Difference between revisions of "Main Page/SlicerCommunity/2019"
(→2019) |
|||
| Line 2: | Line 2: | ||
=2019= | =2019= | ||
| − | ==Unique | + | ==Unique Metasomal Musculature in Sweat Bees (Hymenoptera, Apoidea, Halictidae) Revealed by Micro-CT Scanning== |
{|width="100%" | {|width="100%" | ||
Revision as of 12:30, 2 April 2019
Home < Main Page < SlicerCommunity < 2019Go to 2022 :: 2021 :: 2020 :: 2019 :: 2018 :: 2017 :: 2016 :: 2015 :: 2014-2011 :: 2010-2000
The community that relies on 3D Slicer is large and active: (numbers below updated on December 1st, 2023)
- 1,467,466+ downloads in the last 11 years (269,677 in 2023, 206,541 in 2022)
- over 17.900+ literature search results on Google Scholar
- 2,147+ papers on PubMed citing the Slicer platform paper
- Fedorov A., Beichel R., Kalpathy-Cramer J., Finet J., Fillion-Robin J-C., Pujol S., Bauer C., Jennings D., Fennessy F.M., Sonka M., Buatti J., Aylward S.R., Miller J.V., Pieper S., Kikinis R. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magnetic Resonance Imaging. 2012 Nov;30(9):1323-41. PMID: 22770690. PMCID: PMC3466397.
- 39 events in open source hackathon series continuously running since 2005 with 3260 total participants
- Slicer Forum with +8,138 subscribers has approximately 275 posts every week
The following is a sample of the research performed using 3D Slicer outside of the group that develops it. in 2019
We monitor PubMed and related databases to update these lists, but if you know of other research related to the Slicer community that should be included here please email: marianna (at) bwh.harvard.edu.
Contents
- 1 2019
- 1.1 Unique Metasomal Musculature in Sweat Bees (Hymenoptera, Apoidea, Halictidae) Revealed by Micro-CT Scanning
- 1.2 3D Reconstruction of MR-Visible Fe3O4-Mesh Implants: Pelvic Mesh Measurement Techniques and Preliminary Findings
- 1.3 A Complete Workflow for Utilizing Monte Carlo Toolkits in Clinical Cases for a Double-Scattering Proton Therapy System
- 1.4 Morphological Analysis of Sigmoid Sinus Anatomy: Clinical Applications to Neurotological Surgery
2019
Unique Metasomal Musculature in Sweat Bees (Hymenoptera, Apoidea, Halictidae) Revealed by Micro-CT Scanning
|
Publication: American Museum Novitates | PDF Authors: Herhold, Hollister W.; Davis, Steven R., 1983-; Smith, Corey Shepard.; Engel, Michael S.; Grimaldi, David A. Institution: American Museum of Natural History, New York, NY Abstract: Bees of the family Halictidae (Apoidea: Anthophila) have three pairs of thick, bundled muscles that are circular to subcircular in cross section within the first metasomal segment, as revealed by micro-CT scanning of 16 species in 15 genera of five bee families. In nonhalictids and the basal halictid subfamily Rophitinae, these muscles are planar (flat and sheetlike), typically lying between the anterior air sacs and abdominal wall. In Nomiinae and Halictinae, these muscles, especially the dorsal-ventral pair, bulge into air-sac space, partly enveloped by air-sac membrane. A possible function may be to facilitate metasomal compression and contraction, and thus air flow. The bundled shape of these derived halictid muscles is similar to that of flight muscles, but further data is needed to determine if they are fibrillar, which would suggest a completely different function. |
3D Reconstruction of MR-Visible Fe3O4-Mesh Implants: Pelvic Mesh Measurement Techniques and Preliminary Findings
|
Publication: Neurourol Urodyn. 2019 Jan;38(1):369-78. PMID: 30387537 Authors: Brocker KA, Mokry T, Alt CD, Kauczor HU, Lenz F, Sohn C, DeLancey JO, Chen L. Institution: Department of Obstetrics and Gynecology, Medical School, University of Heidelberg, Heidelberg, Germany. Abstract: AIMS: To develop MR-based measurement technique to evaluate the postoperative dimension and location of implanted magnetic resonance (MR)-visible meshes. METHODS: This technique development study reports findings of six patients (A-F) with cystoceles treated with anterior vaginal MR-visible Fe3O4 -polypropylene implants. Implanted meshes were reconstructed from 3 months and/or 1 year postsurgical MR-images using 3D Slicer. Measurements including mesh length, distance to the ischial spines, pudendal, and obturator neurovascular bundles and urethra were obtained using software Rhino® and a custom Matlab® program. The range of implanted mesh length and their placements were reported and compared with mesh design and implantation recommendations. With the anterior/posterior-mesh-segment-ratio mesh shrinkage localization was evaluated. RESULTS: Examinations were possible for patients A-D 3 months and for A, C, E, and F 1 year postsurgical. The mesh was at least 40% shorter in all patients 3 months and/or 1 year postoperatively. A, B showed shrinkage in the anterior segment, D, E in the posterior segment (Patients C, F not applicable due to intraoperative mesh trimming). Patient E presented pain in the area of mesh shrinkage. In Patient C posterior mesh fixations were placed in the iliococcygeal muscle rather than sacrospinous ligaments. Arm placement less than 20 mm from the pudendal neurovascular bundles was seen in all cases. The portion of the urethra having mesh underneath it ranged from 19% to 55%. CONCLUSIONS: MRI-based measurement techniques have been developed to quantify implanted mesh location and dimension. Mesh placement variations possibly correlating with postoperative complications can be illustrated. Funding:
|
A Complete Workflow for Utilizing Monte Carlo Toolkits in Clinical Cases for a Double-Scattering Proton Therapy System
|
Publication: J Appl Clin Med Phys. 2019 Jan;20(1):23-30. PMID: 30426669 | PDF Authors: Muller L, Prusator M, Ahmad S, Chen Y. Institution: Department of Radiation Oncology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Abstract: The methods described in this paper allow end users to utilize Monte Carlo (MC) toolkits for patient-specific dose simulation and perform analysis and plan comparisons for double-scattering proton therapy systems. The authors aim to fill two aspects of this process previously not explicitly published. The first one addresses the modeling of field-specific components in simulation space. Patient-specific compensator and aperture models are exported from treatment planning system and converted to STL format using a combination of software tools including Matlab and Autodesk's Netfabb. They are then loaded into the MC geometry for simulation purpose. The second details a method for easily visualizing and comparing simulated doses with the dose calculated from the treatment planning system. This system is established by utilizing the open source software 3D Slicer. The methodology was demonstrated with a two-field proton treatment plan on the IROC lung phantom. Profiles and two-dimensional (2D) dose planes through the target isocenter were analyzed using our in-house software tools. This present workflow and set of codes can be easily adapted by other groups for their clinical practice. |
Morphological Analysis of Sigmoid Sinus Anatomy: Clinical Applications to Neurotological Surgery
|
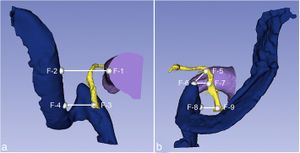
Publication: J Otolaryngol Head Neck Surg. 2019 Jan 11;48(1):2. PMID: 30635049 | PDF Authors: Van Osch K, Allen D, Gare B, Hudson TJ, Ladak H, Agrawal SK. Institution: Schulich School of Medicine & Dentistry, Western University, London, Ontario, Canada. Abstract: OBJECTIVES: The primary objective of this study was to use high-resolution micro-CT images to create accurate three-dimensional (3D) models of several intratemporal structures, and to compare several surgically important dimensions within the temporal bone. The secondary objective was to create a statistical shape model (SSM) of a dominant and non-dominant sigmoid sinus (SS) to provide a template for automated segmentation algorithms. METHODS: A free image processing software, 3D Slicer, was utilized to create three-dimensional reconstructions of the SS, jugular bulb (JB), facial nerve (FN), and external auditory canal (EAC) from micro-CT scans. The models were used to compare several clinically important dimensions between the dominant and non-dominant SS. Anatomic variability of the SS was also analyzed using SSMs generated using the Statismo software framework. RESULTS: Three-dimensional models from 38 temporal bones were generated and analyzed. Right dominance was observed in 74% of the paired SSs. All distances were significantly shorter on the dominant side (p < 0.05), including: EAC - SS (dominant: 13.7 ± 3.4 mm; non-dominant: 15.3 ± 2.7 mm), FN - SS (dominant: 7.2 ± 1.8 mm; non-dominant: 8.1 ± 2.3 mm), 2nd genu FN - superior tip of JB (dominant: 8.7 ± 2.2 mm; non-dominant: 11.2 ± 2.6 mm), horizontal distance between the superior tip of JB - descending FN (dominant: 9.5 ± 2.3 mm; non-dominant: 13.2 ± 3.5 mm), and horizontal distance between the FN at the stylomastoid foramen - JB (dominant: 5.4 ± 2.2 mm; non-dominant: 7.7 ± 2.1). Analysis of the SSMs indicated that SS morphology is most variable at its junction with the transverse sinus, and least variable at the JB. CONCLUSIONS: This is the first known study to investigate the anatomical variation and relationships of the SS using high resolution scans, 3D models and statistical shape analysis. This analysis seeks to guide neurotological surgical approaches and provide a template for automated segmentation and surgical simulation. "In 3D Slicer, nine fiducials (F1 – F9) were placed on the 3D reconstructions of the SS, JB, EAC, and FN to analyze several surgically relevant relationships between these structures." Funding:
|
] |