig M, Larouche J, Whyne C. Institution: Sunnybrook Research Institute (SRI), University of Toronto, Canada. Background/Purpose: Simulation is an effective adjunct to the traditional surgical curriculum, though access to these technologies is often limited and costly. The objectives of this work were to develop a freely accessible virtual pedicle screw simulator and to improve the clinical authenticity of the simulator through integration of low-cost motion tracking. The open-source medical imaging and visualization software, 3D Slicer, was used as the development platform for the virtual simulation. 3D Slicer contains many features for quickly rendering and transforming 3D models of the bony spine anatomy from patient-specific CT scans. A step-wise pedicle screw insertion workflow module was developed which emulated typical pre-operative planning steps. This included taking anatomic measurements, identifying insertion landmarks, and choosing appropriate screw sizes. Monitoring of the surgeon's simulated tool was assessed with a low-cost motion tracking sensor in real-time. This allowed for the surgeon's physical motions to be tracked as they defined the virtual screw's insertion point and trajectory on the rendered anatomy. Screw insertion was evaluated based on bone density contact and cortical breaches. Initial surgeon feedback of the virtual simulator with integrated motion tracking was positive, with no noticeable lag and high accuracy between the real-world and virtual environments. The software yields high fidelity 3D visualization of the complex geometry and the tracking enabled coordination of motion to small changes in both translational and angular positioning. Future work will evaluate the benefit of this simulation platform with use over the course of resident spine rotations to improve planning and surgical competency. |
Effect of Decompressive Craniectomy on Perihematomal Edema in Patients with Intracerebral Hemorrhage
|
Publication: PLoS One. 2016 Feb 12;11(2):e0149169. PMID: 26872068 | PDF Authors: Fung C, Murek M, Klinger-Gratz PP, Fiechter M, Z'Graggen WJ, Gautschi OP, El-Koussy M, Gralla J, Schaller K, Zbinden M, Arnold M, Fischer U, Mattle HP, Raabe A, Beck J. Institution: Department of Neurosurgery, University Hospital Bern, Bern, Switzerland. Background/Purpose: BACKGROUND: Perihematomal edema contributes to secondary brain injury in the course of intracerebral hemorrhage. The effect of decompressive surgery on perihematomal edema after intracerebral hemorrhage is unknown. This study analyzed the course of PHE in patients who were or were not treated with decompressive craniectomy. Methods: More than 100 computed tomography images from our published cohort of 25 patients were evaluated retrospectively at two university hospitals in Switzerland. Computed tomography scans covered the time from admission until day 100. Eleven patients were treated by decompressive craniectomy and 14 were treated conservatively. Absolute edema and hematoma volumes were assessed using 3-dimensional volumetric measurements. Relative edema volumes were calculated based on maximal hematoma volume. Results: Absolute perihematomal edema increased from 42.9 ml to 125.6 ml (192.8%) after 21 days in the decompressive craniectomy group, versus 50.4 ml to 67.2 ml (33.3%) in the control group (Δ at day 21 = 58.4 ml, p = 0.031). Peak edema developed on days 25 and 35 in patients with decompressive craniectomy and controls respectively, and it took about 60 days for the edema to decline to baseline in both groups. Eight patients (73%) in the decompressive craniectomy group and 6 patients (43%) in the control group had a good outcome (modified Rankin Scale score 0 to 4) at 6 months (P = 0.23). Conclusions: Decompressive craniectomy is associated with a significant increase in perihematomal edema compared to patients who have been treated conservatively. Perihematomal edema itself lasts about 60 days if it is not treated, but decompressive craniectomy ameliorates the mass effect exerted by the intracerebral hemorrhage plus the perihematomal edema, as reflected by the reduced midline shift. |
Current Smoking Status is Associated with Lower Quantitative CT Measures of Emphysema and Gas Trapping
|
Publication: J Thorac Imaging. 2016 Jan;31(1):29-36. PMID: 26429588| PDF Authors: Zach JA, Williams A, Jou SS, Yagihashi K, Everett D, Hokanson JE, Stinson D, Lynch DA, COPDGene Investigators. Institution: Divisions of Radiology, Biostatistics and Bioinformatics, National Jewish Health, Denver, CO, USA. Background/Purpose: The purposes of this study were to evaluate the effect of smoking status on quantitative computed tomography CT measures of low-attenuation areas (LAAs) on inspiratory and expiratory CT and to provide a method of adjusting for this effect. Materials and Methods: A total of 6762 current and former smokers underwent spirometry and volumetric inspiratory and expiratory CT. Quantitative CT analysis was completed using open-source 3D Slicer software. Funding:
|
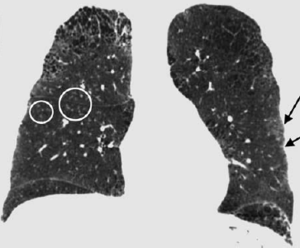 Examples of CN on CT. Coronal CT image of a GOLD 1 subject with moderately extensive visual extent of emphysema. However, the quantitative emphysema score was only 5.1%. The emphysema may have been masked on quantitative assessment by the presence of centrilobular nodules (circled) and patchy ground-glass abnormality (arrows). |
A Proposed Method for Accurate 3D Analysis of Cochlear Implant Migration using Fusion of Cone Beam CT
|
Publication: Front Surg. 2016 Jan 25;3:2. PMID: 26901134 | PDF Authors: Dees G, van Hoof M, Stokroos R. Institution: Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center, Maastricht, The Netherlands. Background/Purpose: The goal of this investigation was to compare fusion of sequential cone beam computerized tomography (CT) volumes to the gold standard (fiducial registration) in order to be able to analyze clinical cochlear implant (CI) migration with high accuracy in three dimensions. MATERIALS AND Methods: Paired cone beam CT volumes were performed on five human cadaver temporal bones and one human subject. These volumes were fused using 3D Slicer 4 and BRAINSFit software. Using a gold standard fiducial technique, the accuracy, robustness, and performance time of the fusion process were assessed. Results: This proposed fusion protocol achieves a subvoxel median Euclidean distance of 0.05 mm in human cadaver temporal bones and 0.16 mm (mean) when applied to the described in vivo human synthetic data set in over 95% of all fusions. Performance times are <2 min. Conclusion: Here, a new and validated method based on existing techniques is described, which could be used to accurately quantify migration of CI electrodes. |
 Human cadaver temporal bone. Axial fused images of a human cadaver temporal bone. (A) No registration. (B) Fiducial registration. (C) BRAINSFit registration. Notice the discernible overlapping borders when no registration is applied. The arrows indicate a fiducial marker. Image analysis, registration, and visualization are performed using the open source 3D Slicer 4 package, including the BRAINS software package. |
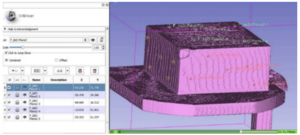
Boolean Combinations of Implicit Functions for Model Clipping in Computer-Assisted Surgical Planning
|
Publication: PLoS One. 2016 Jan 11;11(1):e0145987. PMID: 26751685 | PDF Authors: Zhan Q, Chen X. Institution: School of Mechanical Engineering, Shanghai Jiao Tong University, Shanghai, China. Background/Purpose: This paper proposes an interactive method of model clipping for computer-assisted surgical planning. The model is separated by a data filter that is defined by the implicit function of the clipping path. Being interactive to surgeons, the clipping path that is composed of the plane widgets can be manually repositioned along the desirable presurgical path, which means that surgeons can produce any accurate shape of the clipped model. The implicit function is acquired through a recursive algorithm based on the Boolean combinations (including Boolean union and Boolean intersection) of a series of plane widgets' implicit functions. The algorithm is evaluated as highly efficient because the best time performance of the algorithm is linear, which applies to most of the cases in the computer-assisted surgical planning. Based on the above stated algorithm, a user-friendly module named SmartModelClip is developed on the basis of 3D Slicer platform and VTK. A number of arbitrary clipping paths have been tested. Experimental results of presurgical planning for three types of Le Fort fractures and for tumor removal demonstrate the high reliability and efficiency of our recursive algorithm and robustness of the module. Funding:
|
 A snapshot of the module SmartModelClip in 3D Slicer. On the left is the operator command view that users can create and manipulate clipping path and thickness plane(i.e., they can create, hide and delete plane widgets). Users can also reverse the directions of the axes of the both clipping path and thickness plane widget. On the right is the scene that users can interact with the clipping path. They can specify the fiducial points that position the clipping path and modify the boundary of the clipping path by dragging the handles to obtain the desirable clipping path. |
Three-Dimensional Visualization of the Distribution of Melanin-Concentrating Hormone Producing Neurons in the Mouse Hypothalamus
|
Publication: J Chem Neuroanat. 2016 Jan;71:20-5. PMID: 26686291 Authors: Reinitz LZ, Szőke B, Várkonyi EÉ, Sótonyi P, Jancsik V. Institution: Faculty of Veterinary Science, Department of Anatomy and Histology, Szent István University, Budapest, Hungary. Background/Purpose: We present here a new procedure to represent the 3D distribution of neuronal cell bodies within the brain, using exclusively softwares free for research purposes. Our technique is based on digitalized photos of brain slices processed by immunohistochemical technique, and the 3D Slicer software. The technique presented enables transposition of immunohistochemical or in situ hybridization data to the stereotaxic mouse brain atlas (e.g. Paxinos, G., Franklin, K.B.J., 2001. The Mouse Brain in Stereotaxic Coordinates. second ed. Academic Press, San Diego). By exporting the finalized models into a popular 3D design software (3DS Max) arbitrary environment and motion simulation can be created to improve the visual understanding of the area studied. Application of this technique provides the possibility to store, analyze and compare data - e.g. on the hypothalamic neuropeptides - across experimental techniques and laboratories. The method is exemplified by visualizing the distribution of immunohistochemically identified melanin-concetrating hormone (MCH) containing perikarya within the mouse hypothalamus. |
In Vivo Visualization of the Facial Nerve in Patients with Acoustic Neuroma using Diffusion Tensor Imaging-Based Fiber Tracking
|
Publication: J Neurosurg. 2016 Jan 1:1-8. PMID: 26722859 | PDF Authors: Song F, Hou Y, Sun G, Chen X, Xu B, Huang JH, Zhang J. Institution: Department of Neurosurgery, People's Liberation Army General Hospital, Beijing, China. Background/Purpose: OBJECTIVE Preoperative determination of the facial nerve (FN) course is essential to preserving its function. Neither regular preoperative imaging examination nor intraoperative electrophysiological monitoring is able to determine the exact position of the FN. The diffusion tensor imaging-based fiber tracking (DTI-FT) technique has been widely used for the preoperative noninvasive visualization of the neural fasciculus in the white matter of brain. However, further studies are required to establish its role in the preoperative visualization of the FN in acoustic neuroma surgery. The object of this study is to evaluate the feasibility of using DTI-FT to visualize the FN. Methods Data from 15 patients with acoustic neuromas were collected using 3-T MRI. The visualized FN course and its position relative to the tumors were determined using DTI-FT with 3D Slicer software. The preoperative visualization results of FN tracking were verified using microscopic observation and electrophysiological monitoring during microsurgery. Results Preoperative visualization of the FN using DTI-FT was observed in 93.3% of the patients. However, in 92.9% of the patients, the FN visualization results were consistent with the actual surgery. CONCLUSIONS DTI-FT, in combination with intraoperative FN electrophysiological monitoring, demonstrated improved FN preservation in patients with acoustic neuroma. FN visualization mainly included the facial-vestibular nerve complex of the FN and vestibular nerve. |
Optic Nerve Tractography Prediction of Visual Deficit in Pituitary Macroadenoma
|
Publication: J Neurol Surg B 2016; 77-P060. Authors: Au K, Zadeh G. Institution: Toronto Western Hospital, University Health Network, Toronto, Ontario, Canada. Background/Purpose: The presentation of nonfunctioning pituitary adenomas is frequently delayed due to the absence of a hormonal syndrome, and tumors have often attained a large size by the time of diagnosis. Pronounced compression of the optic chiasm can be evident on imaging, and may be associated with deficits in visual acuity and visual fields. However, the severity of visual symptoms varies widely among patients, and some retain intact visual function despite dramatic optic chiasm deformation. MRI features including optic nerve atrophy and vertical tumor extension, and other modalities such as optical coherence tomography, have not been found to reliably predict visual deficits or recovery of visual function following pituitary tumor resection. Diffusion tensor imaging (DTI) utilizes the principle of anisotropic water diffusion along white matter fibers to reconstruct fiber tracts. Tractography has long been used to delineate large fiber bundles in glioma surgery, but the feasibility of tracking small fiber bundles including cranial nerves has also recently been demonstrated. The optic nerves, chiasm, optic tracts and optic radiations can be displayed to a high degree of detail using DTI. Since processes such as inflammation and demyelination affect water anisotropy, DTI parameters can detect pathologic changes in axonal properties. Patients with a new diagnosis of pituitary adenoma causing compression of the optic chiasm undergo neuro-opthalmologic evaluation including assessment of visual acuity and Humphrey visual field testing. Thin-slice imaging of the sellar region including T1-weighted anatomic imaging and diffusion-weighted imaging (DWI) scans are obtained on 3T MRI, and processed using 3D Slicer software. Neuro-opthalmologic and imaging evaluation are repeated post-operatively in patients who undergo surgical resection of the pituitary tumor. DTI parameters including fractional anisotropy, radial diffusivity and axial diffusivity are measured and correlated to visual findings. The ability to reliably correlate non-invasive imaging with visual function in the setting of optic chiasm compression may allow for accurate identification of patients who will develop visual deficits, and who therefore require more urgent surgical intervention. Such imaging may also be valuable in predicting recovery of visual function following decompressive surgery. |