Difference between revisions of "Main Page/SlicerCommunity/2011-2014"
Tag: 2017 source edit |
Tag: 2017 source edit |
||
| Line 279: | Line 279: | ||
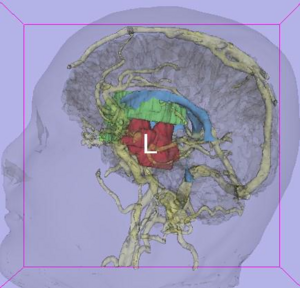
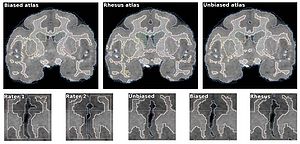
|align="right"|[[image:Hsing-PLosOne2014-fig3.png|thumb|300px| 16 segment model showing the 4 regions evaluated around each pulmonary vein. A) Zoomed and cropped slices labeled by region. B) 3D color-coded display, showing 4 regions about each PV, with explicit labeling for the right inferior and left superior PV. Image analyses were performed using ImageJ (NIH Image, Bethesda, MD) and [http://slicer.org '''3D Slicer'''] (v3.6, NA-MIC, Boston, MA).]] | |align="right"|[[image:Hsing-PLosOne2014-fig3.png|thumb|300px| 16 segment model showing the 4 regions evaluated around each pulmonary vein. A) Zoomed and cropped slices labeled by region. B) 3D color-coded display, showing 4 regions about each PV, with explicit labeling for the right inferior and left superior PV. Image analyses were performed using ImageJ (NIH Image, Bethesda, MD) and [http://slicer.org '''3D Slicer'''] (v3.6, NA-MIC, Boston, MA).]] | ||
| + | |} | ||
| + | |||
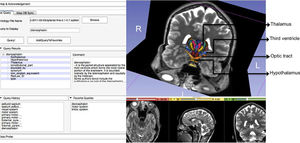
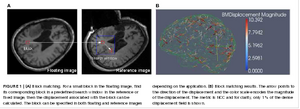
| + | ==Bi-modal Non-rigid Registration of Brain MRI Data with Deconvolution of Joint Statistics== | ||
| + | {|width="100%" | ||
| + | | | ||
| + | '''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/25020093 IEEE Trans Image Process. 2014 Sep;23(9):3999-4009. PMID: 25020093] | ||
| + | |||
| + | '''Authors:''' Pilutti D, Strumia M, Hadjidemetriou S. | ||
| + | |||
| + | '''Institution:''' Department of Radiology Medical Physics, University Medical Center Freiburg, Freiburg, Germany. | ||
| + | |||
| + | '''Background/Purpose:''' A brain MRI protocol typically includes several imaging contrasts that can provide complementary information by highlighting different tissue properties. The acquired data sets often need to be coregistered or placed in a standard anatomic space before any further processing. Current registration methods particularly for multicontrast data are computationally very intensive, their resolution is lower than that of the images, and their distance metric and its optimization can be limiting. In this paper, a novel and effective nonrigid registration method is proposed that is based on the restoration of the joint statistics of pairs of such images. The registration is performed with the deconvolution of the joint statistics with an adaptive Wiener filter. The deconvolved statistics are forced back to the spatial domain to estimate a preliminary registration. The spatial transformation is also regularized with Gaussian spatial smoothing. The registration method has been compared with the B-Splines method implemented in [http://slicer.org '''3D Slicer'''] and with the SyN method implemented in the ANTs toolkit. The validation has been performed with a simulated Shepp–Logan phantom, a BrainWeb phantom, the real data of the NIREP database, and real multicontrast data sets of healthy volunteers. The proposed method has shown improved comparative accuracy as well as analytical efficiency. | ||
|} | |} | ||
Revision as of 17:42, 10 February 2020
Home < Main Page < SlicerCommunity < 2011-2014Go to 2022 :: 2021 :: 2020 :: 2019 :: 2018 :: 2017 :: 2016 :: 2015 :: 2014-2011 :: 2010-2000
The community that relies on 3D Slicer is large and active: (numbers below updated on December 1st, 2023)
- 1,467,466+ downloads in the last 11 years (269,677 in 2023, 206,541 in 2022)
- over 17.900+ literature search results on Google Scholar
- 2,147+ papers on PubMed citing the Slicer platform paper
- Fedorov A., Beichel R., Kalpathy-Cramer J., Finet J., Fillion-Robin J-C., Pujol S., Bauer C., Jennings D., Fennessy F.M., Sonka M., Buatti J., Aylward S.R., Miller J.V., Pieper S., Kikinis R. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magnetic Resonance Imaging. 2012 Nov;30(9):1323-41. PMID: 22770690. PMCID: PMC3466397.
- 39 events in open source hackathon series continuously running since 2005 with 3260 total participants
- Slicer Forum with +8,138 subscribers has approximately 275 posts every week
The following is a sample of the research performed using 3D Slicer outside of the group that develops it. in 2011-2014
We monitor PubMed and related databases to update these lists, but if you know of other research related to the Slicer community that should be included here please email: marianna (at) bwh.harvard.edu.
Contents
- 1 2014
- 1.1 Structural and Functional Bases of Inhibited Temperament
- 1.2 Enhancing Dentate Gyrus Function with Dietary Flavanols Improves Cognition in Older Adults
- 1.3 Femoral and Tibial Insert Downsizing Increases the Laxity Envelope in TKA
- 1.4 MR-Guided Vertebroplasty with Augmented Reality Image Overlay Navigation
- 1.5 Medial Frontal White and Gray Matter Contributions to General Intelligence
- 1.6 Elastography using Multi-Stream GPU: An Application to Online Tracked Ultrasound Elastography, In-Vivo and the da Vinci Surgical System
- 1.7 Texture Descriptors to distinguish Radiation Necrosis from Recurrent Brain Tumors on multi-parametric MRI
- 1.8 Comparison of the Tada Formula with Software Slicer: Precise and Low-Cost Method for Volume Assessment of Intracerebral Hematoma
- 1.9 Human Cardiac Telocytes: 3D Imaging by FIB-SEM Tomography
- 1.10 Segmentation of Metastatic Lesions in Large-scale Registries: Comparison of Expert Manual Segmentation vs. Semi-automated Methods
- 1.11 A New Improved Method for Assessing Brain Deformation after Decompressive Craniectomy
- 1.12 Posterior Cerebral Artery Angle and the Rupture of Basilar Tip Aneurysms
- 1.13 A Nonrigid Registration Method for Correcting Brain Deformation Induced by Tumor Resection
- 1.14 Distribution of Coronoid Fracture Lines by Specific Patterns of Traumatic Elbow Instability
- 1.15 Cardiovascular Magnetic Resonance Imaging of Scar Development Following Pulmonary Vein Isolation: A Prospective Study
- 1.16 Bi-modal Non-rigid Registration of Brain MRI Data with Deconvolution of Joint Statistics
- 1.17 Clinical Testing of an Alternate Method of Inserting Bone-Implanted Fiducial Markers
- 1.18 Three-Dimensional Imaging of HIV-1 Virological Synapses Reveals Membrane Architectures Involved in Virus Transmission
- 1.19 How Action Selection can be Embodied: Intracranial Gamma Band Recording Shows Response Competition during the Eriksen Flankers Test
- 1.20 Airway Wall Thickness is Increased in COPD Patients with Bronchodilator Responsiveness
- 1.21 Compact Robotically Steerable Image-Guided Instrument for Multi-Adjacent-Point (MAP) Targeting
- 1.22 Combined Compared to Dissociated Oral and Intestinal Sucrose Stimuli induce Different Brain Hedonic Processes
- 1.23 Microstructural Changes in the Striatum and Their Impact on Motor and Neuropsychological Performance in Patients with Multiple Sclerosis
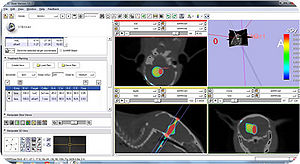
- 1.24 Design and Initial Evaluation of a Treatment Planning Software System for MRI-guided Laser Ablation in the Brain
- 1.25 Orbitofrontal Cortex Volume in Area 11/13 Predicts Reward Devaluation, but not Reversal Learning Performance, in Young and Aged Monkeys
- 1.26 Robust Radiomics Feature Quantification using Semiautomatic Volumetric Segmentation
- 1.27 Tranexamic Acid for Spontaneous Intracerebral Hemorrhage: A Randomized Controlled Pilot Trial (ISRCTN50867461)
- 1.28 On the Design and Development of A Breast Biopsy Navigation System: Path Generation Algorithm and System with Its GUI Evaluation
- 1.29 The Efficacy of Neuroendoscopic Treatment for Middle Cranial Fossa Arachnoid Cysts Assessed by MRI 3D Segmentation and Modeling
- 1.30 Relationship between Interleukin-6 Gene Polymorphism and Hippocampal Volume in Antipsychotic-Naïve Schizophrenia: Evidence for Differential Susceptibility?
- 1.31 Multi-Modal Glioblastoma Segmentation: Man versus Machine
- 1.32 Rapid Amygdala Responses during Trace Fear Conditioning without Awareness
- 1.33 BNST Neurocircuitry in Humans
- 1.34 An Intra-Individual Comparison of MRI, [18F]-FET and [18F]-FLT PET in Patients with High-Grade Gliomas
- 1.35 The Swallow Tail Appearance of the Healthy Nigrosome – A New Accurate Test of Parkinson’s Disease: A Case- Control and Retrospective Cross-Sectional MRI Study at 3T
- 1.36 Clinical and Computed Tomographic Predictors of Chronic Bronchitis in COPD: A Cross Sectional Analysis of the COPDGene Study
- 1.37 Faceted Visualization of Three Dimensional Neuroanatomy by Combining Ontology with Faceted Search
- 1.38 An ITK Implementation of a Physics-based Non-rigid Registration Method for Brain Deformation in Image-guided Neurosurgery
- 1.39 Morphological Parameters Associated with Ruptured Posterior Communicating Aneurysms
- 1.40 Computational Modelling of Emboli Travel Trajectories in Cerebral Arteries: Influence of Microembolic Particle Size and Density
- 1.41 Adaptive Distance Metric Learning for Diffusion Tensor Image Segmentation
- 1.42 Multiple White Matter Volume Reductions in Patients with Panic Disorder: Relationships between Orbitofrontal Gyrus Volume and Symptom Severity and Social Dysfunction
- 1.43 Using Stress MRI to Analyze the 3D Changes in Apical Ligament Geometry from Rest to Maximal Valsalva: A Pilot Study
- 1.44 Scanning Fast and Slow: Current Limitations of 3 Tesla Functional MRI and Future Potential
- 1.45 Molecular Drivers and Cortical Spread of Lateral Entorhinal Cortex Dysfunction in Preclinical Alzheimer’s Disease
- 1.46 Retrosigmoid Implantation of an Active Bone Conduction Stimulator in a Patient with Chronic Otitis Media
- 1.47 Evaluation of Prostate Segmentation Algorithms for MRI: The PROMISE12 Challenge
- 1.48 The Detection and Visualization of Brain Tumors on T2-Weighted MRI Images using Multiparameter Feature Blocks
- 1.49 Spinal Curvature Measurement by Tracked Ultrasound Snapshots
- 1.50 Sequencing Biological and Physical Events Affects Specific Frequency Bands within the Human Premotor Cortex: An Intracerebral EEG Study
- 1.51 Regional 3D Superimposition to assess Temporomandibular Joint Condylar Morphology
- 2 2013
- 2.1 Tracked Ultrasound Snapshots in Percutaneous Pedicle Screw Placement Navigation: A Feasibility Study
- 2.2 Dietary Cholesterol Increases Ventricular Volume and Narrows Cerebrovascular Diameter in a Rabbit Model of Alzheimer's Disease
- 2.3 Rapid and Efficient Localization of Depth Electrodes and Cortical Labeling using Free and Open Source Medical Software in Epilepsy Surgery Candidates
- 2.4 Reduced Habituation in Patients with Schizophrenia
- 2.5 On the Prospect of Patient-specific Biomechanics without Patient-specific Properties of Tissues
- 2.6 Derivation of Neural Stem Cells from Human Adult Peripheral CD34+ Cells for an Autologous Model of Neuroinflammation
- 2.7 Can Transrectal Needle Biopsy be Optimised to Detect Nearly All Prostate Cancer with a Volume of ≥0.5 mL? A Three-dimensional Analysis
- 2.8 Analysis of Morphological Parameters to Differentiate Rupture Status in Anterior Communicating Artery Aneurysms
- 2.9 Anatomic and Morphological Evaluation of the Quadriceps Tendon using 3-Dimensional Magnetic Resonance Imaging Reconstruction
- 2.10 Optical Tractography of the Mouse Heart using Polarization-sensitive Optical Coherence Tomography
- 2.11 Individual Subject Classification of Mixed Dementia from Pure Subcortical Vascular Dementia Based on Subcortical Shape Analysis
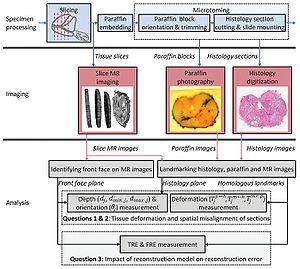
- 2.12 3D Prostate Histology Image Reconstruction: Quantifying the Impact of Tissue Deformation and Histology Section Location
- 2.13 Heat-induced Shrinkage and Shape Preservation of Teeth: A Radiologic Evaluation
- 2.14 Clinical Correlates of Nucleus Accumbens Volume in Drug-naive, Adult Patients with Obsessive-compulsive Disorder
- 2.15 Probing the Regional Distribution of Pulmonary Gas Exchange through Single-breath gas- and Dissolved-phase 129Xe MR Imaging
- 2.16 Resection Probability Maps for Quality Assessment of Glioma Surgery without Brain Location Bias
- 2.17 Consistent Surgeon Evaluations of Three-Dimensional Rendering of PET/CT Scans of the Abdomen of a Patient with a Ductal Pancreatic Mass
- 2.18 Fiber Tract-Driven Topographical Mapping (FTTM) Reveals Microstructural Relevance for Interhemispheric Visuomotor Function in the Aging Brain
- 2.19 Prostate Volumetric Assessment by Magnetic Resonance Imaging and Transrectal Ultrasound: Impact of Variation in Calculated Prostate-Specific Antigen Density on Patient Eligibility for Active Surveillance Program
- 2.20 Quantification and Analysis of 3D Magnetic Resonance Image Brain Tumor
- 2.21 Optic Radiation Fiber Tractography in Glioma Patients Based on High Angular Resolution Diffusion Imaging with Compressed Sensing Compared with Diffusion Tensor Imaging - Initial Experience
- 2.22 Endodontic Access Cavity Simulation in Ceramic Dental Crowns
- 2.23 Augmented Reality Visualization using Image Overlay Technology for MR-Guided Interventions: Cadaveric Bone Biopsy at 1.5 T
- 2.24 How to Detect Amygdala Activity with Magnetoencephalography using Source Imaging
- 2.25 Paired Inspiratory-expiratory Chest CT Scans to Assess for Small Airways Disease in COPD
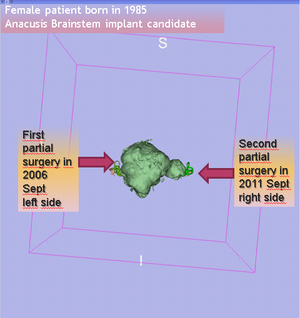
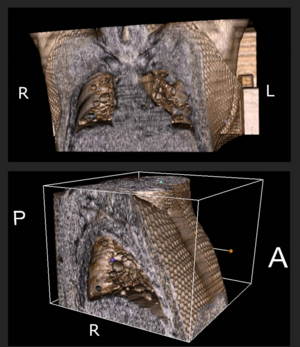
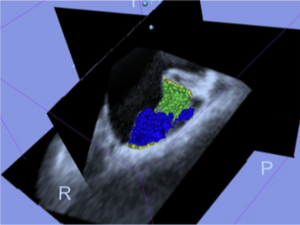
- 2.26 Imaging in Audiology: A Case Report of a Patient with Bilateral Acoustic Neuroma
- 2.27 Computed Tomography Image Processing to Detect the Real Mechanism of Bioprosthesis Failure: Implication for Valve-in-valve Implantation
- 2.28 Preliminary Study on the Clinical Application of Augmented Reality Neuronavigation
- 2.29 Quantitative MRI Analysis of Craniofacial Bone Marrow in Patients with Sickle Cell Disease
- 2.30 Software for MR Image Overlay Guided Needle Insertions: The Clinical Translation Process
- 2.31 Analysis of Conventional Swept-source OCT of Subglottic Stenosis in a Rabbit Model
- 2.32 Three-dimensional Volumetric Rendition of Cannon Ball Pulmonary Metastases by the Use of 3D Slicer, an Open Source Free Software Package
- 2.33 In Vivo Imaging of Dopaminergic Neurotransmission after Transient Focal Ischemia in Rats
- 2.34 MRI Evidence for Altered Venous Drainage and Intracranial Compliance in Mild Traumatic Brain Injury
- 2.35 A Robust Variational Approach for Simultaneous Smoothing and Estimation of DTI
- 2.36 Augmented Reality Visualization Using an Image Overlay System for MR-guided Interventions: Technical Performance of Spine Injection Procedures in Human Cadavers at 1.5 Tesla
- 3 2012
- 3.1 Comparative Evaluation of Mitral Valve Strain by Deformation Tracking in 3D-Echocardiography
- 3.2 Perk Tutor: An Open-source Training Platform for Ultrasound-guided Needle Insertions
- 3.3 Pituitary Adenoma Volumetry with 3D Slicer
- 3.4 Differences in Simple Morphological Variables in Ruptured and Unruptured Middle Cerebral Artery Aneurysms
- 3.5 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network
- 3.6 SlicerRT: Radiation Therapy Research oolkit for 3D Slicer
- 3.7 Developmental Trajectories of Amygdala and Hippocampus from Infancy to Early Adulthood in Healthy Individuals
- 3.8 Extra-Hippocampal Subcortical Limbic Involvement Predicts Episodic Recall Performance in Multiple Sclerosis
- 3.9 Advanced Neuroimaging in Traumatic Brain Injury
- 3.10 Posterior Vaginal Prolapse Shape and Position Changes at Maximal Valsalva Seen in 3D MRI-based Models
- 3.11 Talairach Methodology in the Multimodal Imaging and Robotics Era
- 3.12 SARRP Dose Planning System
- 3.13 Three-dimensional Image Quantification as a New Morphometry Method for Microvascular Tissue Engineering
- 3.14 Prostate: Registration of Digital Histopathologic Images to in Vivo MR Images Acquired by Using Endorectal Receive Coil
- 3.15 A Comparison of the Effect of Age on Levator Ani and Obturator Internus Muscle Cross-sectional Areas and Volumes in Nulliparous Women
- 3.16 A System for Video-based Navigation for Endoscopic Endonasal Skull Base Surgery
- 3.17 Levator Ani Subtended Volume: A Novel Parameter to Evaluate Levator Ani Muscle Laxity in Pelvic Organ Prolapse
- 3.18 Tractography Delineates Microstructural Changes in the Trigeminal Nerve After Focal Radiosurgery for Trigeminal Neuralgia
- 3.19 Square-cut: A Segmentation Algorithm on the Basis of a Rectangle Shape
- 3.20 Anatomical and Functional Correlates of Human Hippocampal Volume Asymmetry
- 3.21 Hippocampal Subregions are Differentially Affected in the Progression to Alzheimer's Disease
- 3.22 Long-term Memory Search Across the Visual Brain
- 3.23 Temporal Course of Cerebrospinal Fluid Dynamics and Amyloid Accumulation in the Aging Rat Brain from Three to Thirty Months
- 3.24 Intact Relational Memory and Normal Hippocampal Structure in the Early Stage of Psychosis
- 3.25 TREK: An Integrated System Architecture for Intraoperative Cone-beam CT-guided Surgery
- 3.26 Cholesterol Increases Ventricular Volume in a Rabbit Model of Alzheimer's Disease
- 4 2011
- 4.1 Atlas-guided Segmentation of Vervet Monkey Brain MRI
- 4.2 Comparison of Acute and Chronic Traumatic Brain Injury Using Semi-automatic Multimodal Segmentation of MR Volumes
- 4.3 3D Slicer
- 4.4 An Open Environment CT-US Fusion for Tissue Segmentation During Interventional Guidance
- 4.5 Mixed Handedness is Associated with Greater Age-related Decline in Volumes of the Hippocampus and Amygdala: The PATH Through Life Study
- 4.6 Multiple Costal Cartilage Graft Reconstruction for the Treatment of a Full-length Laryngotracheal Stenosis after an Inhalation Burn
- 4.7 A Supervised Patch-based Approach for Human Brain Labeling
- 4.8 The Chronic Bronchitic Phenotype of COPD: An Analysis of the COPDGene Study
- 4.9 Airway Inspector: Phenotyping the Lung in COPD
- 4.10 Distance Measurement in Middle Ear Surgery using a Telemanipulator
- 4.11 3D Slicer as a Tool for Interactive Brain Tumor Segmentation
- 4.12 The Effect of Augmented Reality Training on Percutaneous Needle Placement in Spinal Facet Joint Injections
- 4.13 Optimal Transseptal Puncture Location for Robot-assisted Left Atrial Catheter Ablation
- 4.14 Using KinectTM and a Haptic Interface for Implementation of Real-Time Virtual Fixtures
- 4.15 Multiple Indices of Diffusion Identifies White Matter Damage in Mild Cognitive Impairment and Alzheimer's Disease
- 4.16 Assessment of Abdominal Adipose Tissue and Organ Fat Content by Magnetic Resonance Imaging
- 4.17 Subject-specific Musculoskeletal Modeling of the Lower Extremities in Persons with Unilateral Cerebral Palsy
- 4.18 Consistent Neuroanatomical Age-related Volume Differences Across Multiple Samples
- 4.19 Enhancement of a Master-Slave Robotic System for Natural Orifice Transluminal Endoscopic Surgery
- 4.20 Brain Regional Lesion Burden and Impaired Mobility in the Elderly
- 4.21 Three Dimensional in Vivo Modelling of Vestibular Schwannomas and Surrounding Cranial Nerves using Diffusion Imaging Tractography
- 4.22 Intraoperative Real-Time Querying of White Matter Tracts During Frameless Stereotactic Neuronavigation
- 4.23 Three-dimensional Visualization of Subdural Electrodes for Presurgical Planning
- 4.24 Segmentations of MRI Images of the Female Pelvic Floor: A Study of Inter- and Intra-reader Reliability
- 4.25 3D Visualization of Subdural Electrode Shift as Measured at Craniotomy Reopening
- 4.26 Lung Volumes and Emphysema in Smokers with Interstitial Lung Abnormalities
- 4.27 Integration of 3D Anatomical Data Obtained by CT Imaging and 3D Optical Scanning for Computer Aided Implant Surgery
- 4.28 Anisotropy of Transcallosal Motor Fibres Indicates Functional Impairment in Children with Periventricular Leukomalacia
- 4.29 Automatic Lung Segmentation in CT Images with Accurate Handling of the Hilar Region
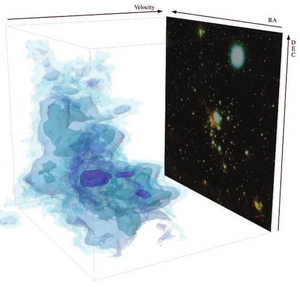
- 4.30 Using 3D Slicer in Astronomy
- 4.31 Brain Morphometry in Autism Spectrum Disorders: A Unified Approach for Structure-specific Statistical Analysis of Neuroimaging Data
- 4.32 Cognitive Profile and Brain Morphological Changes in Obstructive Sleep Apnea
2014
Structural and Functional Bases of Inhibited Temperament
|
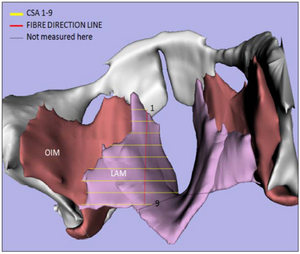
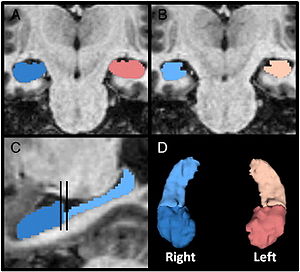
Publication: Soc Cogn Affect Neurosci. 2014 Dec;9(12):2049-58. PMID: 24493850 | PDF Authors: Clauss JA, Seay AL, VanDerKlok RM, Avery SN, Cao A, Cowan RL, Benningfield MM, Blackford JU. Institution: Department of Psychiatry, Vanderbilt University Medical School, Nashville, TN, USA. Background/Purpose: Children born with an inhibited temperament are at heightened risk for developing anxiety, depression and substance use. Inhibited temperament is believed to have a biological basis; however, little is known about the structural brain basis of this vulnerability trait. Structural MRI scans were obtained from 84 (44 inhibited, 40 uninhibited) young adults. Given previous findings of amygdala hyperactivity in inhibited individuals, groups were compared on three measures of amygdala structure. To identify novel substrates of inhibited temperament, a whole brain analysis was performed. Functional activation and connectivity were examined across both groups. Inhibited adults had larger amygdala and caudate volume and larger volume predicted greater activation to neutral faces. In addition, larger amygdala volume predicted greater connectivity with subcortical and higher order visual structures. Larger caudate volume predicted greater connectivity with the basal ganglia, and less connectivity with primary visual and auditory cortex. We propose that larger volume in these salience detection regions may result in increased activation and enhanced connectivity in response to social stimuli. Given the strong link between inhibited temperament and risk for psychiatric illness, novel therapeutics that target these brain regions and related neural circuits have the potential to reduce rates of illness in vulnerable individuals. Funding:
|
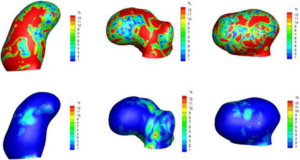
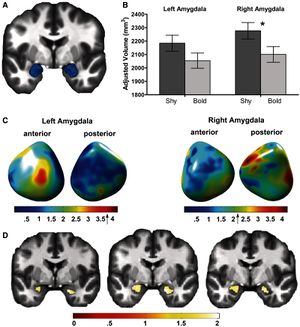 Inhibited adults have larger amygdalae. (A) Average manually traced amygdala displayed in 3D. (B) Overall amygdala volume was greater in the inhibited compared with the uninhibited group in the right amygdala (inhibited: 2277 ± 62 mm3; uninhibited: 2101 ± 59 mm3; P = 0.045). (C) In the inhibited group, shape analysis reveals areas of greater convexity in the left and right amygdala. The peak areas of convexity are shown in red. Group differences in surface amygdala shape are displayed on an average amygdala surface. (D) Inhibited adults had regions of significantly larger gray matter volume in both the left and right amygdalae (P < 0.05 FWE corrected at the cluster level). For the left amygdala, the significant cluster was 442 voxels (35% of 1252 voxels; peak voxel: x = −21, y = −4, z = −16). For the right amygdala, the significant cluster was 402 voxels (33% of 1217 voxels; peak voxel: x = 18, y = −3, z = −22). Areas of significant between-group differences are illustrated on multiple coronal slices of an average brain. Amygdala volume was estimated for each of the subjects in 3D Slicer, Version 3.4. |
Enhancing Dentate Gyrus Function with Dietary Flavanols Improves Cognition in Older Adults
|
Publication: Nat Neurosci. 2014 Dec;17(12):1798-803. PMID: 25344629 | PDF Authors: Brickman AM, Khan UA, Provenzano FA, Yeung LK, Suzuki W, Schroeter H, Wall M, Sloan RP, Small SA. Institution: Taub Institute for Research on Alzheimer's Disease and the Aging Brain, Columbia University, New York, New York, USA. Background/Purpose: The dentate gyrus (DG) is a region in the hippocampal formation whose function declines in association with human aging and is therefore considered to be a possible source of age-related memory decline. Causal evidence is needed, however, to show that DG-associated memory decline in otherwise healthy elders can be improved by interventions that enhance DG function. We addressed this issue by first using a high-resolution variant of functional magnetic resonance imaging (fMRI) to map the precise site of age-related DG dysfunction and to develop a cognitive task whose function localized to this anatomical site. Then, in a controlled randomized trial, we applied these tools to study healthy 50-69-year-old subjects who consumed either a high or low cocoa flavanol-containing diet for 3 months. A high-flavanol intervention was found to enhance DG function, as measured by fMRI and by cognitive testing. Our findings establish that DG dysfunction is a driver of age-related cognitive decline and suggest non-pharmacological means for its amelioration. Funding:
|
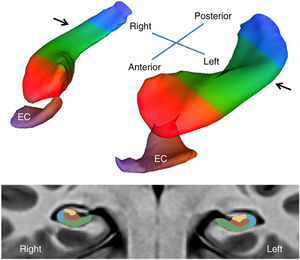 A bilateral map of the hippocampal circuit generated from the high-resolution acquisitions of CBV-fMRI. A three-dimensional rendering of the bilateral hippocampal circuit (top) derived from a group-wise template of multiple axial slices (illustrated at bottom), generated using the native sub-millimeter resolution of CBV maps (Supplementary Video 1). The EC is the main gateway into the hippocampal circuit, and over the long axis (top) the circuit is divided into the head (red), body (green) and tail (blue). In its transverse axis (bottom), taken through the body of the hippocampal long axis (indicated by arrows, top), the hippocampal circuit is divided into the dentate gyrus (brown), CA3 (yellow), CA1 (blue) and subiculum (green). All statistical analyses were performed only in the boundaries of the hippocampal circuit. Corrected maps from individual group comparisons and regressions were then overlaid onto their respective group-wise templates in cross-section using 3D Slicer and also displayed as maximum intensity projections over mesh models of the hippocampal formation. |
Femoral and Tibial Insert Downsizing Increases the Laxity Envelope in TKA
|
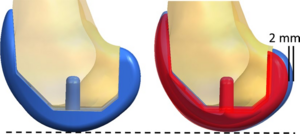
Publication: Knee Surg Sports Traumatol Arthrosc. 2014 Dec;22(12):3003-11. PMID: 25274088 | PDF Authors: Mueller JK, Wentorf FA, Moore RE. Institution: Zimmer, Inc., Warsaw, IN, USA. Background/Purpose: Purpose: This study examines the effect of component downsizing in a modern total knee arthroplasty (TKA) system on the laxity envelope of the knee throughout flexion. Methods: A robotic testing system was utilized to measure laxity envelopes in the implanted knee by in the anterior-posterior (AP), medial-lateral (ML), internal-external (IE) and varus-valgus (VV) directions. Five fresh-frozen cadavers were tested with a modern cruciate retaining TKA implantation, a 1-mm thinner polyethylene insert and a femoral component 2 mm smaller in the AP dimension. Results: The downsized tibial insert was more lax throughout the flexion arc with up to 2.0 mm more laxity in the AP direction at full extension, a 43.8 % increase over the original implantation. A thinner insert consistently increased laxity throughout the arc of flexion in all degrees of freedom. Downsizing the femoral component resulted in 8.5 mm increase in AP laxity at 90°, a 73.9 % increase. In mid-flexion, downsizing the femur produced similar laxity values to the downsized insert in AP, ML, IE and VV directions. Conclusion: Downsizing the TKA components had significant effects on laxity throughout flexion. Downsizing a femoral component 2 mm had an equivalent increase in laxity in mid-flexion as downsizing the tibial insert 1 mm. This study quantifies the importance of choosing the appropriate implant component size, having the appropriate size available and the effect of downsizing. The laxity of the implanted knee contributes to how the implant feels to the patient and ultimately the patient's satisfaction with their new knee. |
|
Publication: Cardiovasc Intervent Radiol. 2014 Dec;37(6):1589-96. PMID: 24722894 Authors: Fritz J, U-Thainual P, Ungi T, Flammang AJ, Kathuria S, Fichtinger G, Iordachita II, Carrino JA. Institution: Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins University School of Medicine, Baltimore, MD, USA. Background/Purpose: To evaluate the feasibility of magnetic resonance imaging (MRI)-guided vertebroplasty at 1.5 Tesla using augmented reality image overlay navigation. Materials and Methods: Twenty-five unilateral vertebroplasties [5 of 25 (20 %) thoracic, 20 of 25 (80 %) lumbar] were prospectively planned in 5 human cadavers. A clinical 1.5-Teslan MRI system was used. An augmented reality image overlay navigation system and 3D Slicer visualization software were used for MRI display, planning, and needle navigation. Intermittent MRI was used to monitor placement of the MRI-compatible vertebroplasty needle. Cement injections (3 ml of polymethylmethacrylate) were performed outside the bore. The cement deposits were assessed on intermediate-weighted MR images. Outcome variables included type of vertebral body access, number of required intermittent MRI control steps, location of final needle tip position, cement deposit location, and vertebroplasty time. Results: All planned procedures (25 of 25, 100 %) were performed. Sixteen of 25 (64 %) transpedicular and 9 of 25 (36 %) parapedicular access routes were used. Six (range 3-9) MRI control steps were required for needle placement. No inadvertent punctures were visualized. Final needle tip position and cement location were adequate in all cases (25 of 25, 100 %) with a target error of the final needle tip position of 6.1 ± 1.9 mm (range 0.3-8.7 mm) and a distance between the planned needle tip position and the center of the cement deposit of 4.3 mm (range 0.8-6.8 mm). Time requirement for one level was 16 (range 11-21) min. Conclusion: MRI-guided vertebroplasty using image overlay navigation is feasible allowing for accurate vertebral body access and cement deposition in cadaveric thoracic and lumbar vertebral bodies. Funding:
|
Medial Frontal White and Gray Matter Contributions to General Intelligence
|
Publication: PLoS One. 2014 Dec 31;9(12):e112691. PMID: 25551572 | PDF Authors: Ohtani T, Nestor PG, Bouix S, Saito Y, Hosokawa T, Kubicki M. Institution: Department of Diagnostic and Interventional Radiology, Centre Hospitalier Universitaire Vaudois (CHUV) and University of Lausanne, Lausanne, Switzerland. Background/Purpose: The medial orbitofrontal cortex (mOFC) and rostral anterior cingulate cortex (rACC) are part of a wider neural network that plays an important role in general intelligence and executive function. We used structural brain imaging to quantify magnetic resonance gray matter volume and diffusion tensor white matter integrity of the mOFC-rACC network in 26 healthy participants who also completed neuropsychological tests of intellectual abilities and executive function. Stochastic tractography, the most effective Diffusion Tensor Imaging method for examining white matter connections between adjacent gray matter regions, was employed to assess the integrity of mOFC-rACC pathways. Fractional anisotropy (FA), which reflects the integrity of white matter connections, was calculated. Results indicated that higher intelligence correlated with greater gray matter volumes for both mOFC and rACC, as well as with increased FA for left posterior mOFC-rACC connectivity. Hierarchical regression analyses revealed that DTI-derived FA of left posterior mOFC-rACC uniquely accounted for 29%-34% of the variance in IQ, in comparison to 11%-16% uniquely explained by gray matter volume of the left rACC. Together, left rACC gray matter volume and white matter connectivity between left posterior mOFC and rACC accounted for up to 50% of the variance in general intelligence. This study is to our knowledge the first to examine white matter connectivity between OFC and ACC, two gray matter regions of interests that are very close in physical proximity, and underscores the important independent contributions of variations in rACC gray matter volume and mOFC-rACC white matter connectivity to individual differences in general intelligence. |
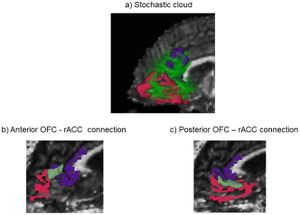 The stochastic cloud connecting the medial orbitofrontal cortex (mOFC) and the rostral anterior cingulate cortex (rACC). The red structure is the mOFC, the purple is the rACC, and the light green is the stochastic cloud connecting the mOFC and rACC. Stochastic tractography (part of Slicer3 software was performed to generate WM connections. |
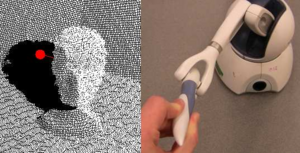
Elastography using Multi-Stream GPU: An Application to Online Tracked Ultrasound Elastography, In-Vivo and the da Vinci Surgical System
|
Publication: PLoS One. 2014 Dec 26;9(12):e115881. PMID: 25541954 | PDF Authors: Deshmukh NP, Kang HJ, Billings SD, Taylor RH, Hager GD, Boctor EM. Institution: Department of Computer Science, Johns Hopkins University, Baltimore, MD, USA. Background/Purpose: A system for real-time ultrasound (US) elastography will advance interventions for the diagnosis and treatment of cancer by advancing methods such as thermal monitoring of tissue ablation. A multi-stream graphics processing unit (GPU) based accelerated normalized cross-correlation (NCC) elastography, with a maximum frame rate of 78 frames per second, is presented in this paper. A study of NCC window size is undertaken to determine the effect on frame rate and the quality of output elastography images. This paper also presents a novel system for Online Tracked Ultrasound Elastography (O-TRuE), which extends prior work on an offline method. By tracking the US probe with an electromagnetic (EM) tracker, the system selects in-plane radio frequency (RF) data frames for generating high quality elastograms. A novel method for evaluating the quality of an elastography output stream is presented, suggesting that O-TRuE generates more stable elastograms than generated by untracked, free-hand palpation. Since EM tracking cannot be used in all systems, an integration of real-time elastography and the da Vinci Surgical System is presented and evaluated for elastography stream quality based on our metric. The da Vinci surgical robot is outfitted with a laparoscopic US probe, and palpation motions are autonomously generated by customized software. It is found that a stable output stream can be achieved, which is affected by both the frequency and amplitude of palpation. The GPU framework is validated using data from in-vivo pig liver ablation; the generated elastography images identify the ablated region, outlined more clearly than in the corresponding B-mode US images.
|
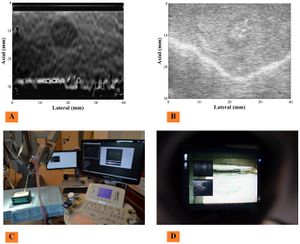 Integration with da Vinci surgical systems. Untracked elastography has been integrated with da Vinci surgical systems using a laparoscopic probe controlled by an arm of the da Vinci surgical robot. (C) Shows the overall setup. (D) Shows the view from surgeon's console of how B-mode (B) and Elastography image (A) appear when overlaid in the console display. The system is highly modular and connected via the OpenIGTLinkMUSiiC API. This grants the ability to connect our system to various open source frontend modules, such as 3D Slicer for advanced visualization of the image stream. |
Texture Descriptors to distinguish Radiation Necrosis from Recurrent Brain Tumors on multi-parametric MRI
|
Publication: Proc SPIE. 2014;9035:90352B. PMID: 24910722 | PDF Authors: Pallavi T, Prateek P, Lisa R, Leo W, Chaitra B, Andrew S, Mark C, Anant M. Institution: Department of Biomedical Engineering, Case Western Reserve University, Cleveland, OH, USA. Background/Purpose: Differentiating radiation necrosis (a radiation induced treatment effect) from recurrent brain tumors (rBT) is currently one of the most clinically challenging problems in care and management of brain tumor (BT) patients. Both radiation necrosis (RN), and rBT exhibit similar morphological appearance on standard MRI making non-invasive diagnosis extremely challenging for clinicians, with surgical intervention being the only course for obtaining definitive "ground truth". Recent studies have reported that the underlying biological pathways defining RN and rBT are fundamentally different. This strongly suggests that there might be phenotypic differences and hence cues on multi-parametric MRI, that can distinguish between the two pathologies. One challenge is that these differences, if they exist, might be too subtle to distinguish by the human observer. In this work, we explore the utility of computer extracted texture descriptors on multi-parametric MRI (MP-MRI) to provide alternate representations of MRI that may be capable of accentuating subtle micro-architectural differences between RN and rBT for primary and metastatic (MET) BT patients. We further explore the utility of texture descriptors in identifying the MRI protocol (from amongst T1-w, T2-w and FLAIR) that best distinguishes RN and rBT across two independent cohorts of primary and MET patients. A set of 119 texture descriptors (co-occurrence matrix homogeneity, neighboring gray-level dependence matrix, multi-scale Gaussian derivatives, Law features, and histogram of gradient orientations (HoG)) for modeling different macro and micro-scale morphologic changes within the treated lesion area for each MRI protocol were extracted. Principal component analysis based variable importance projection (PCA-VIP), a feature selection method previously developed in our group, was employed to identify the importance of every texture descriptor in distinguishing RN and rBT on MP-MRI. PCA-VIP employs regression analysis to provide an importance score to each feature based on their ability to distinguish the two classes (RN/rBT). The top performing features identified via PCA-VIP were employed within a random-forest classifier to differentiate RN from rBT across two cohorts of 20 primary and 22 MET patients. Our results revealed that, (a) HoG features at different orientations were the most important image features for both cohorts, suggesting inherent orientation differences between RN, and rBT, (b) inverse difference moment (capturing local intensity homogeneity), and Laws features (capturing local edges and gradients) were identified as important for both cohorts, and (c) Gd-C T1-w MRI was identified, across the two cohorts, as the best MRI protocol in distinguishing RN/rBT. Funding:
|
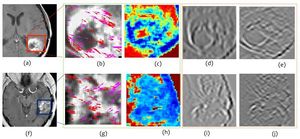 Representative T1-w MR images for rBT (a) and RN (f). Figures 3 (b), (c) and (g), (h) outlined in green, represent top performing features (HoG (red, magenta arrows show top 2 prominent directions), and Laplacian inverse moment (red shows more heterogeneity)) for rBT, RN respectively. Figures 3 (d), (e) and (i), (j), outlined in orange, represent the worst performing features (S5L5 and L5E5 (laplacian) Laws features) for rBT and RN respectively for primary BT patients. |
Comparison of the Tada Formula with Software Slicer: Precise and Low-Cost Method for Volume Assessment of Intracerebral Hematoma
|
Publication: Stroke. 2014 Nov;45(11):3433-5. PMID: 25316277. | PDF Authors: Xu X, Chen X, Zhang J, Zheng Y, Sun G, Yu X, Xu B. Institution: Department of Neurosurgery, People's Liberation Army General Hospital, Beijing, China. Background/Purpose: The Tada (ABC/2) formula has been used widely for volume assessment of intracerebral hematoma. However, the formula is crude for irregularly shaped hematoma. We aimed to compare the accuracy of the ABC/2 formula with open source software 3D Slicer. Methods—Computed tomographic images of 294 patients with spontaneous intracerebral hematoma were collected. Hematoma volumes were assessed with the ABC/2 formula and calculated with software 3D Slicer. Results of these 2 methods were compared with regard to hematoma size and shape. Results—The estimated hematoma volume was 58.41±37.83 cm3 using the ABC/2 formula, compared with 50.38±31.93 cm3 with 3D Slicer (mean percentage deviation, 16.38±9.15%). When allocate patients into groups according to hematoma size, the mean estimation error were 3.24 cm3 (17.72%), 5.85 cm3 (13.72%), and 15.14 cm3 (17.48%) for groups 1, 2, and 3, respectively. When divided by shape, estimation error was 3.33 cm3 (9.76%), 7.19 cm3 (18.37%), and 29.39 cm3 (39.12%) for regular, irregular, and multilobular hematomas. Conclusions—There is significant estimation error using the ABC/2 formula to calculate hematoma volume. Compared with hematoma size, estimation error is more significantly associated with hematoma shape. Funding:
|
Human Cardiac Telocytes: 3D Imaging by FIB-SEM Tomography
|
Publication: J Cell Mol Med. 2014 Nov;18(11):2157-64. PMID: 25327290. | PDF Authors: Cretoiu D, Hummel E, Zimmermann H, Gherghiceanu M, Popescu LM. Institution: Department of Cell Biology and Histology, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania. Background/Purpose: Telocyte (TC) is a newly identified type of cell in the cardiac interstitium (www.telocytes.com). TCs are described by classical transmission electron microscopy as cells with very thin and long telopodes (Tps; cellular prolongations) having podoms (dilations) and podomers (very thin segments). TCs' three-dimensional (3D) morphology is still unknown. Cardiac TCs seem to be particularly involved in long and short distance intercellular signalling and, therefore, their 3D architecture is important for understanding their spatial connections. Using focused ion beam scanning electron microscopy (FIB-SEM) we show, for the first time, the whole ultrastructural anatomy of cardiac TCs. 3D reconstruction of cardiac TCs by FIB-SEM tomography confirms that they have long, narrow but flattened (ribbon-like) telopodes, with humps generated by the podoms. FIB-SEM tomography also confirms the network made by TCs in the cardiac interstitium through adherens junctions. This study provides the first FIB-SEM tomography of a human cell type. |
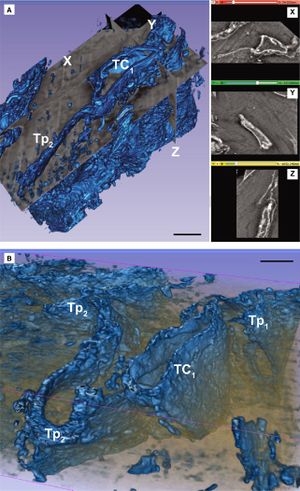 (A and B) Automated segmentation of the stack containing the telocyte TC1 from Figure Figure22 shows that the telopode Tp2 is long (20 μm), narrow (0.2–1 μm) and flat, given a ribbon appearance of the cell. X-Y-Z slice projections from volume could be seen in the right side of A. Scale bars: 2 μm. Images were loaded by batches into 3D Slicer 4.3.1 (64 bit; Harvard Medical School, Boston, MA, USA) and reconstructed using the Volume Rendering module. |
Segmentation of Metastatic Lesions in Large-scale Registries: Comparison of Expert Manual Segmentation vs. Semi-automated Methods
|
Publication: Neuro Oncol. 2014 Nov; 16(Suppl 5): v149. PMC4218376 | PDF Authors: LaMontagne P, Milchencko M, Vélez M, Abraham C, Marcus D, Robinson C, Fouke S. Institution: Washington University School of Medicine, St. Louis, MO, USA. Background/Purpose: To better understand the outcomes after stereotactic radiosurgery (SRS) for brain metastases, we have created a registry that archives MRI studies alongside clinical data in this population. To consider outcomes quantitatively, each metastatic lesion must be segmented to define a 3D volume. In large populations, lesion segmentation is time consuming (and expensive when this requires an experienced Radiation Oncologist or Neurosurgeon) to manually segment each lesion slice by slice. We sought to determine whether semi-automated segmentation using the Growth-Cut toolbox in 3D Slicer (Egger et al. 2013) provides contours equivalent to those created by physicians using manual segmentation methods. A subset of 40 lesions that had undergone manual segmentation for SRS planning were selected to compare with semi-automated segmentation methods. Using the 3D Slicer Growth-Cut toolbox, a novice member of the team partially outlined the lesion tumor and non-tumor tissues. The toolbox then propagated lesion boundaries and created a complete 3D volume. Dice Coefficient (DC), Hausdorff Distance (HD), and Modified Hausdorf Distance (MHD), were used to establish volume similarity between Growth-Cut toolbox output and manual segmentation on metastatic lesions. Additionally, lesion volume, diffusion (ADC), and perfusion (rCBV) were analyzed to determine if segmentation discrepancies resulted in differences in imaging parameter estimates. There was strong similarity of the 3D volumes according to the DC (µ = 0.77), HD (µ = 3.89), and MHD (µ = 0.85). Imaging parameters between segmentation methods, agreed well for both diffusion (ADC R2 = 0.94), and perfusion (rCBV R2 = 0.986). Using 3D Slicer did not substantially decrease tracing time; however, it produced similar results by a novice to those of experts. This study supports the use of the Growth-Cut toolbox when expert manual segmentation does not exist. This finding is particularly useful for large scale studies that would otherwise require significant clinician involvement for ROI generation. |
A New Improved Method for Assessing Brain Deformation after Decompressive Craniectomy
|
Publication: PLoS One. 2014 Oct 10;9(10):e110408. PMID: 25303305 | PDF Authors: Fletcher TL, Kolias AG, Hutchinson PJ, Sutcliffe MP. Institution: Department of Engineering, University of Cambridge, Cambridge, UK. Background/Purpose: Decompressive craniectomy (DC) is a surgical intervention used following traumatic brain injury to prevent or alleviate raised intracranial pressure. However the clinical effectiveness of the intervention remains in doubt. The location of the craniectomy (unilateral or bifrontal) might be expected to change the brain deformation associated with the operation and hence the clinical outcome. As existing methods for assessing brain deformation have several limitations, we sought to develop and validate a new improved method. Funding:
|
Posterior Cerebral Artery Angle and the Rupture of Basilar Tip Aneurysms
|
Publication: PLoS One. 2014 Oct 29;9(10):e110946. PMID: 25353989 | PDF Authors: Ho AL, Mouminah A, Du R. Institution: Department of Neurosurgery, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Since the initial publication of the International Study of Unruptured Intracranial Aneurysms (ISUIA), management of unruptured intracranial aneurysms has been mainly based on the size of the aneurysm. The contribution of morphological characteristics to treatment decisions of unruptured aneurysms has not been well studied in a systematic and location specific manner. We present a large sample of basilar artery tip aneurysms (BTA) that were assessed using a diverse array of morphological variables to determine the parameters associated with ruptured aneurysms. Demographic and clinical risk factors of aneurysm rupture were obtained from chart review. CT angiograms (CTA) were evaluated with 3D Slicer, an open source visualization and image analysis software, to generate 3-D models of the aneurysms and surrounding vascular architecture. Morphological parameters examined in each model included aneurysm volume, aspect ratio, size ratio, aneurysm angle, basilar vessel angle, basilar flow angle, and vessel to vessel angles. Univariate and multivariate analyses were performed to determine statistical significance. From 2008-2013, 54 patients with BTA aneurysms were evaluated in a single institution, and CTAs from 33 patients (15 ruptured, 18 unruptured) were available and analyzed. Aneurysms that underwent reoperation, that were associated with arteriovenous malformations, or that lacked preoperative CTA were excluded. Multivariate logistic regression revealed that a larger angle between the posterior cerebral arteries (P1-P1 angle, p = 0.037) was most strongly associated with aneurysm rupture after adjusting for other morphological variables. In this location specific study of BTA aneurysms, the larger the angle formed between posterior cerebral arteries was found to be a new morphological parameter significantly associated with ruptured BTA aneurysms. This is a physically intuitive parameter that can be measured easily and readily applied in the clinical setting.
|
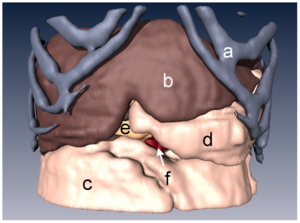
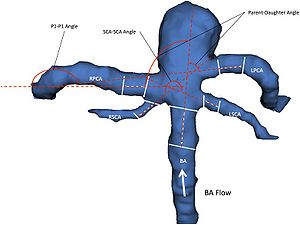 Figure 2 3D model of BTA aneurysm depicting angular variables of the surrounding vasculature. There were three vessel to vessel angles -measured. The Parent-Daughter angle is a composite angle that refers to the average of the two angles formed between the basilar artery (BA) and each posterior cerebral artery (RPCA, LPCA). The P1-P1 angle refers to the angle formed between the two posterior cerebral arteries (RPCA, LPCA). The SCA-SCA angle refers to the angle formed between the two superior cerebellar arteries (RSCA, LSCA). This 3D surface model of the aneurysm and surrounding vessels could be manipulated freely in the 3D Slicer environment. Volumes, lengths, and angles were then manually measured with fiducial-based tractography. |
A Nonrigid Registration Method for Correcting Brain Deformation Induced by Tumor Resection
|
Publication: Med Phys. 2014 Oct;41(10):101710. PMID: 25281949 | PDF Authors: Liu Y, Yao C, Drakopoulos F, Wu J, Zhou L, Chrisochoides N. Institution: Department of Computer Science, Old Dominion University, Norfolk, VA, USA. Background/Purpose: PURPOSE:
This paper presents a nonrigid registration method to align preoperative MRI with intraoperative MRI to compensate for brain deformation during tumor resection. This method extends traditional point-based nonrigid registration in two aspects: (1) allow the input data to be incomplete and (2) simulate the underlying deformation with a heterogeneous biomechanical model.
Funding:
|
 A) The complete flowchart to align preoperative MRI with intraoperative MRI, in which only the highlighted mesh generation and NEMNRR are addressed in this paper. The ventricle was segmented by a region growing method in 3D Slicer |
Distribution of Coronoid Fracture Lines by Specific Patterns of Traumatic Elbow Instability
|
Publication: J Hand Surg Am. 2014 Oct;39(10):2041-6. PMID: 25070699 | PDF Authors: Mellema JJ, Doornberg JN, Dyer GS, Ring D. Institution: Orthopaedic Hand and Upper Extremity Service, Massachusetts General Hospital, Boston, MA, USA. Background/Purpose: To determine if specific coronoid fractures relate to specific overall traumatic elbow instability injury patterns and to depict any relationship on fracture maps and heat maps. Methods: We collected 110 computed tomography (CT) studies from patients with coronoid fractures. Fracture types and pattern of injury were characterized based on anteroposterior and lateral radiographs, 2- and 3-dimensional CT scans, and intraoperative findings as described in operative reports. Using quantitative 3-dimensional CT techniques we were able to reconstruct the coronoid and reduce fracture fragments. Based on these reconstructions, fracture lines were identified and graphically superimposed onto a standard template in order to create 2-dimensional fracture maps. To further emphasize the fracture maps, the initial diagrams were converted into fracture heat maps following arbitrary units of measure. The Fisher exact test was used to evaluate the association between coronoid fracture types and elbow fracture-dislocation patterns. Results: Forty-seven coronoid fractures were associated with a terrible triad fracture dislocation, 30 with a varus posteromedial rotational injury, 1 with a anterior olecranon fracture dislocation, 22 with a posterior olecranon fracture dislocation, and 7 with a posterior Monteggia injury associated with terrible triad fracture dislocation of the elbow. The association between coronoid fracture types and elbow fracture-dislocation patterns, as shown on 2-dimensional fracture and heat maps, was strongly significant. Conclusions: Our fracture maps and heat maps support the observation that specific patterns of traumatic elbow instability have correspondingly specific coronoid fracture patterns. Knowledge of these patterns is useful for planning management because it directs exposure and fixation and helps identify associated ligament injuries and fractures that might benefit from treatment. Clinical Relevance: Two-dimensional fracture and heat mapping techniques may help surgeons to predict the distribution of coronoid fracture lines associated with specific injury patterns.
|
 Images show fracture fragment reduction of 3-dimensional mesh reconstructions in Rhinoceros (McNeel, Seattle, WA). A. Imported 3-dimensional mesh reconstruction was created in 3D Slicer. B. Fracture fragment selected for reduction. C. Image of 3-dimensional mesh reconstruction after reduction of the fracture fragment. |
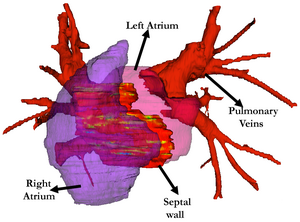
Cardiovascular Magnetic Resonance Imaging of Scar Development Following Pulmonary Vein Isolation: A Prospective Study
|
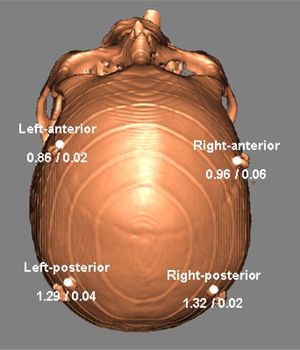
Publication: PLoS One. 2014 Sep 24;9(9):e104844. PMID: 25251403 | PDF Authors: Hsing J, Peters DC, Knowles BR, Manning WJ, Josephson ME. Institution: Department of Medicine, Cardiovascular Division, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA. Background/Purpose: Decompressive craniectomy (DC) is a surgical intervention used following traumatic brain injury to prevent or alleviate raised intracranial pressure. However the clinical effectiveness of the intervention remains in doubt. The location of the craniectomy (unilateral or bifrontal) might be expected to change the brain deformation associated with the operation and hence the clinical outcome. As existing methods for assessing brain deformation have several limitations, we sought to develop and validate a new improved method. Funding:
|
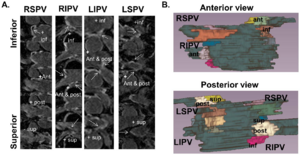 16 segment model showing the 4 regions evaluated around each pulmonary vein. A) Zoomed and cropped slices labeled by region. B) 3D color-coded display, showing 4 regions about each PV, with explicit labeling for the right inferior and left superior PV. Image analyses were performed using ImageJ (NIH Image, Bethesda, MD) and 3D Slicer (v3.6, NA-MIC, Boston, MA). |
Bi-modal Non-rigid Registration of Brain MRI Data with Deconvolution of Joint Statistics
|
Publication: IEEE Trans Image Process. 2014 Sep;23(9):3999-4009. PMID: 25020093 Authors: Pilutti D, Strumia M, Hadjidemetriou S. Institution: Department of Radiology Medical Physics, University Medical Center Freiburg, Freiburg, Germany. Background/Purpose: A brain MRI protocol typically includes several imaging contrasts that can provide complementary information by highlighting different tissue properties. The acquired data sets often need to be coregistered or placed in a standard anatomic space before any further processing. Current registration methods particularly for multicontrast data are computationally very intensive, their resolution is lower than that of the images, and their distance metric and its optimization can be limiting. In this paper, a novel and effective nonrigid registration method is proposed that is based on the restoration of the joint statistics of pairs of such images. The registration is performed with the deconvolution of the joint statistics with an adaptive Wiener filter. The deconvolved statistics are forced back to the spatial domain to estimate a preliminary registration. The spatial transformation is also regularized with Gaussian spatial smoothing. The registration method has been compared with the B-Splines method implemented in 3D Slicer and with the SyN method implemented in the ANTs toolkit. The validation has been performed with a simulated Shepp–Logan phantom, a BrainWeb phantom, the real data of the NIREP database, and real multicontrast data sets of healthy volunteers. The proposed method has shown improved comparative accuracy as well as analytical efficiency. |
Clinical Testing of an Alternate Method of Inserting Bone-Implanted Fiducial Markers
|
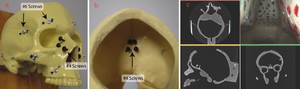
Publication: Int J Comput Assist Radiol Surg. 2014 Sep;9(5):913-20. PMID: 24493228 | PDF Authors: Balachandran R, Fritz MA, Dietrich MS, Danilchenko A, Mitchell JE, Oldfield VL, Lipscomb WW, Fitzpatrick JM, Neimat JS, Konrad PE, Labadie RF. Institution: Department of Otolaryngology, Vanderbilt University Medical Center, Nashville, TN, USA. Background/Purpose: Deep brain stimulation (DBS) surgery utilizes image guidance via bone-implanted fiducial markers to achieve the desired submillimetric accuracy and to provide means for attaching microstereotactic frames. For maximal benefit, the markers must be inserted to the correct depth since over-insertion leads to stripping and under-insertion leads to instability. PURPOSE: The purpose of the study was to test clinically a depth-release drive system, the PosiSeat™, versus manual insertion (pilot hole followed by manual screwing until tactile determined correct seating) for implanting fiducial markers into the bone. Methods: With institutional review board approval, the PosiSeat™ was used to implant markers in 15 DBS patients (57 fiducials). On post-insertion CT scans, the depth of the gap between the shoulder of the fiducial markers and the closest bone surface was measured. Similar depth measurements were performed on the CT scans of 64 DBS patients (250 fiducials), who underwent manual fiducial insertion. Results: Median of shoulder-to-bone distance for PosiSeat™ and manual insertion group were 0.03 and 1.06 mm, respectively. Fifty percent of the fiducials had the shoulder-to-bone distances within 0.01-0.09 mm range for the PosiSeat group and 0.04-1.45 mm range for the manual insertion group. These differences were statistically significant. Conclusions: A depth-release drive system achieves more consistent placement of bone-implanted fiducial markers than manual insertion. Funding:
|
 Median shoulder-to-bone distances at typical anchor locations. The anchor locations are shown as white circles. The two values associated with each location indicate the median value of the shoulder-to-bone distance in mm using the manual method and the PosiSeat method respectively. The scans of patients were analyzed with 3D Slicer Version 3.4. |
Three-Dimensional Imaging of HIV-1 Virological Synapses Reveals Membrane Architectures Involved in Virus Transmission
|
Publication: J. Virol. 2014 Sept; 88(18):10327-39. PMID: 24965444 | PDF Authors: Do T, Murphy G, Earl LA, Del Prete GQ, Grandinetti G, Li GH, Estes JD, Rao P, Trubey CM, Thomas J, Spector J, Bliss D, Nath A, Lifson JD, Subramaniam S. Institution: Laboratory of Cell Biology, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Bethesda, Maryland, USA. Background/Purpose: HIV transmission efficiency is greatly increased when viruses are transmitted at virological synapses formed between infected and uninfected cells. We have previously shown that virological synapses formed between HIV-pulsed mature dendritic cells (DCs) and uninfected T cells contain interdigitated membrane surfaces, with T cell filopodia extending toward virions sequestered deep inside invaginations formed on the DC membrane. To explore membrane structural changes relevant to HIV transmission across other types of intercellular conjugates, we used a combination of light and focused ion beam scanning electron microscopy (FIB-SEM) to determine the three-dimensional (3D) architectures of contact regions between HIV-1-infected CD4+ T cells and either uninfected human CD4+ T cells or human fetal astrocytes. We present evidence that in each case, membrane extensions that originate from the uninfected cells, either as membrane sheets or filopodial bridges, are present and may be involved in HIV transmission from infected to uninfected cells. We show that individual virions are distributed along the length of astrocyte filopodia, suggesting that virus transfer to the astrocytes is mediated, at least in part, by processes originating from the astrocyte itself. Mechanisms that selectively disrupt the polarization and formation of such membrane extensions could thus represent a possible target for reducing viral spread. Funding:
|
 Segmentation of FIB-SEM data shows clear differences between Jurkat cell and primary CD4+ T cell synapses. (A and B) Segmentation of Jurkat cells from the data set in Fig. 3 reveals three infected (*) and two uninfected cells. (B) Zoomed-in view of the cells in panel A. Short membrane extensions cross the synapse from both infected and uninfected cells. (C to F) Uninfected and HIV-1 NL4-3-infected primary CD4+ T cells were cocultured for 8 h and imaged as described for panels A and B. (C) Zoomed-out view of the primary cell cluster reveals extensive membrane interdigitation between infected (*) and uninfected cells. Several virions (red) can be seen at the contact zones with infected cells. (D) Rotated view of the cells shown in panel C. An uninfected cell (brown) with a large membrane-enclosed extension (white arrow) stretches around another uninfected cell (purple), making direct contact with an infected cell (blue). (E) Segmentation of primary T cell cluster shows close contacts between uninfected and infected (*) T cells, as well as a long filopodial contact between the infected cell and a distant, uninfected cell. (F) Back view of the primary cell cluster shown in panel E. Cells display many long filopodia and membrane extensions, common in primary CD4+ T cells but not in Jurkat cells. e. Features of interest were automatically selected with 3DSlicer, or Avizo Fire (Visualization Sciences Group) using a thresholding tool. |
How Action Selection can be Embodied: Intracranial Gamma Band Recording Shows Response Competition during the Eriksen Flankers Test
|
Publication: Front Hum Neurosci. 2014 Aug 26;8:668. PMID: 25206328 | PDF Authors: Caruana F, Uithol S, Cantalupo G, Sartori I, Lo Russo G, Avanzini P. Institution: Brain Center for Social and Motor Cognition - Istituto Italiano di Tecnologia Parma, Italy. Background/Purpose: Recent findings in monkeys suggest that action selection is based on a competition between various action options that are automatically planned by the motor system. Here we discuss data from intracranial EEG recordings in human premotor cortex (PMC) during a bimanual version of the Eriksen flankers test that suggest that the same principles apply to human action decisions. Recording sites in the dorsal PMC show an early but undifferentiated activation, a delayed response that depends on the experimental conditions and, finally, a movement related activation during action execution. Additionally, we found that the medial part of the PMC show a significant increase in response for ipsilateral trials, suggesting a role in inhibiting the wrong response. The ventral PMC seems to be involved in action execution, rather than action selection. Together these findings suggest that the human PMC is part of a network that specifies, selects, and executes actions. Funding:
|
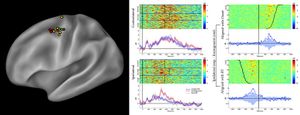 (Left panel) Sites showing significant unspecific, short-latency activations according to the gamma band reactivity within 100 ms after stimulus onset, are shown in yellow. Choice-related sites, showing significant activation during the incongruent trials, are shown in red. Furthermore, sites showing both effect are shown in green. Results are plotted on a template (Caret® ) according to their MNI coordinates. (Central panel) Results from a representative d premotor cortex (PMC) site are shown (P3, M’12). Figure shows the gamma modulation during the congruent, incongruent, and neutral trials requiring a response with the hand contralateral (top) and ipsilateral (bottom) to the implanted hemisphere. Data are aligned with the stimulus onset. The average reaction time for the three conditions is shown at the single trial level (black vertical lines). The short-latency activations is clear in both contralateral- and ipsilateral-response trials, in the three conditions. In the contralateral-response trials the activity is prolonged after the response, while in the ipsilateral-response trials is suppressed before the response. The greater activity during the incongruent conditions is visible in the ipsilateral-response trials. (Right panel) The same dataset, showing a representative dPMC site (P3, M’12) during the incongruent condition requiring a response with the ipsilateral hand, aligned to both the onset of the stimulus (upper part) and the onset of the response (lower panel). For each selected alignment, the other event is indicated by a curved line. Cerebral structures explored by each electrode contact were visualized by a software package for visualization and image analysis (3D Slicer). |
Airway Wall Thickness is Increased in COPD Patients with Bronchodilator Responsiveness
|
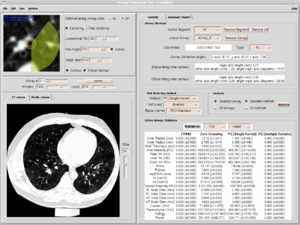
Publication: Respir Res. 2014 Aug 8;15:84. PMID: 25248436 | PDF Authors: Kim V, Desai P, Newell JD, Make BJ, Washko GR, Silverman EK, Crapo JD, Bhatt SP, Criner GJ; COPDGene Investigators. Institution: Temple University School of Medicine, Philadelphia, PA, USA. Background/Purpose: Bronchodilator responsiveness (BDR) is a common but variable phenomenon in COPD. The CT characteristics of airway dimensions that differentiate COPD subjects with BDR from those without BDR have not been well described. We aimed to assess airway dimensions in COPD subjects with and without BDR. Methods: We analyzed subjects with GOLD 1-4 disease in the COPDGene® study who had CT airway analysis. We divided patients into two groups: BDR + (post bronchodilator ΔFEV1 ≥ 10%) and BDR-(post bronchodilator ΔFEV1 < 10%). The mean wall area percent (WA%) of six segmental bronchi in each subject was quantified using VIDA. Using 3D Slicer, airway wall thickness was also expressed as the square root wall area of an airway of 10 mm (Pi10) and 15 mm (Pi15) diameter. %Emphysema and %gas trapping were also calculated. Results: 2355 subjects in the BDR-group and 1306 in the BDR + group formed our analysis. The BDR + group had a greater Pi10, Pi15, and mean segmental WA% compared to the BDR-group. In multivariate logistic regression using gender, race, current smoking, history of asthma, %emphysema, %gas trapping, %predicted FEV1, and %predicted FVC, airway wall measures remained independent predictors of BDR. Using a threshold change in FEV1 ≥ 15% and FEV1 ≥ 12% and 200 mL to divide patients into groups, the results were similar. Conclusion: BDR in COPD is independently associated with CT evidence of airway pathology. This study provides us with greater evidence of changes in lung structure that correlate with physiologic manifestations of airflow obstruction in COPD. Funding:
|
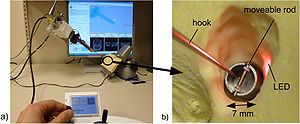
Compact Robotically Steerable Image-Guided Instrument for Multi-Adjacent-Point (MAP) Targeting
|
Publication: IEEE Transactions on Robotics. 2014 Aug;30(4):802-15. Authors: Torabi M, Gupta R, Walsh C.J. Institution: Harvard University, Cambridge, MA, USA. Background/Purpose: Accurately targeting multi-adjacent points (MAPs) during image-guided percutaneous procedures is challenging due to needle deflection and misalignment. The associated errors can result in inadequate treatment of cancer in the case of prostate brachytherapy, or inaccurate diagnosis during biopsy, while repeated insertions increase procedure time, radiation dose, and complications. To address these challenges, we present an image-guided robotic system capable of MAP targeting of irregularly shaped volumes after a single insertion of a percutaneous instrument. The design of the compact CT-compatible drive mechanism is based on a nested screw and screw-spline combination that actuates a straight outer cannula and a curved inner stylet that can be repeatedly straightened when retracted inside the cannula. The stylet translation and cannula rotation/translation enable a 3-D workspace to be reached with the stylet's tip. A closed-form inverse kinematics and image-to-robot registration are implemented in an image-guided system including a point-and-click user interface. The complete system is successfully evaluated with a phantom under a Siemens Definition Flash CT scanner. We demonstrate that the system is capable of MAP targeting for a 2-D shape of the letter “H” and a 3-D helical pattern with an average targeting error of 2.41 mm. These results highlight the benefit and efficacy of the proposed robotic system in seed placement during image-guided brachytherapy. Funding: Harvard School of Engineering and Applied Sciences, Cambridge, MA, USA. |
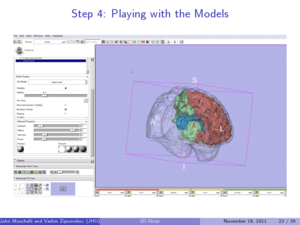
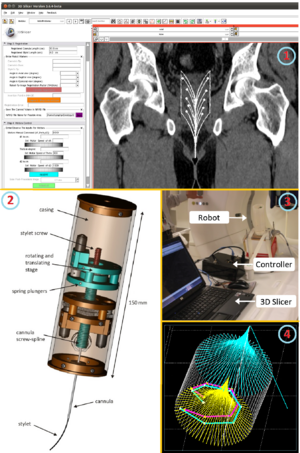 1. Graphical user interface, the robot kinematics, and the image-to-robot registration were developed and integrated into the new image-guided-therapy module in 3D Slicer. 2. Robotically steerable percutaneous instrument that targets multiple adjacent points in irregularly-shaped volumes in soft tissue after a single needle insertion. 3. Robot, positioned with some arbitrary angles on the CT scanner bed, ready to move inside a Dual Source MDCT Siemens scanner. The robot was connected via Ethernet to a laptop computer via OpenIGTLink. 4. The green and pink plots, visualized inside the feasible volume, are the planned and actual shapes of a 3D helix respectively, which represents the location of the seeds in phantom. |
Combined Compared to Dissociated Oral and Intestinal Sucrose Stimuli induce Different Brain Hedonic Processes
|
Publication: Front Psychol. 2014 Aug; 5: 861. PMID: 25147536 | PDF Authors: Clouard C, Meunier-Salaün M-C, Meurice P, Malbert C-H, Val-Laillet D. Institution: INRA, UR1341 Alimentation et Adaptations Digestives, Nerveuses et Comportementales, Saint Gilles, France. Background/Purpose: The characterization of brain networks contributing to the processing of oral and/or intestinal sugar signals in a relevant animal model might help to understand the neural mechanisms related to the control of food intake in humans and suggest potential causes for impaired eating behaviors. This study aimed at comparing the brain responses triggered by oral and/or intestinal sucrose sensing in pigs. Seven animals underwent brain single photon emission computed tomography (99mTc-HMPAO) further to oral stimulation with neutral or sucrose artificial saliva paired with saline or sucrose infusion in the duodenum, the proximal part of the intestine. Oral and/or duodenal sucrose sensing induced differential cerebral blood flow changes in brain regions known to be involved in memory, reward processes and hedonic (i.e., pleasure) evaluation of sensory stimuli, including the dorsal striatum, prefrontal cortex, cingulate cortex, insular cortex, hippocampus, and parahippocampal cortex. Sucrose duodenal infusion only and combined sucrose stimulation induced similar activity patterns in the putamen, ventral anterior cingulate cortex and hippocampus. Some brain deactivations in the prefrontal and insular cortices were only detected in the presence of oral sucrose stimulation. Finally, activation of the right insular cortex was only induced by combined oral and duodenal sucrose stimulation, while specific activity patterns were detected in the hippocampus and parahippocampal cortex with oral sucrose dissociated from caloric load. This study sheds new light on the brain hedonic responses to sugar and has potential implications to unravel the neuropsychological mechanisms underlying food pleasure and motivation.
|
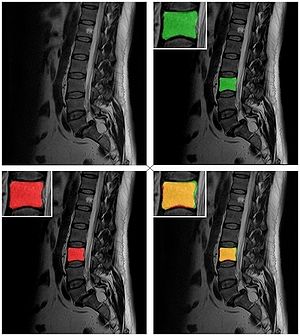
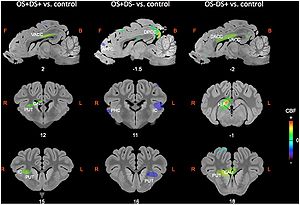 Sagittal and coronal MRI sections showing clusters of differential cerebral blood flow identified during the small volume correction (SVC) analyses in different regions of interest chosen upon a priori hypotheses for the three following contrasts: OS+DS+ (oral and duodenal sucrose stimulation) vs. control, OS+DS- (oral sucrose stimulation) vs. control, and OS-DS+ (duodenal sucrose stimulation) vs. control. The x or y coordinates in the CA–CP (commissura anterior–commissura posterior) plane are indicated below the images. The threshold for significance was set at P < 0.01 (uncorrected). Positive cerebral blood flow (CBF) values indicate a brain metabolism activation and negative CBF values indicate a brain metabolism deactivation compared to control. L, left; R, right; APFC, anterior prefrontal cortex; CAU, caudate nucleus; PUT, putamen; HIP, hippocampus; IC, insular cortex; DACC, dorsal anterior cingulate cortex; VACC, ventral anterior cingulate cortex; PHC, parahippocampal cortex. The representation of the clusters with different metabolism was performed using 3D Slicer. |
Microstructural Changes in the Striatum and Their Impact on Motor and Neuropsychological Performance in Patients with Multiple Sclerosis
|
Publication: PLoS One. 2014 Jul 21;9(7):e101199. PMID: 25047083 | PDF Authors: Cavallari M, Ceccarelli A, Wang GY, Moscufo N, Hannoun S, Matulis CR, Jackson JS, Glanz BI, Bakshi R, Neema M, Guttmann CR. Institution: Dipartimento di Neuroscienze, Salute Mentale e Organi di Senso (NESMOS), Università La Sapienza, Rome, Italy. Background/Purpose: Grey matter (GM) damage is a clinically relevant feature of multiple sclerosis (MS) that has been previously assessed with diffusion tensor imaging (DTI). Fractional anisotropy (FA) of the basal ganglia and thalamus might be increased in MS patients, and correlates with disability scores. Despite the established role of the striatum and thalamus in motor control, mood and cognition, the impact of DTI changes within these structures on motor and neuropsychological performance has not yet been specifically addressed in MS. We investigated DTI metrics of deep GM nuclei and their potential association with mobility and neuropsychological function. DTI metrics from 3T MRI were assessed in the caudate, putamen, and thalamus of 30 MS patients and 10 controls. Sixteen of the patients underwent neuropsychological testing. FA of the caudate and putamen was higher in MS patients compared to controls. Caudate FA correlated with Expanded Disability Status Scale score, Ambulation Index, and severity of depressive symptomatology. Putamen and thalamus FA correlated with deficits in memory tests. In contrast, cerebral white matter (WM) lesion burden showed no significant correlation with any of the disability, mobility and psychometric parameters. Our findings support evidence of FA changes in the basal ganglia in MS patients, as well as deep GM involvement in disabling features of MS, including mobility and cognitive impairment. Deep GM FA appears to be a more sensitive correlate of disability than WM lesion burden. Funding:
|
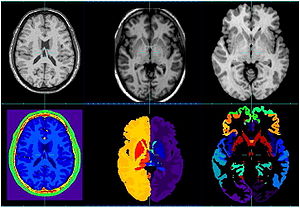
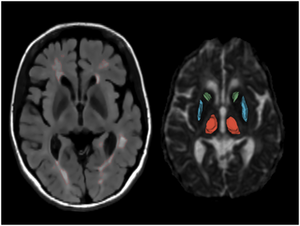 MRI example of white matter lesions and the segmented deep grey matter structures. Lesions and anatomical regions of interest are illustrated on a set of MR images from a 53 year-old male MS patient. Left – axial FLAIR; right – axial diffusivity map. The output of computer-assisted segmentation of the lesions is shown on FLAIR. The 3D models of the manually outlined caudate (green), putamen (blue) and thalamus (red) are overlaid on the fractional anisotropy map of a single section containing these structures. The putamen and the thalamus was manually outlined on AD maps using 3D Slicer (www.slicer.org) |
Design and Initial Evaluation of a Treatment Planning Software System for MRI-guided Laser Ablation in the Brain
|
Publication: Int J Comput Assist Radiol Surg. 2014 Jul;9(4):659-67. PMID: 24091853 Authors: Yeniaras E, Fuentes DT, Fahrenholtz SJ, Weinberg JS, Maier F, Hazle JD, Stafford RJ. Institution: Department of Imaging Physics, University of Texas MD Anderson Cancer Center, Houston, TX, USA. Background/Purpose: An open-source software system for planning magnetic resonance (MR)-guided laser-induced thermal therapy (MRgLITT) in brain is presented. The system was designed to provide a streamlined and operator-friendly graphical user interface (GUI) for simulating and visualizing potential outcomes of various treatment scenarios to aid in decisions on treatment approach or feasibility. Methods: A portable software module was developed on the 3D Slicer platform, an open-source medical imaging and visualization framework. The module introduces an interactive GUI for investigating different laser positions and power settings as well as the influence of patient-specific tissue properties for quickly creating and evaluating custom treatment options. It also provides a common treatment planning interface for use by both open-source and commercial finite element solvers. In this study, an open-source finite element solver for Pennes' bioheat equation is interfaced to the module to provide rapid 3D estimates of the steady-state temperature distribution and potential tissue damage in the presence of patient-specific tissue boundary conditions identified on segmented MR images. Results: The total time to initialize and simulate an MRgLITT procedure using the GUI was [Formula: see text]5 min. Each independent simulation took [Formula: see text]30 s, including the time to visualize the results fused with the planning MRI. For demonstration purposes, a simulated steady-state isotherm contour was correlated with MR temperature imaging (N = 5). The mean Hausdorff distance between simulated and actual contours was 2.0 mm, whereas the mean Dice similarity coefficient was 0.93. Conclusion: We have designed, implemented, and conducted initial feasibility evaluations of a software tool for intuitive and rapid planning of MRgLITT in brain. The retrospective in vivo dataset presented herein illustrates the feasibility and potential of incorporating fast, image-based bioheat predictions into an interactive virtual planning environment for such procedures. Funding:
|
Orbitofrontal Cortex Volume in Area 11/13 Predicts Reward Devaluation, but not Reversal Learning Performance, in Young and Aged Monkeys
|
Publication: J Neurosci. 2014 Jul 23;34(30):9905-16. PMID: 25057193 | PDF Authors: Burke SN, Thome A, Plange K, Engle JR, Trouard TP, Gothard KM, Barnes CA. Institution: ARL Division of Neural Systems, Memory & Aging, Evelyn F. McKnight Brain Institute, University of Arizona, Tucson, AZ, USA. Background/Purpose: The orbitofrontal cortex (OFC) and amygdala are both necessary for decisions based on expected outcomes. Although behavioral and imaging data suggest that these brain regions are affected by advanced age, the extent to which aging alters appetitive processes coordinated by the OFC and the amygdala is unknown. In the current experiment, young and aged bonnet macaques were trained on OFC- and amygdala-dependent tasks that test the degree to which response selection is guided by reward value and can be adapted when expected outcomes change. To assess whether the structural integrity of these regions varies with levels of performance on reward devaluation and object reversal tasks, volumes of areas 11/13 and 14 of the OFC, central/medial (CM), and basolateral (BL) nuclei of the amygdala were determined from high-resolution anatomical MRIs. With age, there were significant reductions in OFC, but not CM and BL, volume. Moreover, the aged monkeys showed impairments in the ability to associate an object with a higher value reward, and to reverse a previously learned association. Interestingly, greater OFC volume of area 11/13, but not 14, was significantly correlated with an animal's ability to anticipate the reward outcome associated with an object, and smaller BL volume was predictive of an animal's tendency to choose a higher value reward, but volume of neither region correlated with reversal learning. Together, these data indicate that OFC volume has an impact on monkeys' ability to guide choice behavior based on reward value but does not impact ability to reverse a previously learned association. 3D Slicer; Pieper and Kikinis, Harvard Medical School) was used to preprocess brain images.
|
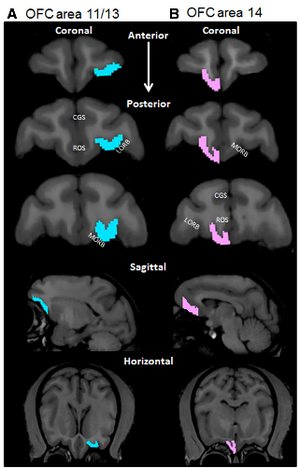 OFC boundaries. Representative boundaries of the OFC for areas 11/13 in the left hemisphere (A; blue) and 14 in the right hemisphere (B; pink) (scan view of left and right hemispheres are reversed). Two independent observers determined the OFC ROI according to the guidelines of Carmichael and Price (1994 ) and Preuss and Goldman-Rakic (1991). The top three images show representative coronal sections along the anterior to posterior axis. The fourth row of images represents a representative sagittal section; and the bottom row represents horizontal sections containing the OFC from the same monkey. CGS, Cingulatesulcus; ROS, rostral sulcus; LORB, lateral orbital sulcus; MORB, medial orbital sulcus. |
Robust Radiomics Feature Quantification using Semiautomatic Volumetric Segmentation
|
Publication: PLoS One. 2014 Jul; 9(7):e102107. PMID: 25025374 | PDF Authors: Parmar C, Rios Velazquez E, Leijenaar R, Jermoumi M, Carvalho S, Mak RH, Mitra S, Shankar BU, Kikinis R, Haibe-Kains B, Lambin P, Aerts HJ. Institution: Department of Radiation Oncology, Dana-Farber Cancer Institute, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Due to advances in the acquisition and analysis of medical imaging, it is currently possible to quantify the tumor phenotype. The emerging field of Radiomics addresses this issue by converting medical images into minable data by extracting a large number of quantitative imaging features. One of the main challenges of Radiomics is tumor segmentation. Where manual delineation is time consuming and prone to inter-observer variability, it has been shown that semi-automated approaches are fast and reduce inter-observer variability. In this study, a semiautomatic region growing volumetric segmentation algorithm, implemented in the free and publicly available 3D Slicer platform, was investigated in terms of its robustness for quantitative imaging feature extraction. Fifty-six 3D-radiomic features, quantifying phenotypic differences based on tumor intensity, shape and texture, were extracted from the computed tomography images of twenty lung cancer patients. These radiomic features were derived from the 3D-tumor volumes defined by three independent observers twice using 3D Slicer, and compared to manual slice-by-slice delineations of five independent physicians in terms of intra-class correlation coefficient (ICC) and feature range. Radiomic features extracted from 3D Slicer segmentations had significantly higher reproducibility (ICC = 0.8560.15, p = 0.0009) compared to the features extracted from the manual segmentations (ICC = 0.7760.17). Furthermore, we found that features extracted from 3D Slicer segmentations were more robust, as the range was significantly smaller across observers (p = 3.819e-07), and overlapping with the feature ranges extracted from manual contouring (boundary lower: p = 0.007, higher: p = 5.863e-06). Our results show that 3D Slicer segmented tumor volumes provide a better alternative to the manual delineation for feature quantification, as they yield more reproducible imaging descriptors. Therefore, 3D Slicer can be employed for quantitative image feature extraction and image data mining research in large patient cohorts. Funding:
UM 2011-5020, KWF UM 2009-4454)
|
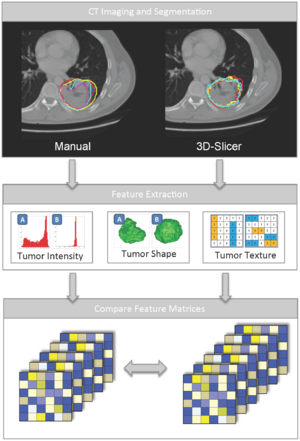 Schematic diagram depicting the overview of the analysis. A: First, we performed five manual delineations and six 3D Slicer segmentations (three observers twice) on twenty lung tumors. B: Second, fifty-six radiomic features quantifying tumor intensity, texture and shape were extracted from these segmentations. C: Third, the resulting feature matrices were compared for robustness of the feature values. |
Tranexamic Acid for Spontaneous Intracerebral Hemorrhage: A Randomized Controlled Pilot Trial (ISRCTN50867461)
|
Publication: J Stroke Cerebrovasc Dis. 2014 Jul;23(6):1312-8. PMID: 24680087 | PDF Authors: Sprigg N, Renton CJ, Dineen RA, Kwong Y, Bath PM. Institution: Stroke Trials Unit, Division of Clinical Neurosciences, School of Medicine, University of Nottingham, Nottingham, UK. Background/Purpose: Spontaneous intracerebral hemorrhage (ICH) can be devastating, particularly if hematoma expansion (HE) occurs. Tranexamic acid (TA), an antifibrinolytic drug, significantly reduced mortality in bleeding patients after trauma in the large CRASH-2 trial. The CRASH-2 ICH substudy found that TA nonsignificantly reduced mortality and dependency in traumatic ICH. The aim of this study was to assess the feasibility of performing a randomized controlled trial of tranexamic acid in spontaneous ICH, ahead of a definitive study. Methods: We performed a single-center, prospective, randomized (2:1), double-blind, placebo-controlled blinded endpoint trial of TA (intravenous 1 g bolus, 1 g infusion/8 h) in acute (<24 hours) spontaneous ICH. The primary objective was to test the feasibility of recruiting to the trial. Other objectives included tolerability (adverse events) and the effect of TA on HE and death and dependency. Results: The trial was feasible, with 24 patients enrolled (TA, n=16; placebo, n=8) between March 2011 and March 2012, and acceptable-only 3 patients declined to participate. All patients received the correct randomized treatment; 1 patient in the TA group did not complete the infusion because of neurologic deterioration. There were no significant differences in secondary outcomes including adverse events, HE, death, and dependency. One patient in the TA group had a deep vein thrombosis. Conclusions: This, the first randomized controlled trial of TA in ICH, found that the protocol could be delivered on schedule (2 patients/mo) and was feasible. Larger studies are needed to assess safety and efficacy of TA in ICH. The data were converted to analyze format before volumetric analysis using 3D Slicer software. |
|
Publication: IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI), 2014 Jun; | PDF Authors: Burke SN, Thome A, Plange K, Engle JR, Trouard TP, Gothard KM, Barnes CA. Institution: ARL Division of Neural Systems, Memory & Aging, Evelyn F. McKnight Brain Institute, University of Arizona, Tucson, AZ, USA. Background/Purpose: The orbitofrontal cortex (OFC) and amygdala are both necessary for decisions based on expected outcomes. Although behavioral and imaging data suggest that these brain regions are affected by advanced age, the extent to which aging alters appetitive processes coordinated by the OFC and the amygdala is unknown. In the current experiment, young and aged bonnet macaques were trained on OFC- and amygdala-dependent tasks that test the degree to which response selection is guided by reward value and can be adapted when expected outcomes change. To assess whether the structural integrity of these regions varies with levels of performance on reward devaluation and object reversal tasks, volumes of areas 11/13 and 14 of the OFC, central/medial (CM), and basolateral (BL) nuclei of the amygdala were determined from high-resolution anatomical MRIs. With age, there were significant reductions in OFC, but not CM and BL, volume. Moreover, the aged monkeys showed impairments in the ability to associate an object with a higher value reward, and to reverse a previously learned association. Interestingly, greater OFC volume of area 11/13, but not 14, was significantly correlated with an animal's ability to anticipate the reward outcome associated with an object, and smaller BL volume was predictive of an animal's tendency to choose a higher value reward, but volume of neither region correlated with reversal learning. Together, these data indicate that OFC volume has an impact on monkeys' ability to guide choice behavior based on reward value but does not impact ability to reverse a previously learned association. 3D Slicer; Pieper and Kikinis, Harvard University) was used to preprocess brain images. Funding:
|
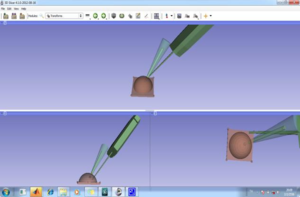 Real-time movement of 3D models in 3D Slicer Software. |
The Efficacy of Neuroendoscopic Treatment for Middle Cranial Fossa Arachnoid Cysts Assessed by MRI 3D Segmentation and Modeling
|
Publication: Childs Nerv Syst. 2014 Jun;30(6):1037-44. PMID: 24258453 Authors: Li Y, Chen X, Xu B. Institution: Department of Neurosurgery, People's Liberation Army General Hospital, Beijing, China. Background/Purpose: The purpose of this study was to present a more precise and objective way to assess the effectiveness of neuroendoscopic application in the treatment of middle cranial fossa arachnoid cysts. Methods: Between March 2009 and December 2012, 28 patients affected by middle cranial fossa arachnoid cysts were initially treated with endoscopic fenestration at the three spaces. The volumes of the cysts on MR images at the time of pre-op and 4 months after surgery were reconstructed by 3D Slicer and quantitatively calculated to compare the volumetric changes. The possible predisposing factors of surgical outcomes were analyzed as well. Results: All the models of the cysts were successfully reconstructed, and the mean volume of the cysts was 135.77 ± 90.43 cm3 before surgery and 93.08 ± 100.31 cm3 after surgery at 4 months follow-up (t = 2.98, P = 0.006). The volumes of those two cases (7.14 %), presenting intracranial hypertension and ventricular dilation after surgery, were dramatically increased, whereas the others were decreased in 20 cases (71.43 %) or remained unchanged in 6 cases (21.43 %). There was significant difference on the age factor among the three result groups (P = 0.001). Conclusion: The reconstruction of 3D for the assessment of the endoscopic fenestration outcomes is a feasible and precise way for clinical work. The variety of outcomes probably depends on age discrepancy. |
Relationship between Interleukin-6 Gene Polymorphism and Hippocampal Volume in Antipsychotic-Naïve Schizophrenia: Evidence for Differential Susceptibility?
|
Publication: PLoS One. 2014 May 2;9(5):e96021. PMID: 24787542 | PDF Authors: Kalmady SV, Venkatasubramanian G, Shivakumar V, Gautham S, Subramaniam A, Jose DA, Maitra A, Ravi V, Gangadhar BN. Institution: The Schizophrenia Clinic, Department of Psychiatry, National Institute of Mental Health and Neuro Sciences, Bangalore, India. Background/Purpose: Various lines of evidence including epidemiological, genetic and foetal pathogenetic models suggest a compelling role for Interleukin-6 (IL-6) in the pathogenesis of schizophrenia. IL-6 mediated inflammatory response triggered by maternal infection or stress induces disruption of prenatal hippocampal development which might contribute towards psychopathology during adulthood. There is a substantial lack of knowledge on how genetic predisposition to elevated IL-6 expression effects hippocampal structure in schizophrenia patients. In this first-time study, we evaluated the relationship between functional polymorphism rs1800795 of IL-6 and hippocampal gray matter volume in antipsychotic-naïve schizophrenia patients in comparison with healthy controls. Funding:
|
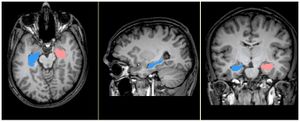 Cerebral MRI depicting manual segmentation of hippocampus. Figure shows MRI with segmented hippocampus in axial, sagittal & coronal sections within 3D Slicer software interface. |
Multi-Modal Glioblastoma Segmentation: Man versus Machine
|
Publication: PLoS One. 2014 May; 9(5):e96873. PMID: 24804720 | PDF Authors: Porz N, Bauer S, Pica A, Schucht P, Beck J, Verma RK, Slotboom J, Reyes M, Wiest R. Institution: Support Center for Advanced Neuroimaging - Institute for Diagnostic and Interventional Neuroradiology, University Hospital Inselspital and University of Bern, Bern, Switzerland. Background/Purpose: Reproducible segmentation of brain tumors on magnetic resonance images is an important clinical need. This study was designed to evaluate the reliability of a novel fully automated segmentation tool for brain tumor image analysis in comparison to manually defined tumor segmentations. Methods: We prospectively evaluated preoperative MR Images from 25 glioblastoma patients. Two independent expert raters performed manual segmentations. Automatic segmentations were performed using the Brain Tumor Image Analysis software (BraTumIA). In order to study the different tumor compartments, the complete tumor volume TV (enhancing part plus non-enhancing part plus necrotic core of the tumor), the TV+ (TV plus edema) and the contrast enhancing tumor volume CETV were identified. We quantified the overlap between manual and automated segmentation by calculation of diameter measurements as well as the Dice coefficients, the positive predictive values, sensitivity, relative volume error and absolute volume error. Results: Comparison of automated versus manual extraction of 2-dimensional diameter measurements showed no significant difference (p = 0.29). Comparison of automated versus manual segmentation of volumetric segmentations showed significant differences for TV+ and TV (p<0.05) but no significant differences for CETV (p>0.05) with regard to the Dice overlap coefficients. Spearman's rank correlation coefficients (ρ) of TV+, TV and CETV showed highly significant correlations between automatic and manual segmentations. Tumor localization did not influence the accuracy of segmentation. Conclusions: In summary, we demonstrated that BraTumIA supports radiologists and clinicians by providing accurate measures of cross-sectional diameter-based tumor extensions. The automated volume measurements were comparable to manual tumor delineation for CETV tumor volumes, and outperformed inter-rater variability for overlap and sensitivity. Funding:
|
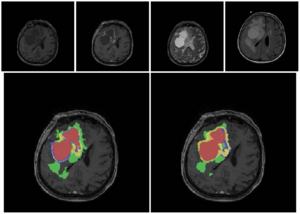 The figures show the original images and the segmentations as overlays on the post-contrast T1-weighted images for a patient with a good overlap of manual and automatic segmentation. Upper row: an axial slice of the original images (T1w, T1wGd, T2, FLAIR from left to right). Bottom row left column: manual segmentation, right column: automatic segmentation. Color code for segmentations: red = necrosis, yellow = enhancing tumor, blue = non-enhancing tumor, green = edema. TV+ corresponds to a combination of all colors, TV corresponds to red+yellow+blue compartments, CETV corresponds to the yellow compartment. Manual segmentation was performed with the open source software 3D Slicer Version 4.2.2.3. |
Rapid Amygdala Responses during Trace Fear Conditioning without Awareness
|
Publication: PLoS One. 2014 May 13;9(5):e96803. PMID: 24823365 | PDF Authors: Balderston NL, Schultz DH, Baillet S, Helmstetter FJ. Institution: Department of Psychology, University of Wisconsin-Milwaukee, Milwaukee, WI, USA. Background/Purpose: The role of consciousness in learning has been debated for nearly 50 years. Recent studies suggest that conscious awareness is needed to bridge the gap when learning about two events that are separated in time, as is true for trace fear conditioning. This has been repeatedly shown and seems to apply to other forms of classical conditioning as well. In contrast to these findings, we show that individuals can learn to associate a face with the later occurrence of a shock, even if they are unable to perceive the face. We used a novel application of magnetoencephalography (MEG) to non-invasively record neural activity from the amygdala, which is known to be important for fear learning. We demonstrate rapid (∼170-200 ms) amygdala responses during the stimulus free period between the face and the shock. These results suggest that unperceived faces can serve as signals for impending threat, and that rapid, automatic activation of the amygdala contributes to this process. In addition, we describe a methodology that can be applied in the future to study neural activity with MEG in other subcortical structures.
|
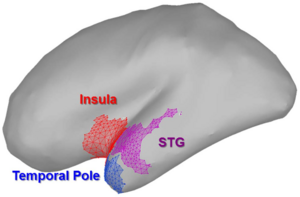 Regions identified as potentially contributing to signal observed in the amygdala. We used a rigorous and unbiased approach to identify potential sources of contamination. Of all the regions sampled, these are the only regions to potentially show evidence of gamma oscillations at ,170 ms. Therefore they were subjected to further analysis. We used 3D Slicer to create the surface models of the cortex, amygdala, and hippocampus. |
BNST Neurocircuitry in Humans
|
Publication: Neuroimage. 2014 May 1;91:311-23. PMID: 24444996 | PDF Authors: Avery SN, Clauss JA, Winder DG, Woodward N, Heckers S, Blackford JU. Institution: Vanderbilt Brain Institute, Vanderbilt University, Nashville, TN, USA. Background/Purpose: Anxiety and addiction disorders are two of the most common mental disorders in the United States, and are typically chronic, disabling, and comorbid. Emerging evidence suggests the bed nucleus of the stria terminalis (BNST) mediates both anxiety and addiction through connections with other brain regions, including the amygdala and nucleus accumbens. Although BNST structural connections have been identified in rodents and a limited number of structural connections have been verified in non-human primates, BNST connections have yet to be described in humans. Neuroimaging is a powerful tool for identifying structural and functional circuits in vivo. In this study, we examined BNST structural and functional connectivity in a large sample of humans. The BNST showed structural and functional connections with multiple subcortical regions, including limbic, thalamic, and basal ganglia structures, confirming structural findings in rodents. We describe two novel connections in the human brain that have not been previously reported in rodents or non-human primates, including a structural connection with the temporal pole, and a functional connection with the paracingulate gyrus. The findings of this study provide a map of the BNST's structural and functional connectivity across the brain in healthy humans. In large part, the BNST neurocircuitry in humans is similar to the findings from rodents and non-human primates; however, several connections are unique to humans. Future explorations of BNST neurocircuitry in anxiety and addiction disorders have the potential to reveal novel mechanisms underlying these disabling psychiatric illnesses. Funding:
|
 The stria terminalis mask (blue) and BNST mask (red) traced in 3D Slicer are shown on a 3-dimensional template brain (left). The group DTI streamlines map, masked by the stria terminalis mask, is shown in green on a 3-dimensional template brain (middle). Each voxel of the stria terminalis mask overlapped with the group streamlines map, demonstrating that tractography streamlines were coursing through the entire stria terminalis. For reference, a histological section of the stria terminalis is shown (right). |
An Intra-Individual Comparison of MRI, [18F]-FET and [18F]-FLT PET in Patients with High-Grade Gliomas
|
Publication: PLos One. 2014 Apr; 9(4):e95830. PMID: 24759867 | PDF Authors: Nowosielski M, DiFranco MD, Putzer D, Seiz M, Recheis W, Jacobs AH, Stockhammer G, Hutterer M. Institution: Department of Neurology, Innsbruck Medical University, Innsbruck, Austria. Background/Purpose: Intra-individual spatial overlap analysis of tumor volumes assessed by MRI, the amino acid PET tracer [18F]-FET and the nucleoside PET tracer [18F]-FLT in high-grade gliomas (HGG). Methods: MRI, [18F]-FET and [18F]-FLT PET data sets were retrospectively analyzed in 23 HGG patients. Morphologic tumor volumes on MRI (post-contrast T1 (cT1) and T2 images) were calculated using a semi-automatic image segmentation method. Metabolic tumor volumes for [18F]-FET and [18F]-FLT PETs were determined by image segmentation using a threshold-based volume of interest analysis. After co-registration with MRI the morphologic and metabolic tumor volumes were compared on an intra-individual basis in order to estimate spatial overlaps using the Spearman’s rank correlation coefficient and the Mann-Whitney U test. Registration of MRI (cT1 and T2), [18F]-FET and [18F]-FLT PET data sets was performed using the fast rigid registration package in 3D Slicer Version 3.6.3.1.0 [26]. All data were co-registered to MRI cT1 imaging sequence. Results: [18F]-FLT uptake was negative in tumors with no or only moderate contrast enhancement on MRI, detecting only 21 of 23 (91%) HGG. In addition, [18F]-FLT uptake was mainly restricted to cT1 tumor areas on MRI and [18F]-FLT volumes strongly correlated with cT1 volumes (r = 0.841, p,0.001). In contrast, [18F]-FET PET detected 22 of 23 (96%) HGG. [18F]-FET uptake beyond areas of cT1 was found in 61% of cases and [18F]-FET volumes showed only a moderate correlation with cT1 volumes (r = 0.573, p,0.001). Metabolic tumor volumes beyond cT1 tumor areas were significantly larger for [18F]-FET compared to [18F]-FLT tracer uptake (8.3 vs. 2.7 cm3, p,0.001). Conclusion: In HGG [18F]-FET but not [18F]-FLT PET was able to detect metabolic active tumor tissue beyond contrast enhancing tumor on MRI. In contrast to [18F]-FET, blood-brain barrier breakdown seems to be a prerequisite for [18F]-FLT tracer uptake. Funding:
|
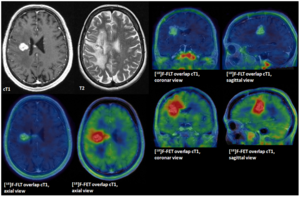 [18F]-FET tracer uptake independent from contrast enhancement on MRI, overlap. GBM WHO IV at 2nd tumor recurrence. Contrast enhanced T1 sequences (cT1) tumor volume 5.4 cm3, metabolically active tumor volumes for [18F]-FET 17.58 cm3 and [18F]-FLT of 3.9 cm3. Overlap analysis detected a [18F]-FET volume of 9.2 cm3 beyond the borders of cT1. |
The Swallow Tail Appearance of the Healthy Nigrosome – A New Accurate Test of Parkinson’s Disease: A Case- Control and Retrospective Cross-Sectional MRI Study at 3T
|
Publication: PLos One 2014 Apr; 9(4):e93814. PMID: 24710392 | PDF Authors: Schwarz ST, Afzal M, Morgan PS, Bajaj N, Gowland PA, Auer DP. Institution: Stroke Trials Unit, Division of Clinical Neurosciences, School of Medicine, University of Nottingham, Nottingham, UK. Background/Purpose: There is no well-established in vivo marker of nigral degeneration in Parkinson’s disease (PD). An ideal imaging marker would directly mirror the loss of substantia nigra dopaminergic neurones, which is most prominent in sub-regions called nigrosomes. High-resolution, iron-sensitive, magnetic resonance imaging (MRI) at 7T allows direct nigrosome-1 visualization in healthy people but not in PD. Here, we investigated the feasibility of nigrosome-1 detection using 3T - susceptibility- weighted (SWI) MRI and the diagnostic accuracy that can be achieved for diagnosing PD in a clinical population. 114 high- resolution 3T – SWI-scans were reviewed consisting of a prospective case-control study in 19 subjects (10 PD, 9 controls) and a retrospective cross-sectional study in 95 consecutive patients undergoing routine clinical SWI-scans (.50 years, 9 PD, 81 non-PD, 5 non-diagnostic studies excluded). Two raters independently classified subjects into PD and non-PD according to absence or presence of nigrosome-1, followed by consensus reading. Diagnostic accuracy was assessed against clinical diagnosis as gold standard. Absolute inter- and intra-rater agreement was $94% (kappa$0.82, p,0.001). In the prospective study 8/9 control and 8/10 PD; and in the retrospective study 77/81 non-PD and all 9 PD subjects were correctly classified. Diagnostic accuracy of the retrospective cohort was: sensitivity 100%, specificity 95%, NPV 1, PPV 0.69 and accuracy 96% which dropped to 91% when including non-diagnostic scans (‘intent to diagnose’). The healthy nigrosome-1 can be readily depicted on high-resolution 3T - SWI giving rise to a ‘swallow tail’ appearance of the dorsolateral substantia nigra, and this feature is lost in PD. Visual radiological assessment yielded a high diagnostic accuracy for PD vs. an unselected clinical control population. Assessing the substantia nigra on SWI for the typical ‘swallow tail’ appearance has potential to become a new and easy applicable 3T MRI diagnostic tool for nigral degeneration in PD. Funding:
|
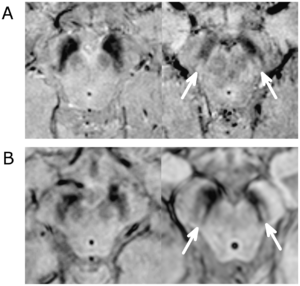 SWI MRI in PD and Non-PD patients. A. High resolution SWI MRI (3D gradient echo EPI, magnitude image) of a PD patient (left, 60 years, female, UPDRS: 53, HY score 3, nigrosome-1 absent bilaterally) and a control (right, 61 years, female, nigrosome-1 present bilaterally). B. Clinical high resolution 3D-T2*/SWI MRI (Philips ‘PRESTO’ sequence), of a PD patient (left, 58 years old, male, nigrosome-1 absent bilaterally) and a non-PD patient (right, 70 years old, female, diagnosed with an aneurysmal subarachnoid haemorrhage, nigrosome-1 present bilaterally). The magnitude images were reviewed in multiple planes using 3D Slicer or a locally developed image viewing and analysis software. |
Clinical and Computed Tomographic Predictors of Chronic Bronchitis in COPD: A Cross Sectional Analysis of the COPDGene Study
|
Publication: Respir Res. 2014 Apr 27;15(1):52. PMID: 24766722 | PDF Authors: Kim V, Davey A, Comellas AP, Han MK, Washko G, Martinez CH, Lynch D, Lee JH, Silverman EK, Crapo JD, Make BJ, Criner GJ. Institution: Temple University School of Medicine, Philadelphia, PA, USA. Background/Purpose: Chronic bronchitis (CB) has been related to poor outcomes in Chronic Obstructive Pulmonary Disease (COPD). From a clinical standpoint, we have shown that subjects with CB in a group with moderate to severe airflow obstruction were younger, more likely to be current smokers, male, Caucasian, had worse health related quality of life, more dyspnea, and increased exacerbation history compared to those without CB. We sought to further refine our clinical characterization of chronic bronchitics in a larger cohort and analyze the CT correlates of CB in COPD subjects. We hypothesized that COPD patients with CB would have thicker airways and a greater history of smoking, acute bronchitis, allergic rhinitis, and occupational exposures compared to those without CB. Methods: We divided 2703 GOLD 1-4 subjects in the Genetic Epidemiology of COPD (COPDGene(R)) Study into two groups based on symptoms: chronic bronchitis (CB+, n = 663, 24.5%) and no chronic bronchitis (CB-, n = 2040, 75.5%). Subjects underwent extensive clinical characterization, and quantitative CT analysis to calculate mean wall area percent (WA%) of 6 segmental airways was performed using VIDA PW2. Square roots of the wall areas of bronchi with internal perimeters 10 mm and 15 mm (Pi10 and Pi15, respectively),%emphysema,%gas trapping, were calculated using 3D Slicer. Results: There were no differences in%emphysema (11.4 ± 12.0 vs. 12.0 ± 12.6%, p = 0.347) or%gas trapping (35.3 ± 21.2 vs. 36.3 ± 20.6%, p = 0.272) between groups. Mean segmental WA% (63.0 ± 3.2 vs. 62.0 ± 3.1%, p < 0.0001), Pi10 (3.72 ± 0.15 vs. 3.69 ± 0.14 mm, p < 0.0001), and Pi15 (5.24 ± 0.22 vs. 5.17 ± 0.20, p < 0.0001) were greater in the CB + group. Greater percentages of gastroesophageal reflux, allergic rhinitis, histories of asthma and acute bronchitis, exposures to dusts and occupational exposures, and current smokers were seen in the CB + group. In multivariate binomial logistic regression, male gender, Caucasian race, a lower FEV1%, allergic rhinitis, history of acute bronchitis, current smoking, and increased airway wall thickness increased odds for having CB. Conclusion: Histories of asthma, allergic rhinitis, acute bronchitis, current smoking, a lower FEV1%, Caucasian race, male gender, and increased airway wall thickness are associated with CB. These data provide clinical and radiologic correlations to the clinical phenotype of CB. Funding:
|
Faceted Visualization of Three Dimensional Neuroanatomy by Combining Ontology with Faceted Search
|
Publication: Neuroinformatics. 2014 Apr;12(2):245-59. PMID: 24006207 | PDF Authors: Veeraraghavan H, Miller JV. Institution: Memorial Sloan-Kettering Cancer Center, New York, NY, USA. Background/Purpose: In this work, we present a faceted-search based approach for visualization of anatomy by combining a three dimensional digital atlas with an anatomy ontology. Specifically, our approach provides a drill-down search interface that exposes the relevant pieces of information (obtained by searching the ontology) for a user query. Hence, the user can produce visualizations starting with minimally specified queries. Furthermore, by automatically translating the user queries into the controlled terminology our approach eliminates the need for the user to use controlled terminology. We demonstrate the scalability of our approach using an abdominal atlas and the same ontology. We implemented our visualization tool on the open-source 3D Slicer software. We present results of our visualization approach by combining a modified Foundational Model of Anatomy (FMA) ontology with the Surgical Planning Laboratory (SPL) Brain 3D digital atlas, and geometric models specific to patients computed using the SPL brain tumor dataset. Funding:
|
An ITK Implementation of a Physics-based Non-rigid Registration Method for Brain Deformation in Image-guided Neurosurgery
|
Publication: Front Neuroinform. 2014 Apr 7;8:33. PMID: 24778613 | PDF Authors: Liu Y, Kot A, Drakopoulos F, Yao C, Fedorov A, Enquobahrie A, Clatz O, Chrisochoides NP. Institution: CRTC Lab and Computer Science, Old Dominion University, Norfolk, VA, USA. Background/Purpose: As part of the ITK v4 project efforts, we have developed ITK filters for physics-based non-rigid registration (PBNRR), which satisfies the following requirements: account for tissue properties in the registration, improve accuracy compared to rigid registration, and reduce execution time using GPU and multi-core accelerators. The implementation has three main components: (1) Feature Point Selection, (2) Block Matching (mapped to both multi-core and GPU processors), and (3) a Robust Finite Element Solver. The use of multi-core and GPU accelerators in ITK v4 provides substantial performance improvements. For example, for the non-rigid registration of brain MRIs, the performance of the block matching filter on average is about 10 times faster when 12 hyperthreaded multi-cores are used and about 83 times faster when the NVIDIA Tesla GPU is used in Dell Workstation. Funding:
|
Morphological Parameters Associated with Ruptured Posterior Communicating Aneurysms
|
Publication: PLoS One. 2014 Apr;9(4):e94837. PMID: 24733151 | PDF Authors: Ho A, Lin N, Charoenvimolphan N, Stanley M, Frerichs KU, Day AL, Du R. Institution: Department of Neurosurgery, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: The rupture risk of unruptured intracranial aneurysms is known to be dependent on the size of the aneurysm. However, the association of morphological characteristics with ruptured aneurysms has not been established in a systematic and location specific manner for the most common aneurysm locations. We evaluated posterior communicating artery (PCoA) aneurysms for morphological parameters associated with aneurysm rupture in that location. CT angiograms were evaluated to generate 3-D models of the aneurysms and surrounding vasculature. Univariate and multivariate analyses were performed to evaluate morphological parameters including aneurysm volume, aspect ratio, size ratio, distance to ICA bifurcation, aneurysm angle, vessel angles, flow angles, and vessel-to-vessel angles. From 2005-2012, 148 PCoA aneurysms were treated in a single institution. Preoperative CTAs from 63 patients (40 ruptured, 23 unruptured) were available and analyzed. Multivariate logistic regression revealed that smaller volume (p = 0.011), larger aneurysm neck diameter (0.048), and shorter ICA bifurcation to aneurysm distance (p = 0.005) were the most strongly associated with aneurysm rupture after adjusting for all other clinical and morphological variables. Multivariate subgroup analysis for patients with visualized PCoA demonstrated that larger neck diameter (p = 0.018) and shorter ICA bifurcation to aneurysm distance (p = 0.011) were significantly associated with rupture. Intracerebral hemorrhage was associated with smaller volume, larger maximum height, and smaller aneurysm angle, in addition to lateral projection, male sex, and lack of hypertension. We found that shorter ICA bifurcation to aneurysm distance is significantly associated with PCoA aneurysm rupture. This is a new physically intuitive parameter that can be measured easily and therefore be readily applied in clinical practice to aid in the evaluation of patients with PCoA aneurysms.
|
 3D model of PCoA aneurysm depicting angular variables of the surrounding vasculature. There were three vessel-to-vessel angles measured. The ICA1 to ICA2 angle refers to the angle between the distal ICA (ICA2) and the proximal ICA (ICA1). The ICA1 to PCoA angle refers to the angle formed between the proximal ICA (ICA1) and PCoA. We utilized 3D Slicer, an open source, multi-platform visualization and image analysis software. |
Computational Modelling of Emboli Travel Trajectories in Cerebral Arteries: Influence of Microembolic Particle Size and Density
|
Publication: Biomech Model Mechanobiol. 2014 Apr;13(2):289-302. PMID: 24585077 | PDF Authors: Fabbri D, Long Q, Das S, Pinelli M. Institution: Brunel Institute for Bioengineering, Brunel University, Uxbridge, UK. Background/Purpose: Ischaemic stroke is responsible for up to 80 % of stroke cases. Prevention of the reoccurrence of ischaemic attack or stroke for patients who survived the first symptoms is the major treatment target. Accurate diagnosis of the emboli source for a specific infarction lesion is very important for a better treatment for the patient. However, due to the complex blood flow patterns in the cerebral arterial network, little is known so far of the embolic particle flow trajectory and its behavior in such a complex flow field. The present study aims to study the trajectories of embolic particles released from carotid arteries and basilar artery in a cerebral arterial network and the influence of particle size, mass and release location to the particle distributions, by computational modeling. The cerebral arterial network model, which includes major arteries in the circle of Willis and several generations of branches from them, was generated from MRI images. Particles with diameters of 200, 500 and 800 μm and densities of 800, 1,030 and 1,300 kg/m3 were released in the vessel’s central and near-wall regions. A fully coupled scheme of particle and blood flow in a computational fluid dynamics software ANASYS CFX 13 was used in the simulations. The results show that heavy particles (density large than blood or a diameter larger than 500 μm ) normally have small travel speeds in arteries; larger or lighter embolic particles are more likely to travel to large branches in cerebral arteries. In certain cases, all large particles go to the middle cerebral arteries; large particles with higher travel speeds in large arteries are likely to travel at more complex and tortuous trajectories; emboli raised from the basilar artery will only exit the model from branches of basilar artery and posterior cerebral arteries. A modified Circle of Willis configuration can have significant influence on particle distributions. The local branch patterns of internal carotid artery to middle cerebral artery and anterior communicating artery can have large impact on such distributions.
|
 3D surface rendering of the cerebral arterial network. 3D Slicer was used for image processing and the 3D reconstruction. |
Adaptive Distance Metric Learning for Diffusion Tensor Image Segmentation
|
Publication: PLoSOne 2014 Mar; 9(3):e92069. PMID: 24651858 | PDF Authors: Kong Y, Wang D, Shi L, Hui SC, Chu WC. Institution: Department of Imaging and Interventional Radiology, The Chinese University of Hong Kong, Shatin, New Territories, Hong Kong, China. Background/Purpose: High quality segmentation of diffusion tensor images (DTI) is of key interest in biomedical research and clinical application. In previous studies, most efforts have been made to construct predefined metrics for different DTI segmentation tasks. These methods require adequate prior knowledge and tuning parameters. To overcome these disadvantages, we proposed to automatically learn an adaptive distance metric by a graph based semi-supervised learning model for DTI segmentation. An original discriminative distance vector was first formulated by combining both geometry and orientation distances derived from diffusion tensors. The kernel metric over the original distance and labels of all voxels were then simultaneously optimized in a graph based semi-supervised learning approach. Finally, the optimization task was efficiently solved with an iterative gradient descent method to achieve the optimal solution. With our approach, an adaptive distance metric could be available for each specific segmentation task. Experiments on synthetic and real brain DTI datasets were performed to demonstrate the effectiveness and robustness of the proposed distance metric learning approach. The performance of our approach was compared with three classical metrics in the graph based semi-supervised learning framework. Funding:
|
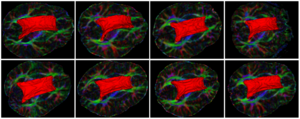 Surfaces of the corpus callosum segmentation results from another 8 datasets using our proposed approach. With the help of 3D Slicer tool, we visualized the 3D surfaces of the manual segmentation. |
Multiple White Matter Volume Reductions in Patients with Panic Disorder: Relationships between Orbitofrontal Gyrus Volume and Symptom Severity and Social Dysfunction
|
Publication: PLoS One. 2014 Mar 24;9(3):e92862. PMID: 24663245| PDF Authors: Konishi J, Asami T, Hayano F, Yoshimi A, Hayasaka S, Fukushima H, Whitford TJ, Inoue T, Hirayasu Y. Institution: Department of Psychiatry, Graduate School of Medicine, Yokohama City University, Yokohama, Japan. Background/Purpose: Numerous brain regions are believed to be involved in the neuropathology of panic disorder (PD) including fronto-limbic regions, thalamus, brain stem, and cerebellum. However, while several previous studies have demonstrated volumetric gray matter reductions in these brain regions, there have been no studies evaluating volumetric white matter changes in the fiber bundles connecting these regions. In addition, although patients with PD typically exhibit social, interpersonal and occupational dysfunction, the neuropathologies underlying these dysfunctions remain unclear. A voxel-based morphometry study was conducted to evaluate differences in regional white matter volume between 40 patients with PD and 40 healthy control subjects (HC). Correlation analyses were performed between the regional white matter volumes and patients' scores on the Panic Disorder Severity Scale (PDSS) and the Global Assessment of Functioning (GAF). Patients with PD demonstrated significant volumetric reductions in widespread white matter regions including fronto-limbic, thalamo-cortical and cerebellar pathways (p<0.05, FDR corrected). Furthermore, there was a significant negative relationship between right orbitofrontal gyrus (OFG) white matter volume and the severity of patients' clinical symptoms, as assessed with the PDSS. A significant positive relationship was also observed between patients' right OFG volumes and their scores on the GAF. Our results suggest that volumetric reductions in widespread white matter regions may play an important role in the pathology of PD. In particular, our results suggest that structural white matter abnormalities in the right OFG may contribute to the social, personal and occupational dysfunction typically experienced by patients with PD. Funding:
|
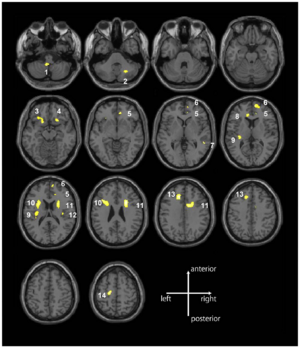 White matter volume reductions in the patients with panic disorder compared with the healthy control subjects. The patients with panic disorder had significant volume reductions in 14 distinct white matter regions (clusters) compared with the healthy control subjects (p,.05, FDR-corrected). The 14 white matter regions included fronto-limbic regions (bilateral OFG, right superior frontal gyrus, left precentral gyrus, bilateral cingulum, and insula), thalamo-cortical pathways (anterior and superior corona radiata), right superior and middle temporal gyrus, and the cerebellum. The gray-scale image was parcellated into each cluster using 3D Slicer. |
Using Stress MRI to Analyze the 3D Changes in Apical Ligament Geometry from Rest to Maximal Valsalva: A Pilot Study
|
Publication: Int Urogynecol J. 2014 Feb;25(2):197-203. PMID: 24008367 | PDF Authors: Luo J, Betschart C, Chen L, Ashton-Miller JA, Delancey JO. Institution: Pelvic Floor Research Group, University of Michigan, Ann Arbor, MI, USA. Background/Purpose: A method was developed using 3D stress magnetic resonance imaging (MRI) and was piloted to test hypotheses concerning changes in apical ligament lengths and lines of action from rest to maximal Valsalva. Methods: Ten women with (cases) and ten without (controls) pelvic organ prolapse (POP) were selected from an ongoing case-control study. Supine, multiplanar stress MRI was performed at rest and at maximal Valsalva and was imported into 3D Slicer v.3.4.1 and aligned. The 3D reconstructions of the uterus and vagina, cardinal ligament (CL), deep uterosacral ligament (USLd), and pelvic bones were created. Ligament length and orientation were then measured. Results: Adequate ligament representations were possible in all 20 study participants. When cases were compared with controls, the curve length of the CL at rest was 71 ±16 mm vs. 59 ± 9 mm (p = 0.051), and the USLd was 38 ± 16 mm vs. 36 ± 11 mm (p = 0.797). Similarly, the increase in CL length from rest to strain was 30 ± 16 mm vs. 15 ± 9 mm (p = 0.033), and USLd was 15 ± 12 mm vs. 7 ± 4 mm (p = 0.094). Likewise, the change in USLd angle was significantly different from CL (p < 0.001). Conclusion: This technique allows quantification of 3D geometry at rest and at strain. In our pilot sample, at maximal Valsalva, CL elongation was greater in cases than controls, whereas USLd was not; CL also exhibited greater changes in ligament length, and USLd exhibited greater changes in ligament inclination angle. Funding:
|
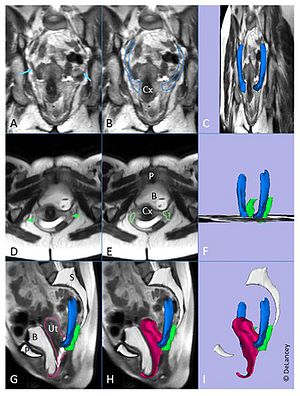 Creating the 3D model: Coronal magnetic resonance image (MRI) showing the cardinal ligament (a; blue arrow) and with outline (b). Model of cardinal ligament (c, blue) shown in slightly skewed coronal image. Axial image showing the deep uterosacral ligament (d; green arrow) and with outline (e). Model of deep uterosacral ligament f; green) shown in the same view angle as (c). Midsagittal image with outline (g) and 3D model (h) of uterus and vagina. Model without image (i) shown in same view angle as (c). Cx cervix, P pubic symphysis, B bladder, Ut uterus, V vagina, S sacrum. |
Scanning Fast and Slow: Current Limitations of 3 Tesla Functional MRI and Future Potential
|
Publication: Frontiersin Physics 2014 Feb;2(1):1-8. | PDF Authors: Boubela RN, Kalcher K, Nasel C, Moser E. Institution: Center for Medical Physics and Biomedical Engineering, Medical University of Vienna, Vienna, Austria. Background/Purpose: Functional MRI at 3T has become a workhorse for the neurosciences, e.g., neurology, psychology, and psychiatry, enabling non-invasive investigation of brain function and connectivity. However, BOLD-based fMRI is a rather indirect measure of brain function, confounded by physiology related signals, e.g., head or brain motion, brain pulsation, blood flow, intermixed with susceptibility differences close or distant to the region of neuronal activity. Even though a plethora of preprocessing strategies have been published to address these confounds, their efficiency is still under discussion. In particular, physiological signal fluctuations closely related to brain supply may mask BOLD signal changes related to “true” neuronal activation. Here we explore recent technical and methodological advancements aimed at disentangling the various components, employing fast multiband vs. standard EPI, in combination with fast temporal ICA. Our preliminary results indicate that fast (TR <0.5 s) scanning may help to identify and eliminate physiologic components, increasing tSNR and functional contrast. In addition, biological variability can be studied and task performance better correlated to other measures. This should increase specificity and reliability in fMRI studies. Furthermore, physiological signal changes during scanning may then be recognized as a source of information rather than a nuisance. As we are currently still undersampling the complexity of the brain, even at a rather coarse macroscopic level, we should be very cautious in the interpretation of neuroscientific findings, in particular when comparing different groups (e.g., age, sex, medication, pathology, etc.). From a technical point of view our goal should be to sample brain activity at layer specific resolution with low TR, covering as much of the brain as possible without violating SAR limits. We hope to stimulate discussion toward a better understanding and a more quantitative use of fMRI. Funding:
|
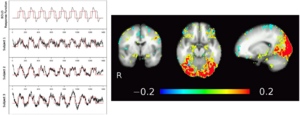 Temporal ICA of low TR, multiband EPI fMRI data from three subjects. Using a strong task (image matching paradigm, block design shown in red). tICA identifies the activation map in the visual cortex but also adjacent to the amygdalae and at the fronto-basis, corresponding to task related time courses as well as strong pulsations (high frequency noise). Note also the major draining vein (V. parieto-occipitalis interna connecting to V. basalis Rosenthal) following medially the temporal lobe next to the amygdalae. The three dimensional visualization of the veins as measured with SWI was done in 3D Slicer. |
Molecular Drivers and Cortical Spread of Lateral Entorhinal Cortex Dysfunction in Preclinical Alzheimer’s Disease
|
Publication: Nat Neurosci. 2014 Feb;17(2):304-11. PMID: 24362760 | PDF Authors: Khan UA, Liu L, Provenzano FA, Berman DE, Profaci CP, Sloan R, Mayeux R, Duff KE, Small SA. Institution: Taub Institute for Research on Alzheimer's Disease and the Aging Brain, Columbia University College of Physicians and Surgeons, New York, NY, USA. Background/Purpose: The entorhinal cortex has been implicated in the early stages of Alzheimer's disease, which is characterized by changes in the tau protein and in the cleaved fragments of the amyloid precursor protein (APP). We used a high-resolution functional magnetic resonance imaging (fMRI) variant that can map metabolic defects in patients and mouse models to address basic questions about entorhinal cortex pathophysiology. The entorhinal cortex is divided into functionally distinct regions, the medial entorhinal cortex (MEC) and the lateral entorhinal cortex (LEC), and we exploited the high-resolution capabilities of the fMRI variant to ask whether either of them was affected in patients with preclinical Alzheimer's disease. Next, we imaged three mouse models of disease to clarify how tau and APP relate to entorhinal cortex dysfunction and to determine whether the entorhinal cortex can act as a source of dysfunction observed in other cortical areas. We found that the LEC was affected in preclinical disease, that LEC dysfunction could spread to the parietal cortex during preclinical disease and that APP expression potentiated tau toxicity in driving LEC dysfunction, thereby helping to explain regional vulnerability in the disease. Funding:
|
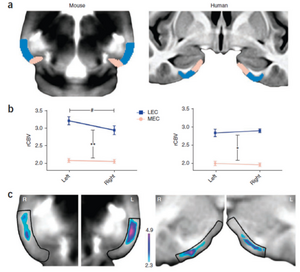 The LEC shows evidence of high metabolism in young unaffected individuals. (a) The entorhinal cortex was segmented into the MEC (pink) and the LEC (blue) in template brains of young wild-type mice (left) and young healthy human subjects (right). (b) In young wild-type mice (left), the LEC (blue) was found to have higher CBV values than the MEC (pink) (**F1,34 = 475.176, P < 0.001), and the left LEC was found to have higher CBV values than the right LEC (#F1,34 = 6.680, P = 0.01). In young healthy human subjects (right), the LEC (blue) was found to have higher CBV values than the MEC (pink) (*F1,34 = 706.199, P <0.001). Data are presented as mean ± s.e.m. (c) Thresholded mean CBV maps in young wild-type mice (left) revealed that the CBV was higher in the LEC than the MEC, with the left LEC showing the highest CBV. Mean CBV maps in young healthy human subjects (right) revealed that the LEC had a higher CBV than the MEC. This image map was thresholded above the mean intensity of the MEC and color-coded using 3D Slicer. |
Retrosigmoid Implantation of an Active Bone Conduction Stimulator in a Patient with Chronic Otitis Media
|
Publication: Auris Nasus Larynx. 2014 Feb;41(1):84-7. PMID: 23722197 Authors: Lassaletta L, Sanchez-Cuadrado I, Muñoz E, Gavilan J. Institution: Department of Otolaryngology, "La Paz" University Hospital, IdiPaz Research Institute, Madrid, Spain. Background/Purpose: Percutaneous bone conduction implants are widely used in patients with conductive and mixed hearing loss with no benefit from conventional air conduction hearing aids. These devices have several complications including skin reaction, wound infection, growth of skin over the abutment, and implant extrusion. We describe a case of a transcutaneous bone conduction implantation (Bonebridge, Med-el) in a patient with conductive hearing loss due to chronic otitis media. Surgical planification was performed with the software 3D Slicer 4.1. According to this program, the implant transductor was positioned in the retrosigmoid area. Aided thresholds demonstrate a significant benefit, with an improvement from 68dB to 25dB. Speech discrimination scores improved 35dB. The patient is very happy and uses her device daily. The Bonebridge implant is a promising transcutaneous bone conduction implant for patients with conductive hearing loss. Retrosigmoid implantation may be useful in cases with mastoid pathology or previous surgery.
|
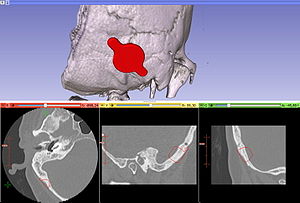 Top 3D Slicer reconstruction showing the planned location of the transductor (red) in the right retrosigmoid area. The theoretical position and area of dura compression (red figure) is shown in the axial (bottom, left), coronal (bottom, middle) and sagital (bottom, right) CT scan images. Note the planned position of one of the screws in the coronal view. |
Evaluation of Prostate Segmentation Algorithms for MRI: The PROMISE12 Challenge
|
Publication: Med Image Anal. 2014 Feb;18(2):359-73. PMID: 24418598 | PDF Authors: Litjens G, Toth R, van de Ven W, Hoeks C, Kerkstra S, van Ginneken B, Vincent G, Guillard G, Birbeck N, Zhang J, Strand R, Malmberg F, Ou Y, Davatzikos C, Kirschner M, Jung F, Yuan J, Qiu W, Gao Q, Edwards PE, Maan B, van der Heijden F, Ghose S, Mitra J, Dowling J, Barratt D, Huisman H, Madabhushi A. Institution: Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands. Background/Purpose: Prostate MRI image segmentation has been an area of intense research due to the increased use of MRI as a modality for the clinical workup of prostate cancer. Segmentation is useful for various tasks, e.g. to accurately localize prostate boundaries for radiotherapy or to initialize multi-modal registration algorithms. In the past, it has been difficult for research groups to evaluate prostate segmentation algorithms on multi-center, multi-vendor and multi-protocol data. Especially because we are dealing with MR images, image appearance, resolution and the presence of artifacts are affected by differences in scanners and/or protocols, which in turn can have a large influence on algorithm accuracy. The Prostate MR Image Segmentation (PROMISE12) challenge was setup to allow a fair and meaningful comparison of segmentation methods on the basis of performance and robustness. In this work we will discuss the initial results of the online PROMISE12 challenge, and the results obtained in the live challenge workshop hosted by the MICCAI2012 conference. In the challenge, 100 prostate MR cases from 4 different centers were included, with differences in scanner manufacturer, field strength and protocol. A total of 11 teams from academic research groups and industry participated. Algorithms showed a wide variety in methods and implementation, including active appearance models, atlas registration and level sets. Evaluation was performed using boundary and volume based metrics which were combined into a single score relating the metrics to human expert performance. The winners of the challenge where the algorithms by teams Imorphics and ScrAutoProstate, with scores of 85.72 and 84.29 overall. Both algorithms where significantly better than all other algorithms in the challenge (p<0.05) and had an efficient implementation with a run time of 8min and 3s per case respectively. Overall, active appearance model based approaches seemed to outperform other approaches like multi-atlas registration, both on accuracy and computation time. Although average algorithm performance was good to excellent and the Imorphics algorithm outperformed the second observer on average, we showed that algorithm combination might lead to further improvement, indicating that optimal performance for prostate segmentation is not yet obtained. Funding:
|
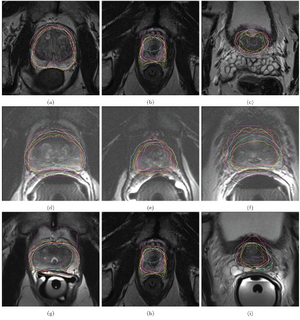 Qualitative segmentation results of case 3 (a, b, c), case 10 (d, e, f) and case 25 (g, h, i) at the center (a, d, g), apex (b, e, h) and base (c, f, i) of the prostate. Case 3 had the best, case 10 reasonable and case 25 the worst algorithm scores on average. The different colors indicate the results for the different teams. Contouring was performed by annotating spline-connected points in either 3D Slicer or MeVisLab. |
The Detection and Visualization of Brain Tumors on T2-Weighted MRI Images using Multiparameter Feature Blocks
|
Publication: International Journal of Emerging Technology and Advanced Engineering. 2014 Feb; 4(2):127-31. | PDF Authors: Wakchaure SL, Ghuge DG, Musale DS. Institution: Department of Computer Science, Indore Institute of Science and Technology, Madhya Pradesh, India. Background/Purpose: The main topic of this paper is to segment brain tumors, their components (edema and necrosis) and internal structures of the brain in 3D MR images. For tumor segmentation we propose a framework that is a combination of region-based and boundary-based paradigms. In this framework, segment the brain using a method adapted for pathological cases and extract some global information on the tumor by symmetry based histogram analysis. The objective of this paper is to present an analytical method to detect lesions or tumors in digitized medical images for 3D visualization. This research opens a new window in the field of image processing by 3D Volume Representation of tumor through the use of Magnetic Resonant Imaging and an integrated software tool 3D Slicer. The authors developed a tumor detection method using three parameters; edge (E), gray (G), and contrast (H) values. The method proposed here studied the EGH parameters in a supervised block of input images. These feature blocks were compared with standardized parameters (derived from normal template block) to detect abnormal occurrences, e.g. image block which contain lesions or tumor cells. The proposed method shows more precision among the others. Processing time is less. This will help the physicians in analyzing the brain tumors accurately and efficiently. |
Spinal Curvature Measurement by Tracked Ultrasound Snapshots
|
Publication: Ultrasound Med Biol. 2014 Feb;40(2):447-54. PMID: 24268452 Authors: Ungi T, King F, Kempston M, Keri Z, Lasso A, Mousavi P, Rudan J, Borschneck DP, Fichtinger G. Institution: Laboratory for Percutaneous Surgery, School of Computing, Queen's University, Kingston, ON, Canada. Background/Purpose: Monitoring spinal curvature in adolescent kyphoscoliosis requires regular radiographic examinations; however, the applied ionizing radiation increases the risk of cancer. Ultrasound imaging is favored over radiography because it does not emit ionizing radiation. Therefore, we tested an ultrasound system for spinal curvature measurement, with the help of spatial tracking of the ultrasound transducer. Tracked ultrasound was used to localize vertebral transverse processes as landmarks along the spine to measure curvature angles. The method was tested in two scoliotic spine models by localizing the same landmarks using both ultrasound and radiographic imaging and comparing the angles obtained. A close correlation was found between tracked ultrasound and radiographic curvature measurements. Differences between results of the two methods were 1.27 ± 0.84° (average ± SD) in an adult model and 0.96 ± 0.87° in a pediatric model. Our results suggest that tracked ultrasound may become a more tolerable and more accessible alternative to radiographic spine monitoring in adolescent kyphoscoliosis. |
Sequencing Biological and Physical Events Affects Specific Frequency Bands within the Human Premotor Cortex: An Intracerebral EEG Study
|
Publication: PLoS One. 2014 Jan; 9(1): e86384. PMID: 24466067 | PDF Authors: Caruana F, Sartori I,Lo Russo G, Avanzini P. Institution: Brain Center for Social and Motor Cognition, Italian Institute of Technology, Parma, Italy. Background/Purpose: Evidence that the human premotor cortex (PMC) is activated by cognitive functions involving the motor domain is classically explained as the reactivation of a motor program decoupled from its executive functions, and exploited for different purposes by means of a motor simulation. In contrast, the evidence that PMC contributes to the sequencing of non-biological events cannot be explained by the simulationist theory. Here we investigated how motor simulation and event sequencing coexist within the PMC and how these mechanisms interact when both functions are executed. We asked patients with depth electrodes implanted in the PMC to passively observe a randomized arrangement of images depicting biological actions and physical events and, in a second block, to sequence them in the correct order. This task allowed us to disambiguate between the simple observation of actions, their sequencing (recruiting different motor simulation processes), as well as the sequencing of non-biological events (recruiting a sequencer mechanism non-dependant on motor simulation). We analyzed the response of the gamma, alpha and beta frequency bands to evaluate the contribution of each brain rhythm to the observation and sequencing of both biological and non-biological stimuli. We found that motor simulation (biological>physical) and event sequencing (sequencing>observation) differently affect the three investigated frequency bands: motor simulation was reflected on the gamma and, partially, in the beta, but not in the alpha band. In contrast, event sequencing was also reflected on the alpha band.
|
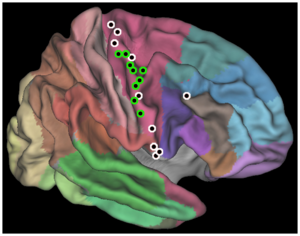 Illustration of the recording sites. Entrance point of the 19 electrodes implanted in the eight patients are plotted on an inflated PALS atlas surface according to their MNI coordinates. Brodmann areas are shown (Caret; see [36]). Green: electrodes with at least one contact showing a significant effect of condition (BIO>PHY) in the gamma band. White: electrodes with no contacts showing a significant effect of condition. Sites are illustrated in the right hemisphere. All entrance point are localized in the precentral gyrus, with the only exception of a rostral electrode, approaching the deep PMC from the BA44. The localization of each of the 107 recording contact was assessed by the coregistration of pre-implantation volumetric brain MRI with post-implantation volumetric brain CT (3D Slicer). |
Regional 3D Superimposition to assess Temporomandibular Joint Condylar Morphology
|
Publication: Dentomaxillofac Radiol. 2014;43(1):20130273. PMID: 24170802 | PDF Authors: Schilling J, Gomes LC, Benavides E, Nguyen T, Paniagua B, Styner M, Boen V, Gonçalves JR, Cevidanes LH. Institution: Department of Periodontics and Oral Medicine, School of Dentistry, University of Michigan, Ann Arbor, MI, USA. Background/Purpose: To investigate the reliability of regional three-dimensional registration and superimposition methods for assessment of temporomandibular joint condylar morphology across subjects and longitudinally. Methods: The sample consisted of cone beam CT scans of 36 patients. The across-subject comparisons included 12 controls, mean age 41.3 ± 12.0 years, and 12 patients with temporomandibular joint osteoarthritis, mean age 41.3 ± 14.7 years. The individual longitudinal assessments included 12 patients with temporomandibular joint osteoarthritis, mean age 37.8 ± 16.7 years, followed up at pre-operative jaw surgery, immediately after and one-year post-operative. Surface models of all condyles were constructed from the cone beam CT scans. Two previously calibrated observers independently performed all registration methods. A landmark-based approach was used for the registration of across-subject condylar models, and temporomandibular joint osteoarthritis vs control group differences were computed with shape analysis. A voxel-based approach was used for registration of longitudinal scans calculated x, y, z degrees of freedom for translation and rotation. Two-way random intraclass correlation coefficients tested the interobserver reliability. Results: Statistically significant differences between the control group and the osteoarthritis group were consistently located on the lateral and medial poles for both observers. The interobserver differences were ≤0.2 mm. For individual longitudinal comparisons, the mean interobserver differences were ≤0.6 mm in translation errors and 1.2° in rotation errors, with excellent reliability (intraclass correlation coefficient >0.75). Conclusion: Condylar registration for across-subjects and longitudinal assessments is reliable and can be used to quantify subtle bony differences in the three-dimensional condylar morphology. Funding:
|
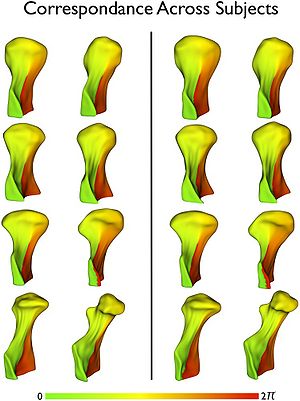 Quality control of the correspondence across 4002 points in the condylar surface models and between observers using parametric color maps. These color maps display one of the two spherical parameters, Phi, which is equivalent to geographical longitude. Eight condyles in the Observer 1 evaluation are shown in the left columns and the same condyles in Observer 2 evaluation are shown in the right columns. Note the consistency of the color maps across all condyles and between observers. |
2013
|
Publication: Clin Orthop Relat Res. 2013 Dec;471(12):4047-55. PMID: 23955194 | PDF Authors: Ungi T, Moult E, Schwab JH, Fichtinger G. Institution: Laboratory for Percutaneous Surgery, School of Computing, Queen's University, Kingston, ON, Canada. Background/Purpose: Computerized navigation improves the accuracy of minimally invasive pedicle screw placement during spine surgery. Such navigation, however, exposes both the patient and the staff to radiation during surgery. To avoid intraoperative exposure to radiation, tracked ultrasound snapshots-ultrasound image frames coupled with corresponding spatial positions-could be used to map preoperatively defined screw plans into the intraoperative coordinate frame. The feasibility of such an approach, however, has not yet been investigated. Questions: Are there vertebral landmarks that can be identified using tracked ultrasound snapshots? Can tracked ultrasound snapshots allow preoperative pedicle screw plans to be accurately mapped-compared with CT-derived pedicle screw plans-into the intraoperative coordinate frame in a simulated setting? Methods: Ultrasound visibility of registration landmarks was checked on volunteers and phantoms. An ultrasound machine with integrated electromagnetic tracking was used for tracked ultrasound acquisition. Registration was performed using 3D Slicer open-source software. Two artificial lumbar spine phantoms were used to evaluate registration accuracy of pedicle screw plans using tracked ultrasound snapshots. Registration accuracy was determined by comparing the ultrasound-derived plans with the CT-derived plans. Results: The four articular processes proved to be identifiable using tracked ultrasound snapshots. Pedicle screw plans were registered to the intraoperative coordinate system using landmarks. The registrations were sufficiently accurate in that none of the registered screw plans intersected the pedicle walls. Registered screw plan positions had an error less than 1.28 ± 1.37 mm (average ± SD) in each direction and an angle difference less than 1.92° ± 1.95° around each axis relative to the CT-derived positions. Conclusion: Registration landmarks could be located using tracked ultrasound snapshots and permitted accurate mapping of pedicle screw plans to the intraoperative coordinate frame in a simulated setting. Clinical Relevance: Tracked ultrasound may allow accurate computer-navigated pedicle screw placement while avoiding ionizing radiation in the operating room; however, further studies that compare this approach with other navigation techniques are needed to confirm the practical use of this new approach.
|
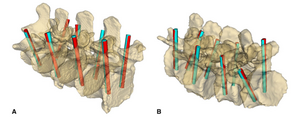 (A) Overview of pedicle screw plan positions as defined in the CT image (blue rods) and as registered using ultrasound snapshots (red rods) in the healthy spine model is shown. (B) Overview of pedicle screw plan positions as defined in the CT image (blue rods) and as registered using ultrasound snapshots (red rods) in the degenerative spine model is shown. Registration was performed using 3D Slicer open-source software. |
Dietary Cholesterol Increases Ventricular Volume and Narrows Cerebrovascular Diameter in a Rabbit Model of Alzheimer's Disease
|
Publication: Neuroscience. 2013 Dec 19;254:61-9. PMID: 24045100 | PDF Authors: Schreurs BG, Smith-Bell CA, Lemieux SK. Institution: Department of Physiology and Pharmacology, and the Blanchette Rockefeller Neurosciences Institute, West Virginia University, Morgantown, WV, USA. Background/Purpose: Using structural magnetic resonance imaging in a clinical scanner at 3.0T, we describe results showing that following 12weeks on a diet of 2% cholesterol, rabbits experience a significant increase in the volume of the third ventricle compared to rabbits on a diet of 0% cholesterol. Using time-of-flight magnetic resonance angiography, we find cholesterol-fed rabbits also experience a decrease in the diameter of a number of cerebral blood vessels including the basilar, posterior communicating, and internal carotid arteries. Taken together, these data confirm that, despite the inability of dietary cholesterol to cross the blood-brain barrier, it does significantly enlarge ventricular volume and decrease cerebrovascular diameter in the rabbit - effects that are also seen in patients with Alzheimer's disease. Using the editing function of 3D Slicer, the ventricles were manually selected using intensity-based threshold painting. The statistics module of 3D Slicer was used for quantification of ventricular volume. Funding:
|
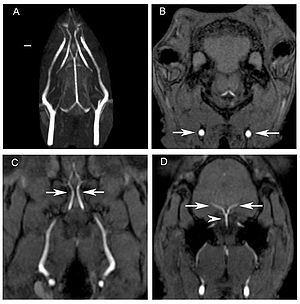 Blood vessels in the heads of rabbits fed different cholesterol or control diets. Sample time-of-flight magnetic resonance imaging images used to measure blood vessel diameters. Panel A shows the maximum intensity projection image of the blood vessels throughout the head of a rabbit. The scale bar is 2 mm. The remaining panels are different axial time-of-flight images showing the common carotid arteries (arrows, B), the internal carotid arteries (arrows, C), and the posterior communicating arteries (arrows, D) and basilar artery (arrow head, D). |
Rapid and Efficient Localization of Depth Electrodes and Cortical Labeling using Free and Open Source Medical Software in Epilepsy Surgery Candidates
|
Publication: Front Neurosci. 2013 Dec 31;7:260. PMID: 24427112 | PDF Authors: Princich JP, Wassermann D, Latini F, Oddo S, Blenkmann AO, Seifer G, Kochen S. Institution: Epilepsy Section, Neurosciences Clinic and Applicated Center, Hospital Ramos Mejia, Universidad de Buenos Aires Buenos Aires, Argentina. Background/Purpose: Depth intracranial electrodes (IEs) placement is one of the most used procedures to identify the epileptogenic zone (EZ) in surgical treatment of drug resistant epilepsy patients, about 20-30% of this population. IEs localization is therefore a critical issue defining the EZ and its relation with eloquent functional areas. That information is then used to target the resective surgery and has great potential to affect outcome. We designed a methodological procedure intended to avoid the need for highly specialized medical resources and reduce time to identify the anatomical location of IEs, during the first instances of intracranial EEG recordings. This workflow is based on established open source software; 3D Slicer and Freesurfer that uses MRI and Post-implant CT fusion for the localization of IEs and its relation with automatic labeled surrounding cortex. To test this hypothesis we assessed the time elapsed between the surgical implantation process and the final anatomical localization of IEs by means of our proposed method compared against traditional visual analysis of raw post-implant imaging in two groups of patients. All IEs were identified in the first 24 H (6-24 H) of implantation using our method in 4 patients of the first group. For the control group; all IEs were identified by experts with an overall time range of 36 h to 3 days using traditional visual analysis. It included (7 patients), 3 patients implanted with IEs and the same 4 patients from the first group. Time to localization was restrained in this group by the specialized personnel and the image quality available. To validate our method; we trained two inexperienced operators to assess the position of IEs contacts on four patients (5 IEs) using the proposed method. We quantified the discrepancies between operators and we also assessed the efficiency of our method to define the EZ comparing the findings against the results of traditional analysis.
|
Reduced Habituation in Patients with Schizophrenia
|
Publication: Schizophr Res. 2013 Dec;151(1-3):124-32 PMID: 24200419 | PDF Authors: Williams LE, Blackford JU, Luksik A, Gauthier I, Heckers S. Institution: Department of Psychiatry, Vanderbilt University, Nashville, TN, USA. Background/Purpose: Neural habituation, the decrease in brain response to repeated stimulation, is a basic form of learning. There is strong evidence for behavioral and physiological habituation deficits in schizophrenia, and one previous study found reduced neural habituation within the hippocampus. However, it is unknown whether neural habituation deficits are specific to faces and limited to the hippocampus. Here we studied habituation of several brain regions in schizophrenia, using both face and object stimuli. Post-scan memory measures were administered to test for a link between hippocampal habituation and memory performance. Methods: During an fMRI scan, 23 patients with schizophrenia and 21 control subjects viewed blocks of a repeated neutral face or neutral object, and blocks of different neutral faces and neutral objects. Habituation in the hippocampus, primary visual cortex and fusiform face area (FFA) was compared between groups. Memory for faces, words, and word pairs was assessed after the scan. Results: Patients showed reduced habituation to faces in the hippocampus and primary visual cortex, but not the FFA. Healthy control subjects exhibited a pattern of hippocampal discrimination that distinguished between repeated and different images for both faces and objects, and schizophrenia patients did not. Hippocampal discrimination was positively correlated with memory for word pairs. Conclusion: Patients with schizophrenia showed reduced habituation of the hippocampus and visual cortex, and a lack of neural discrimination between old and new images in the hippocampus. Hippocampal discrimination correlated with memory performance, suggesting reduced habituation may contribute to the memory deficits commonly observed in schizophrenia. |
 Patients with schizophrenia showed reduced habituation to Repeated faces in the left (k = 34; − 21, −22, −23) and right (k = 13; 18, −37, 4) hippocampus (cluster corrected p-value < .05). Extracting the percent signal change from these clusters shows that while control participants show decreasing hippocampal activity across the run, activity is more sustained for schizophrenia patients. A similar pattern was found in three clusters in the bilateral visual cortex (k = 111, −18, −79, 10; k = 22, 12, −76, 22; k = 19, 24, −97, 7, cluster-corrected p < .05). Percent signal change showed for a representative cluster. In contrast, both controls and schizophrenia patients show robust habituation to Repeated faces within the FFA (a representative single-subject FFA region of interest shown in green). Hippocampal segmentation used a previously established protocol in the 3D Slicer program (version 3.4) |
On the Prospect of Patient-specific Biomechanics without Patient-specific Properties of Tissues
|
Publication: J Mech Behav Biomed Mater. 2013 Nov;27:154-66. PMID: 23491073 | PDF Authors: Miller K, Lu J. Institution: Intelligent Systems for Medicine Laboratory, School of Mechanical and Chemical Engineering, University of Western Australia, Perth, WA, Australia. Background/Purpose: This paper presents main theses of two keynote lectures delivered at Euromech Colloquium "Advanced experimental approaches and inverse problems in tissue biomechanics" held in Saint Etienne in June 2012. We are witnessing an advent of patient-specific biomechanics that will bring in the future personalized treatments to sufferers all over the world. It is the current task of biomechanists to devise methods for clinically-relevant patient-specific modeling. One of the obstacles standing before the biomechanics community is the difficulty in obtaining patient-specific properties of tissues to be used in biomechanical models. We postulate that focusing on reformulating computational mechanics problems in such a way that the results are weakly sensitive to the variation in mechanical properties of simulated continua is more likely to bear fruit in near future. We consider two types of problems: (i) displacement-zero traction problems whose solutions in displacements are weakly sensitive to mechanical properties of the considered continuum; and (ii) problems that are approximately statically determinate and therefore their solutions in stresses are also weakly sensitive to mechanical properties of constituents. We demonstrate that the kinematically loaded biomechanical models of the first type are applicable in the field of image-guided surgery where the current, intraoperative configuration of a soft organ is of critical importance. We show that sac-like membranes, which are prototypes of many thin-walled biological organs, are approximately statically determinate and therefore useful solutions for wall stress can be obtained without the knowledge of the wall's properties. We demonstrate the clinical applicability and effectiveness of the proposed methods using examples from modeling neurosurgery and intracranial aneurysms. Funding:
|
Derivation of Neural Stem Cells from Human Adult Peripheral CD34+ Cells for an Autologous Model of Neuroinflammation
|
Publication: PLoS One. 2013 Nov 26;8(11):e81720 PMID: 24303066 | PDF Authors: Wang T, Choi E, Monaco MC, Campanac E, Medynets M, Do T, Rao P, Johnson KR, Elkahloun AG, Von Geldern G, Johnson T, Subramaniam S, Hoffman D, Major E, Nath A. Institution: Translational Neuroscience Center, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, MD, USA. Background/Purpose: Proinflammatory factors from activated T cells inhibit neurogenesis in adult animal brain and cultured human fetal neural stem cells (NSC). However, the role of inhibition of neurogenesis in human neuroinflammatory diseases is still uncertain because of the difficulty in obtaining adult NSC from patients. Recent developments in cell reprogramming suggest that NSC may be derived directly from adult fibroblasts. We generated NSC from adult human peripheral CD34+ cells by transfecting the cells with Sendai virus constructs containing Sox2, Oct3/4, c-Myc and Klf4. The derived NSC could be differentiated to glial cells and action potential firing neurons. Co-culturing NSC with activated autologous T cells or treatment with recombinant granzyme B caused inhibition of neurogenesis as indicated by decreased NSC proliferation and neuronal differentiation. Thus, we have established a unique autologous in vitro model to study the pathophysiology of neuroinflammatory diseases that has potential for usage in personalized medicine. Features of interest were automatically selected with 3D Slicer using a threshold tool that highlighted features within a specified range of pixel intensity. |
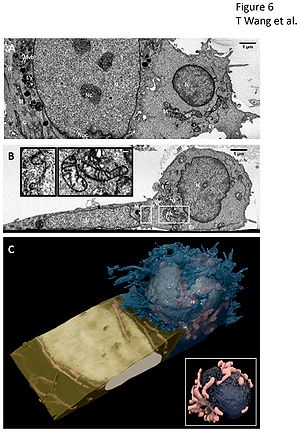 3D imaging of contact between neural stem cell (left) and activated T cell (right) by ion abrasion scanning electron microscopy (IA-SEM). (A, B) Representative, orthogonal 2D images from a 17.57 um x 6.30 um x 8.72 um stack volume show the two cells in direct contact with interlocking cellular membranes in the XZ plane (A) and XY plane (B). The XY plane reveals a localization of Golgi apparatus, vesicles, and mitochondria in the activated T cell near the site of contact. Subcellular organelles are well preserved including nucleus (N), nucleolus (Nc), nuclear pore complexes (Npc), multivesicular bodies (Mvb), lysosome (Ly), mitochondria (M), cytoskeleton (C), intermediate filament (IF), Golgi apparatus (G), vesicles (V), and endoplasmic recticulum (ER). (B, Inset) Expanded view of boxed regions in panel (B) of the interlocking membranes at the cell-cell junction (left) and the T cell mitochondria (right) to illustrate level of detail in images. Scale bars are 100 nm. (C) 3D visualization of the SEM image stack show the activated T cell membrane (blue) engulfing an edge of the neural stem cell membrane (gold). The activated T cell spherical shaped nucleus (ivory), compact mitochondria clusters (pink), and complex membrane protrusions are seen in stark contrast with the neural stem cell flat nucleus (ivory), elongated mitochondria (pink), and smooth cell membrane. (C, Inset) Expanded view of the interior of the T-cell showing the T cell nucleus (navy) is pinched in the center, with the cleft line oriented directly toward the site of contact. Mitochondria (pink) are found clustered along the cleft line. |
Can Transrectal Needle Biopsy be Optimised to Detect Nearly All Prostate Cancer with a Volume of ≥0.5 mL? A Three-dimensional Analysis
|
Publication: BJU Int. 2013 Nov;112(7):898-904. PMID: 23490279| PDF Authors: Kanao K, Eastham JA, Scardino PT, Reuter VE, Fine SW. Institution: Department of Pathology, Urology Service, Memorial Sloan-Kettering Cancer Center, New York, NY, USA. Background/Purpose: Retrospectively analyzed 109 whole-mounted and entirely submitted radical prostatectomy specimens with prostate cancer. All tumors in each prostate were outlined on whole-mount slides and digitally scanned to produce tumor maps. Tumour map images were exported to three-dimensional 3D Slicer software to develop a 3D-prostate cancer model. In all, 20 transrectal biopsy schemes involving two to 40 cores and two to six anteriorly directed biopsy (ADBx) cores (including transition zone, TZ) were simulated, as well as models with various biopsy cutting lengths. Detection rates for tumors of different volumes were determined for the various biopsy simulation schemes. |
Analysis of Morphological Parameters to Differentiate Rupture Status in Anterior Communicating Artery Aneurysms
|
Publication: PLoS One. 2013 Nov 13;8(11):e79635. PMID: 24236149 | PDF Authors: Lin N, Ho A, Charoenvimolphan N, Frerichs KU, Day AL, Du R. Institution: Department of Neurosurgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: In contrast to size, the association of morphological characteristics of intracranial aneurysms with rupture has not been established in a systematic manner. We present an analysis of the morphological variables that are associated with rupture in anterior communicating artery aneurysms to determine site-specific risk variables. One hundred and twenty-four anterior communicating artery aneurysms were treated in a single institution from 2005 to 2010, and CT angiograms (CTAs) or rotational angiography from 79 patients (42 ruptured, 37 unruptured) were analyzed. Vascular imaging was evaluated with 3D Slicer to generate models of the aneurysms and surrounding vasculature. Morphological parameters were examined using univariate and multivariate analysis and included aneurysm volume, aspect ratio, size ratio, distance to bifurcation, aneurysm angle, vessel angle, flow angle, and parent-daughter angle. Multivariate logistic regression revealed that size ratio, flow angle, and parent-daughter angle were associated with aneurysm rupture after adjustment for age, sex, smoking history, and other clinical risk factors. Simple morphological parameters such as size ratio, flow angle, and parent-daughter angle may thus aid in the evaluation of rupture risk of anterior communicating artery aneurysms. Funding:
|
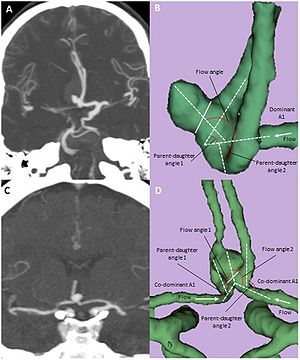 Computed Tomography Angiogram (CTA) and three-dimensional models of anterior communicating aneurysms with a dominant A1 or with co-dominant A1’s.Coronal MIP images are shown for an ruptured AcoA aneurysm with a dominant left A1 (A) and an unruptured AcoA aneurysm with co-dominant A1’s (C). The corresponding 3D reconstructed images from 3D Slicer are shown in B and D with definitions of morphological parameters. Solid line (B and D) indicates aneurysm neck. |
Anatomic and Morphological Evaluation of the Quadriceps Tendon using 3-Dimensional Magnetic Resonance Imaging Reconstruction
|
Publication: Am J Sports Med. 2013 Oct;41(10):2392-9. PMID: 23893419 | PDF Authors: Xerogeanes JW, Mitchell PM, Karasev PA, Kolesov IA, Romine SE. Institution: Department of Orthopaedic Surgery, Emory University School of Medicine, Atlanta, GA, USA. Background/Purpose: The autograft of choice for anterior cruciate ligament (ACL) reconstruction remains controversial. The quadriceps tendon is the least utilized and least studied of the potential autograft options. To determine if the quadriceps tendon has the anatomic characteristics to produce a graft whose length and volume are adequate, reproducible, and predictable when compared with the other commonly used autografts. Study Design: Cross-sectional study; Level of evidence, 3. Methods: Axial proton density magnetic resonance imaging (MRI) scans of 60 skeletally mature patients (30 male and 30 female) were evaluated. Volumetric analysis of 3-dimensional models of the patellar and quadriceps tendons was performed before and after the removal of a 10 mm-wide graft from both tendons. Length, thickness, and width measurements of the quadriceps tendon were made at predetermined locations. Anthropometric data were collected, and subgroup analysis, sex analysis, and linear regression were performed. Results: The mean percentage of volume remaining after removal of a 10 mm-wide graft from the patellar tendon was 56.6%, compared with 61.3% when harvesting an 80 mm-long graft of the same width from the quadriceps tendon. The intra-articular volume of the proposed quadriceps tendon graft was 87.5% greater than that of the patellar tendon graft. The mean length of the quadriceps tendon was 73.5 ± 12.3 mm in female patients and 81.1 ± 10.6 mm in male patients. These measurements were most highly correlated with patient height. The width of the quadriceps tendon decreased as one proceeded proximally from its insertion, and the thickness of the quadriceps tendon remained relatively constant. Conclusion: The quadriceps tendon has the anatomic characteristics to produce a graft whose length and volume are both reproducible and predictable, while yielding a graft with a significantly greater intra-articular volume than a patellar tendon graft with a similar width. |
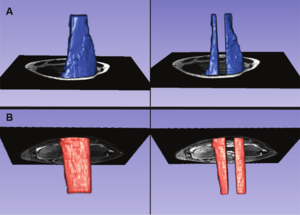 (A) A 3-dimensional model of the distal 8 cm of the quadriceps tendon, with and without the 10 mm–wide graft removed. Using the measurement tool on 3D Slicer, we measured the width of the quadriceps tendon from its insertion to 80 mm above its insertion. (B) A 3-dimensional model of the patellar tendon, with and without the 10 mm–wide graft removed. |
Optical Tractography of the Mouse Heart using Polarization-sensitive Optical Coherence Tomography
|
Publication: Biomed Opt Express. 2013 Oct 21;4(11):2540-5. PMID: 24298414 | PDF Authors: Wang Y, Yao G. Institution: Department of Bioengineering, University of Missouri, Columbia, MO, USA. Background/Purpose: We developed a method to image myocardial fiber architecture in the mouse heart using a Jones matrix-based polarization-sensitive optical coherence tomography (PSOCT) system. The “cross-helical” laminar structure of myocardial fibers can be clearly visualized using this technology. The obtained myocardial fiber organization agrees well with existing knowledge acquired using conventional histology and diffusion tensor magnetic resonance imaging. The open source 3D Slicer was used for 3D data visualization. |
 (a) The 3D structure image of the mouse heart; (b) the corresponding 3D tractographic visualization. The B-scan images of structure, local retardance and optical axis acquired along the dashed line in (a) are shown in (c)-(e). Also shown are the en face images of the (f) structure, (g) local retardance, (h) local optical axis, and (i) cardiac fiber tract of a small region of interest (ROI) extracted at transmural depths from 0.11 mm to 0.91 mm. As shown in (a), the ROI was extracted from the lateral side of the left ventricle wall and had a size of 1.57 mm × 20° rotation (B × C-scan). The size bars in (c) and (f) are 1 mm. |
Individual Subject Classification of Mixed Dementia from Pure Subcortical Vascular Dementia Based on Subcortical Shape Analysis
|
Publication: PLoS One. 2013 Oct 10;8(10):e75602. PMID: 24130724| PDF Authors: Kim HJ, Kim J, Cho H, Ye BS, Yoon CW, Noh Y, Kim GH, Lee JH, Kim JS, Choe YS, Lee KH, Kim CH, Seo SW, Weiner MW, Na DL, Seong JK. Institution: Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. Background/Purpose: Subcortical vascular dementia (SVaD), one of common causes of dementia, has concomitant Alzheimer's disease (AD) pathology in over 30%, termed "mixed dementia". Identifying mixed dementia from SVaD is important because potential amyloid-targeted therapies may be effective for treatment in mixed dementia. The purpose of this study was to discriminate mixed dementia from pure SVaD using magnetic resonance imaging (MRI). We measured brain amyloid deposition using the 11C-Pittsburgh compound B positron emission tomography (PiB-PET) in 68 patients with SVaD. A PiB retention ratio greater than 1.5 was considered PiB(+). Hippocampal and amygdalar shape were used in the incremental learning method to discriminate mixed dementia from pure SVaD because these structures are known to be prominently involved by AD pathologies. Among 68 patients, 23 (33.8%) patients were positive for PiB binding. With use of hippocampal shape analysis alone, PiB(+) SVaD could be discriminated from PiB(-) SVaD with 77.9% accuracy (95.7% sensitivity and 68.9% specificity). With use of amygdalar shape, the discrimination accuracy was 75.0% (87.0% sensitivity and 68.9% specificity). When hippocampal and amygdalar shape were analyzed together, accuracy increased to 82.4% (95.7% sensitivity and 75.6% specificity). An incremental learning method using hippocampal and amygdalar shape distinguishes mixed dementia from pure SVaD. Furthermore, our results suggest that amyloid pathology and vascular pathology have different effects on the shape of the hippocampus and amygdala. |
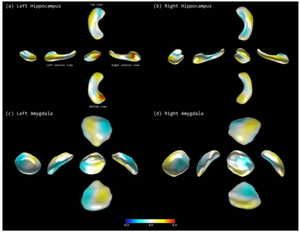 Discriminative regions in classification: (a) left hippocampus, (b) right hippocampus, (c) left amygdala, and (d) right amygdala. Each figure visualizes the LDA axes on the atlas meshes. An expert neuroanatomist manually delineated hippocampal volumes of 20 healthy subjects from the T1 images slice-by-slice using version 4.2.2 of 3D Slicer. |
3D Prostate Histology Image Reconstruction: Quantifying the Impact of Tissue Deformation and Histology Section Location
|
Publication: J Pathol Inform. 2013 Oct 31;4:31. PMID: 24392245 | PDF Authors: Gibson E, Gaed M, Gómez JA, Moussa M, Pautler S, Chin JL, Crukley C, Bauman GS, Fenster A, Ward AD. Institution: Robarts Research Institute, London, Canada. Background/Purpose: Guidelines for localizing prostate cancer on imaging are ideally informed by registered post-prostatectomy histology. 3D histology reconstruction methods can support this by reintroducing 3D spatial information lost during histology processing. The need to register small, high-grade foci drives a need for high accuracy. Accurate 3D reconstruction method design is impacted by the answers to the following central questions of this work. (1) How does prostate tissue deform during histology processing? (2) What spatial misalignment of the tissue sections is induced by microtome cutting? (3) How does the choice of reconstruction model affect histology reconstruction accuracy? Histology, paraffin block face and magnetic resonance images were acquired for 18 whole mid-gland tissue slices from six prostates. 7-15 homologous landmarks were identified on each image. Tissue deformation due to histology processing was characterized using the target registration error (TRE) after landmark-based registration under four deformation models (rigid, similarity, affine and thin-plate-spline [TPS]). The misalignment of histology sections from the front faces of tissue slices was quantified using manually identified landmarks. The impact of reconstruction models on the TRE after landmark-based reconstruction was measured under eight reconstruction models comprising one of four deformation models with and without constraining histology images to the tissue slice front faces. Isotropic scaling improved the mean TRE by 0.8-1.0 mm (all results reported as 95% confidence intervals), while skew or TPS deformation improved the mean TRE by <0.1 mm. The mean misalignment was 1.1-1.9(°) (angle) and 0.9-1.3 mm (depth). Using isotropic scaling, the front face constraint raised the mean TRE by 0.6-0.8 mm. For sub-millimeter accuracy, 3D reconstruction models should not constrain histology images to the tissue slice front faces and should be flexible enough to model isotropic scaling. |
Heat-induced Shrinkage and Shape Preservation of Teeth: A Radiologic Evaluation
|
Publication: J Forensic Odontostomatol. 2013 Oct 1;31 Suppl 1:40-1. Authors: Sandholzer MA, Walmsley DA, Lumley P, Landini G. Institution: School of Dentistry, University of Birmingham, UK. Background/Purpose: Teeth subjected to high temperatures following natural disasters, airplane crashes or house fires can sometimes be the only remains available for forensic identification. The information on macro- and microscopic heat-induced changes of teeth can therefore provide relevant information that can facilitate the identification process. An important macroscopic feature of burned dental remains is the gradual change in color due to compositional changes (i.e. loss of organic content), which generally allows to deduce a temperature range and can indicate the possible preservation of DNA. In practice, the most reliable and frequently applied method for identification of fire victims is comparative dental radiography, based on the comparison of dentition features. Although forensic odontologists are often confronted with fragmented and isolated dental remains, there is still a lack of precise data for the heat-induced dimensional and morphological changes of human teeth that might influence the identification process. This study therefore investigated the volumetric shrinkage, shape preservation, weight loss and color alterations of human teeth and looked at the effects of previously reported heating protocols to enable testing the reliability and inter-comparability of results published in literature. Materials and Methods: A total of 104 freshly extracted sound molars and premolars were included in this study. Micro-CT scans (SkyScan 1172; voxel-size 13.5 µm) were performed before and after exposure to three different previously reported heating regimes in a range of 400 - 1000°C. Volumetric shrinkage was analyzed using Fiji and 3D Slicer software. The weight loss was documented with an high-precision analytical scale. Photographic color measurements and image analysis were performed on calibrated digital photographs and representative color palettes were computed for every experimental group using the Fiji software package. Results: A progressive, temperature-dependent shift of colors was observed, with apparent differences depending on the chosen heating regime. Although fragmentation and cracks at elevated temperatures often affected the pulp chamber and root canals, overall tooth morphology was well preserved. The temperature and the chosen heating regime had a statistically significant influence on the dentinal volumetric shrinkage, which ranged from 4.8% (at 400°C) to 32.5% (at 1000°C). A major increase in shrinkage occurred between 700°C and 800°C, whilst no significant statistical difference was found between lower temperature groups. The weight loss measurements overall correlated significantly with the shrinkage, with a mean weight loss between 7.8% (at 400°C) and 32.8% (at 1000°C), again significantly differing between the heating regimes. Conclusion: In conclusion, the findings of this study showed definite differences of the macro- and microscopic changes related to the experimental heating regime, adding information on the dentinal shrinkage and shape preservation over a large range of temperatures found in possible forensic scenarios. The color changes are summarized in the newly developed color palettes and can be used to deduce a temperature range. By vigilantly implementing the knowledge on the specific color changes, dentinal shrinkage and shape preservation the odontological identification process of fire victims can eventually be facilitated in cases where only fragmented or isolated dental remains are present. |
Clinical Correlates of Nucleus Accumbens Volume in Drug-naive, Adult Patients with Obsessive-compulsive Disorder
|
Publication: Aust N Z J Psychiatry. 2013 Oct;47(10):930-7. PMID: 23737599 Authors: Narayanaswamy JC, Jose D, Kalmady S, Venkatasubramanian G, Reddy YJ. Institution: Obsessive Compulsive Disorder Clinic & Translational Psychiatry Lab, Neurobiology Research Center at National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore, India. Background/Purpose: Background:Reward-processing deficits have been demonstrated in obsessive-compulsive disorder (OCD) and this has been linked to ventral striatal abnormalities. However, volumetric abnormalities of the nucleus accumbens (NAcc), a key structure in the reward pathway, have not been examined in OCD. We report on the volumetric abnormalities of NAcc and its correlation with illness severity in drug-naïve, adult patients with OCD. Method: In this cross-sectional study of case-control design, the magnetic resonance imaging (MRI) 1.5-T (1-mm) volume of NAcc was measured using 3D Slicer software in drug-naïve OCD patients (n = 44) and age, sex and handedness-matched healthy controls (HCs) (n = 36) using a valid and reliable method. OCD symptoms were assessed using the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) Symptom checklist and severity and the Clinical Global Impression-Severity (CGI-S) scale. Results: There was no significant difference in NAcc volumes on either side between OCD patients and HCs (F = 3.45, p = 0.07). However, there was significant negative correlation between the right NAcc volume and Y-BOCS compulsion score (r = -0.48, p = 0.001). Conclusion:Study observations suggest involvement of the NAcc in the pathogenesis of OCD, indicating potential reward-processing deficits. Correlation between the right NAcc volume deficit and severity of compulsions offers further support for this region as a candidate for deep brain stimulation treatment in OCD. |
Probing the Regional Distribution of Pulmonary Gas Exchange through Single-breath gas- and Dissolved-phase 129Xe MR Imaging
|
Publication: J Appl Physiol. 2013 Sep;115(6):850-60. PMID: 23845983 | PDF Authors: Kaushik SS, Freeman MS, Cleveland ZI, Davies J, Stiles J, Virgincar RS, Robertson SH, He M, Kelly KT, Foster WM, McAdams HP, Driehuys BP. Institution: Department of Biomedical Engineering, Duke University, Durham, NC, USA. Background/Purpose: Although some central aspects of pulmonary function (ventilation and perfusion) are known to be heterogeneous, the distribution of diffusive gas exchange remains poorly characterized. A solution is offered by hyperpolarized 129Xe magnetic resonance (MR) imaging, because this gas can be separately detected in the lung's air spaces and dissolved in its tissues. Early dissolved-phase 129Xe images exhibited intensity gradients that favored the dependent lung. To quantitatively corroborate this finding, we developed an interleaved, three-dimensional radial sequence to image the gaseous and dissolved 129Xe distributions in the same breath. These images were normalized and divided to calculate "129Xe gas-transfer" maps. We hypothesized that, for healthy volunteers, 129Xe gas-transfer maps would retain the previously observed posture-dependent gradients. This was tested in nine subjects: when the subjects were supine, 129Xe gas transfer exhibited a posterior-anterior gradient of -2.00 ± 0.74%/cm; when the subjects were prone, the gradient reversed to 1.94 ± 1.14%/cm (P < 0.001). The 129Xe gas-transfer maps also exhibited significant heterogeneity, as measured by the coefficient of variation, that correlated with subject total lung capacity (r = 0.77, P = 0.015). Gas-transfer intensity varied nonmonotonicaly with slice position and increased in slices proximal to the main pulmonary arteries. Despite substantial heterogeneity, the mean gas transfer for all subjects was 1.00 ± 0.01 while supine and 1.01 ± 0.01 while prone (P = 0.25), indicating good "matching" between gas- and dissolved-phase distributions. This study demonstrates that single-breath gas- and dissolved-phase 129Xe MR imaging yields 129Xe gas-transfer maps that are sensitive to altered gas exchange caused by differences in lung inflation and posture. Funding:
|
 Image processing used to limit the analysis to the thoracic cavity. A: gas-phase image (green) overlaid on the corresponding thoracic cavity image (grayscale) prior to registration. Postregistration thoracic cavity image (B) was used to create a thoracic cavity mask that defines the data analysis region (C). Airways in the mask were manually segmented, and the mask was then subjected to morphological closing with a spherical structuring element (7-pixel diameter) and a filling operation to yield the final mask (D). E: outline of the processed thoracic cavity mask on the gas-phase image. The thoracic cavity image was then segmented using the region-growing algorithm in 3D Slicer to create a binary thoracic cavity “mask” |
Resection Probability Maps for Quality Assessment of Glioma Surgery without Brain Location Bias
|
Publication: PLoS One. 2013 Sep 6;8(9):e73353. PMID: 24039922| PDF Authors: De Witt Hamer PC, Hendriks EJ, Mandonnet E, Barkhof F, Zwinderman AH, Duffau H. Institution: Neurosurgical Center Amsterdam, VU University Medical Center, Amsterdam, The Netherlands. Background/Purpose: Intraoperative brain stimulation mapping reduces permanent postoperative deficits and extends tumor removal in resective surgery for glioma patients. Successful functional mapping is assumed to depend on the surgical team's expertise. In this study, glioma resection results are quantified and compared using a novel approach, so-called resection probability maps (RPM), exemplified by a surgical team comparison, here with long and short experience in mapping. Methods: Adult patients with glioma were included by two centers with two and fifteen years of mapping experience. Resective surgery was targeted at non-enhanced MRI extension and was limited by functional boundaries. Neurological outcome was compared. To compare resection results, we applied RPMs to quantify and compare the resection probability throughout the brain at 1 mm resolution. Considerations for spatial dependence and multiple comparisons were taken into account. Results: The senior surgical team contributed 56, and the junior team 52 patients. The patient cohorts were comparable in age, preoperative tumor volume, lateralization, and lobe localization. Neurological outcome was similar between teams. The resection probability on the RPMs was very similar, with none (0%) of 703,967 voxels in left-sided tumors being differentially resected, and 124 (0.02%) of 644,153 voxels in right-sided tumors. Conclusion: RPMs provide a quantitative volumetric method to compare resection results, which we present as standard for quality assessment of resective glioma surgery because brain location bias is avoided. Stimulation mapping is a robust surgical technique, because the neurological outcome and functional-based resection results using stimulation mapping are independent of surgical experience, supporting wider implementation. |
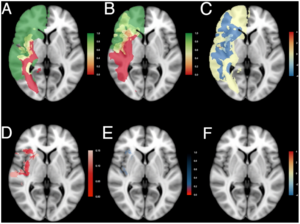 Resection probability maps for right-sided gliomas. Results comparing (A) the junior surgical team, n = 29, and (B) the senior surgical team, n = 29, are shown superimposed on standard brain space (MNI152). A probability of 0 (red) represents locations where tumor was never resected, and a probability of 1 (green) represents locations where tumor was resected in all patients. An intermediate probability (yellow) represents locations where glioma was removed in a subset of patients. (C) Relative differences in probability of resection as log odds ratio. (D) The adjusted p-value map adjusted by the empirical null-distribution to address spatial dependency of voxels. Values less than 0.15 are plotted in shades of red. (E) The q-value map to address multiple testing. Values below 0.2 are plotted in shades of red, values between 0.2 and 0.8 in shades of blue. (F) Differences in probability of resection as log odds ratio for voxels with a q-value less than 0.2 demonstrate similar resection results between the two patient cohorts. Results are superimposed on a transversal section at z = 0 of MNI152. See Movie S2 for all transversal sections. |
Consistent Surgeon Evaluations of Three-Dimensional Rendering of PET/CT Scans of the Abdomen of a Patient with a Ductal Pancreatic Mass
|
Publication: PLoS One. 2013 Sep 24;8(9):e75237. PMID: 24086475| PDF Authors: Wampole ME, Kairys JC, Mitchell EP, Ankeny ML, Thakur ML, Wickstrom E. Institution: Department of Biochemistry and Molecular Biology, Thomas Jefferson University, Philadelphia, PA, USA. Background/Purpose: Two-dimensional (2D) positron emission tomography (PET) and computed tomography (CT) are used for diagnosis and evaluation of cancer patients, requiring surgeons to look through multiple planar images to comprehend the tumor and surrounding tissues. We hypothesized that experienced surgeons would consistently evaluate three-dimensional (3D) presentation of CT images overlaid with PET images when preparing for a procedure. We recruited six Jefferson surgeons to evaluate the accuracy, usefulness, and applicability of 3D renderings of the organs surrounding a malignant pancreas prior to surgery. PET/CT and contrast-enhanced CT abdominal scans of a patient with a ductal pancreatic mass were segmented into 3D surface renderings, followed by co-registration. Version A used only the PET/CT image, while version B used the contrast-enhanced CT scans co-registered with the PET images. The six surgeons answered 15 questions covering a) the ease of use and accuracy of models, b) how these models, with/without PET, changed their understanding of the tumor, and c) what are the best applications of the 3D visualization, on a scale of 1 to 5. The six evaluations revealed a statistically significant improvement from version A (score 3.6±0.5) to version B (score 4.4±0.4). A paired-samples t-test yielded t(14) = -8.964, p<0.001. Across the surgeon cohort, contrast-enhanced CT fused with PET provided a more lifelike presentation than standard CT, increasing the usefulness of the presentation. The experienced surgeons consistently reported positive reactions to 3D surface renderings of fused PET and contrast-enhanced CT scans of a pancreatic cancer and surrounding organs. Thus, the 3D presentation could be a useful preparative tool for surgeons prior to making the first incision. This result supports proceeding to a larger surgeon cohort, viewing prospective 3D images from multiple types of cancer. Funding:
|
Fiber Tract-Driven Topographical Mapping (FTTM) Reveals Microstructural Relevance for Interhemispheric Visuomotor Function in the Aging Brain
|
Publication: Neuroimage. 2013 Aug 15;77:195-206. PMID: 23567886 | PDF Authors: Schulte T, Maddah M, Müller-Oehring EM, Rohlfing T, Pfefferbaum A, Sullivan EV. Institution: SRI International, Neuroscience Program, Menlo Park, CA, USA. Background/Purpose: We present a novel approach - DTI-based fiber tract-driven topographical mapping (FTTM) - to map and measure the influence of age on the integrity of interhemispheric fibers and challenge their selective functions with measures of interhemispheric integration of lateralized information. This approach enabled identification of spatially specific topographical maps of scalar diffusion measures and their relation to measures of visuomotor performance. Relative to younger adults, older adults showed lower fiber integrity indices in anterior than posterior callosal fibers. FTTM analysis identified a dissociation in the microstructural-function associates between age groups: in younger adults, genu fiber integrity correlated with interhemispheric transfer time, whereas in older adults, body fiber integrity was correlated with interhemispheric transfer time with topographical specificity along left-lateralized callosal fiber trajectories. Neural co-activation from redundant targets was evidenced by fMRI-derived bilateral extrastriate cortex activation in both groups, and a group difference emerged for a pontine activation cluster that was differently modulated by response hand in older than younger adults. Bilateral processing advantages in older but not younger adults further correlated with fiber integrity in transverse pontine fibers that branch into the right cerebellar cortex, thereby supporting a role for the pons in interhemispheric facilitation. In conclusion, in the face of compromised anterior callosal fibers, older adults appear to use alternative pathways to accomplish visuomotor interhemispheric information transfer and integration for lateralized processing. This shift from youthful associations may indicate recruitment of compensatory mechanisms involving medial corpus callosum fibers and subcortical pathways. Funding:
|
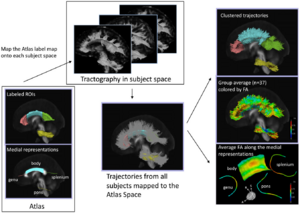 Pipeline for DTI-based fiber tract-driven topographic mapping (FTTM) analysis. Left panel: (Bottom) Labeled ROIs in the ICBM-DTI-81 atlas and the derived initial medial representation of each bundle. Middle panel: (Top) The ROIs are mapped to each subject space by applying the affine transformation obtained by registering the FA volume of the atlas to the FA volume of each subject. Seeded from the registered ROIs, streamline tractography is performed in each subject's native image space using 3D Slicer3). (Bottom) Trajectories from all 37 subjects are mapped back to the atlas space and are clustered into bundles based on their spatial proximity and shape similarity to the medial representation of fiber tracts in the atlas. Right panel: (Top) Trajectories are colored with the most probable label assigned in the clustering process. (Middle) Trajectories are colored with the FA values. (Bottom) The medial representation of each bundle is colored by the average FA of trajectories in each bundle summarizing the local variation of the diffusion parameter along that fiber bundle, thereby providing topographic parameter maps. |
Prostate Volumetric Assessment by Magnetic Resonance Imaging and Transrectal Ultrasound: Impact of Variation in Calculated Prostate-Specific Antigen Density on Patient Eligibility for Active Surveillance Program
|
Publication: Journal of Computer Assisted Tomography. 2013 Jul/Aug;37(4):589-95. PMID: 23863537 Authors: Dianat SS, Rancier Ruiz RM, Bonekamp D, Carter HB, Macura KJ. Institution: Department of Radiology, Johns Hopkins University, Baltimore, MD. Background/Purpose: The objective of this study was to investigate impact of prostate volume variations on prostate-specific antigen density (PSAD) and patient eligibility for active surveillance (AS). Methods: Prostate volume and PSAD were calculated for 46 patients with prostate cancer in AS who underwent prostate magnetic resonance imaging and transrectal ultrasound (TRUS). Manual method and 2 semiautomated methods for prostate segmentation (3D Slicer and OsiriX) were used for MR volumetry. Results: Magnetic resonance volumetric methods showed very good agreement (intraclass correlation coefficient, 0.98). The concordance correlation coefficient was higher among MR volumetry methods (0.971-0.998) than between TRUS and MR volumetry (0.849-0.863). The variation in PSAD estimated by TRUS versus magnetic resonance imaging was higher in large prostates (r = 0.327, P = 0.027). Transrectal ultrasonography volumetry may improperly classify 20% of patients as eligible for AS with PSAD greater than 0.15 threshold. Conclusion: Although clinically used TRUS reliably estimates PSAD, it may misclassify some patients who are not eligible for AS based on PSAD criteria. Magnetic resonance-based volumetry should be considered for a more reliable PSAD calculation. |
Quantification and Analysis of 3D Magnetic Resonance Image Brain Tumor
|
Publication: International Journal of Tomography & Simulation. 2013 Jul; 24(3):17-26. Authors: Aju D, Ray, BK. Institution: Department of Neurosurgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA. Background/Purpose: An analysis and detection of brain tumor is performed using MRI scanned images. Also a 3D visualization of the detected tumor part and its quantification is achieved through the proposed methodology. Initially, the noise is reduced by applying high pass filter and image enhancement is performed as a preprocessing step to enhance the input image quality. Morphological operations are applied to the enhanced image to detect the shape of the tumor in the enhanced image. The tumor part is mapped onto the original gray scale image with 255 intensity values to make the tumor visible more in the image. 3D Slicer is utilized to extract and visualize the 3D tumor data. The volume of the extracted 3D tumor portion is also calculated using 3D Slicer. The methodology has been tried out on a number of different input data sets and it is observed that it always gave the precise and desired result. |
Optic Radiation Fiber Tractography in Glioma Patients Based on High Angular Resolution Diffusion Imaging with Compressed Sensing Compared with Diffusion Tensor Imaging - Initial Experience
|
Publication: PLoS One. 2013 Jul;8(7):e70973. PMID: 23923036 | PDF Authors: Kuhnt D, Bauer M, Sommer J, Merhof D, Nimsky C. Institution: Department of Neurosurgery, University of Marburg, Marburg, Germany. Background/Purpose: Up to now, fiber tractography in the clinical routine is mostly based on diffusion tensor imaging (DTI). However, there are known drawbacks in the resolution of crossing or kissing fibers and in the vicinity of a tumor or edema. These restrictions can be overcome by tractography based on High Angular Resolution Diffusion Imaging (HARDI) which in turn requires larger numbers of gradients resulting in longer acquisition times. Using compressed sensing (CS) techniques, HARDI signals can be obtained by using less non-collinear diffusion gradients, thus enabling the use of HARDI-based fiber tractography in the clinical routine. Eight patients with gliomas in the temporal lobe, in proximity to the optic radiation (OR), underwent 3T MRI including a diffusion-weighted dataset with 30 gradient directions. Fiber tractography of the OR using a deterministic streamline algorithm based on DTI was compared to tractography based on reconstructed diffusion signals using HARDI+CS. HARDI+CS based tractography displayed the OR more conclusively compared to the DTI-based results in all eight cases. In particular, the potential of HARDI+CS-based tractography was observed for cases of high grade gliomas with significant peritumoral edema, larger tumor size or closer proximity of tumor and reconstructed fiber tract. Overcoming the problem of long acquisition times, HARDI+CS seems to be a promising basis for fiber tractography of the OR in regions of disturbed diffusion, areas of high interest in glioma surgery. Funding:
|
 Fiber tractography results presented for each patient (patients 1–8 according rows 1–8) based on DTI (column 1), 3D Slicer (column 2), and based on HARDI+CS (column 4) within MedAlyVis. Overlay of DTI-based (red) and HARDI+CS-based tractography (green) (r = right; l = left; a = anterior; p = posterior). |
Endodontic Access Cavity Simulation in Ceramic Dental Crowns
|
Publication: Dent Mater. 2013 Jun;29(6):626-34. PMID: 23587359 Authors: Cuddihy M, Gorman CM, Burke FM, Ray NJ, Kelliher D. Institution: Department of Materials, Royal School of Mines, Imperial College London, London, UK. Background/Purpose: It is proposed that a non-uniform rational B-spline (NURBS) based solid geometric model of a ceramic crown would be a flexible and quick approach to virtually simulate root canal access cavities. The computation of strain components orthogonal to surface flaws generated during the drilling would be an appropriate way of comparing different access cavity configurations. Methods: A μCT scan is used to develop a full 3D NURBS geometric solid model of a ceramic crown. Three different access cavity configurations are created virtually in the geometric model and there are then imported into proprietary finite element software. A linear analysis of the each crown is carried out under appropriate in vivo loading and the results are post-processed to carry out a quantitative comparison of the three configurations. Results: The geometric model is shown to be a flexible and quick way of simulation access cavities. Preliminary indications are that post processed strain results from the finite element analysis are good comparators of competing access cavity configurations. SIGNIFICANCE: The generation of geometric solid models of dental crowns from μCT scans is a flexible and efficient methodology to simulate a number of access cavity configurations. Furthermore, advanced post-processing of the primary finite element analysis results is worthwhile as preliminary results indicate that improved quantitative comparisons between different access cavity configurations are possible. In this work, all image processing and reconstruction work is undertaken in 3D Slicer, an open source medical visualization software package. |
Augmented Reality Visualization using Image Overlay Technology for MR-Guided Interventions: Cadaveric Bone Biopsy at 1.5 T
|
Publication: Invest Radiol. 2013 Jun;48(6):464-70. PMID: 23328911 Authors: Fritz J, U-Thainual P, Ungi T, Flammang AJ, McCarthy EF, Fichtinger G, Iordachita II, Carrino JA. Institution: Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins University School of Medicine, Baltimore, MD, USA. Background/Purpose: The purpose of this study was to prospectively test the hypothesis that image overlay technology facilitates accurate navigation for magnetic resonance (MR)-guided osseous biopsy. A prototype augmented reality image overlay system was used in conjunction with a clinical 1.5-T MR imaging system. Osseous biopsy of a total of 16 lesions was planned in 4 human cadavers with osseous metastases. A loadable module of 3D Slicer open-source medical image analysis and visualization software was developed and used for display of MR images, lesion identification, planning of virtual biopsy paths, and navigation of drill placement. The osseous drill biopsy was performed by maneuvering the drill along the displayed MR image containing the virtual biopsy path into the target. The drill placement and the final drill position were monitored by intermittent MR imaging. Outcome variables included successful drill placement, number of intermittent MR imaging control steps, target error, number of performed passes and tissue sampling, time requirements, and pathological analysis of the obtained osseous core specimens including adequacy of specimens, presence of tumor cells, and degree of necrosis. A total of 16 osseous lesions were sampled with percutaneous osseous drill biopsy. Eight lesions were located in the osseous pelvis (8/16, 50%) and 8 (8/16, 50%) lesions were located in the thoracic and lumbar spine. Lesion size was 2.2 cm (1.1-3.5 cm). Four (2-8) MR imaging control steps were required. MR imaging demonstrated successful drill placement inside 16 of the 16 target lesions (100%). One needle pass was sufficient for accurate targeting of all lesions. One tissue sample was obtained in 8 of the 16 lesions (50%); 2, in 6 of the16 lesions (38%); and 3, in 2 of the 16 lesions (12%). The target error was 4.3 mm (0.8-6.8 mm). Length of time required for biopsy of a single lesion was 38 minutes (20-55 minutes). Specimens of 15 of the 16 lesions (94%) were sufficient for pathological evaluation. Of those 15 diagnostic specimens, 14 (93%) contained neoplastic cells, whereas 1 (7%) specimen demonstrated bone marrow without evidence of neoplastic cells. Of those 14 diagnostic specimens, 11 (79%) were diagnostic for carcinoma or adenocarcinoma, which was concordant with the primary neoplasm, whereas, in 3 of the 14 diagnostic specimens (21%), the neoplastic cells were indeterminate. Image overlay technology provided accurate navigation for the MR-guided biopsy of osseous lesions of the spine and the pelvis in human cadavers at 1.5 T. The high technical and diagnostic yield supports further evaluation with clinical trials. Funding:
|
How to Detect Amygdala Activity with Magnetoencephalography using Source Imaging
|
Publication: J Vis Exp. 2013; (76):50212 PMID: 23770774 | PDF Authors: Balderston NL, Schultz DH, Baillet S, Helmstetter FJ. Institution: Department of Psychology, University of Wisconsin-Milwaukee, WI, USA. Background/Purpose: In trace fear conditioning a conditional stimulus (CS) predicts the occurrence of the unconditional stimulus (UCS), which is presented after a brief stimulus free period (trace interval)(1). Because the CS and UCS do not co-occur temporally, the subject must maintain a representation of that CS during the trace interval. In humans, this type of learning requires awareness of the stimulus contingencies in order to bridge the trace interval(2-4). However when a face is used as a CS, subjects can implicitly learn to fear the face even in the absence of explicit awareness*. This suggests that there may be additional neural mechanisms capable of maintaining certain types of "biologically-relevant" stimuli during a brief trace interval. Given that the amygdala is involved in trace conditioning, and is sensitive to faces, it is possible that this structure can maintain a representation of a face CS during a brief trace interval. It is challenging to understand how the brain can associate an unperceived face with an aversive outcome, even though the two stimuli are separated in time. Furthermore investigations of this phenomenon are made difficult by two specific challenges. First, it is difficult to manipulate the subject's awareness of the visual stimuli. One common way to manipulate visual awareness is to use backward masking. In backward masking, a target stimulus is briefly presented (< 30 msec) and immediately followed by a presentation of an overlapping masking stimulus(5). The presentation of the mask renders the target invisible(6-8). Second, masking requires very rapid and precise timing making it difficult to investigate neural responses evoked by masked stimuli using many common approaches. Blood-oxygenation level dependent (BOLD) responses resolve at a timescale too slow for this type of methodology, and real time recording techniques like electroencephalography (EEG) and magnetoencephalography (MEG) have difficulties recovering signal from deep sources. However, there have been recent advances in the methods used to localize the neural sources of the MEG signal(9-11). By collecting high-resolution MRI images of the subject's brain, it is possible to create a source model based on individual neural anatomy. Using this model to "image" the sources of the MEG signal, it is possible to recover signal from deep subcortical structures, like the amygdala and the hippocampus. Funding:
|
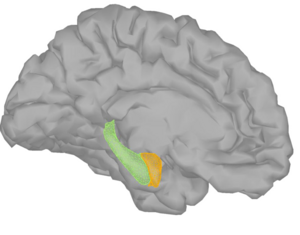 MEG results from a typical conditioning experiment. The figure shows the 3D models of the amygdala (orange), hippocampus (green), using 3D Slicer and cerebral cortex used to model the sources of the MEG signal. |
Paired Inspiratory-expiratory Chest CT Scans to Assess for Small Airways Disease in COPD
|
Publication: Respir Res. 2013 Apr;14:42. PMID: 23566024 | PDF Authors: Hersh CP, Washko GR, Estépar RS, Lutz S, Friedman PJ, Han MK, Hokanson JE, Judy PF, Lynch DA, Make BJ, Marchetti N, Newell JD Jr, Sciurba FC, Crapo JD, Silverman EK; COPDGene Investigators Institution: Channing Division of Network Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Gas trapping quantified on chest CT scans has been proposed as a surrogate for small airway disease in COPD. We sought to determine if measurements using paired inspiratory and expiratory CT scans may be better able to separate gas trapping due to emphysema from gas trapping due to small airway disease. Methods: Smokers with and without COPD from the COPDGene Study underwent inspiratory and expiratory chest CT scans. Emphysema was quantified by the percent of lung with attenuation < −950HU on inspiratory CT. Four gas trapping measures were defined: (1) Exp−856, the percent of lung < −856HU on expiratory imaging; (2) E/I MLA, the ratio of expiratory to inspiratory mean lung attenuation; (3) RVC856-950, the difference between expiratory and inspiratory lung volumes with attenuation between −856 and −950 HU; and (4) Residuals from the regression of Exp−856 on percent emphysema. Results: In 8517 subjects with complete data, Exp−856 was highly correlated with emphysema. The measures based on paired inspiratory and expiratory CT scans were less strongly correlated with emphysema. Exp−856, E/I MLA and RVC856-950 were predictive of spirometry, exercise capacity and quality of life in all subjects and in subjects without emphysema. In subjects with severe emphysema, E/I MLA and RVC856-950 showed the highest correlations with clinical variables. Conclusions: Quantitative measures based on paired inspiratory and expiratory chest CT scans can be used as markers of small airway disease in smokers with and without COPD, but this will require that future studies acquire both inspiratory and expiratory CT scans. Funding:
|
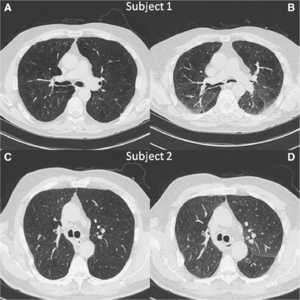 Inspiratory (A,C) and expiratory (B,D) chest CT images from two subjects with similar percent of lung voxels with attenuation values < −856HU on expiratory CT scans (Exp−856) demonstrate the inability of expiratory image analysis alone to distinguish gas trapping due to emphysema from gas trapping due to small airway disease. Computerized image analysis was performed with 3D SLICER software. |
Imaging in Audiology: A Case Report of a Patient with Bilateral Acoustic Neuroma
|
Publication: Poster Presentation at the 11th congress of the European Federation of Audiology Societies (EFAS) June 19-22, 2013. Poster with Embedded Video [codec: Xvid (free,open source), Office: MS Office 2010] | Case Time Line Authors: Nagy AL, Jarabin J, Toth F, Rovo L, Kiss JG. Institution: University of Szeged, Department of Oto-rhino-laryngology and Head and Neck Surgery, Szeged, Hungary. Background/Purpose: We present a patient with bilateral acoustic neuromas. The tumor was tracked from 2006 until 2013. Pre- and postoperative CT and MR scans are shown. Both neuroma volumes were computed at different time points, before and after various interventions (stereotaxic irradiation, neurosurgery). We also compared the size change of the neuromas over time at different time points, by registering five volumes of differing modalities (four MR and one CT) using a one-by-one registration technique. We used the freely available open source software 3D Slicer to reconstruct 3D CT and MR data, to register, and overlay them; and to visually track the changes. |
Computed Tomography Image Processing to Detect the Real Mechanism of Bioprosthesis Failure: Implication for Valve-in-valve Implantation
|
Publication: J Heart Valve Dis. 2013 Mar;22(2):236-8. PMID: 23798214 Authors: Ruggieri VG, Anselmi A, Wang Q, Esneault S, Haigron P, Verhoye JP. Institution: Department of Cardiovascular and Thoracic Surgery, Pontchaillou University Hospital, Rennes, France. Background/Purpose: Transcatheter valve-in-valve implantation is an emerging option for patients with structural deterioration of an aortic bioprosthesis and who are at a high surgical risk. The present case underlines the need for dedicated imaging to accurately understand the mechanism of valve failure, and the feasibility of a valve-in-valve procedure. Methods: A patient with structural bioprosthetic deterioration at echocardiography was investigated using computed tomography (CT) scanning and novel 3D Slicer software. The findings were compared with those revealed at intraoperative pathology. Results: Post-processed CT images showed the bulk of calcifications to be located at the subvalvular level, suggesting the presence of calcified pannus. Pathology of the explanted valve confirmed that the valve stenosis was due primarily to pannus. Misdiagnosed calcified pannus represents a major threat during valve-in-valve procedures, due mainly to embolic risk. Conclusion: The 3D Slicer elaboration of CT images may be invaluable in providing a precise definition of the mechanism of valve failure, and also to establish the feasibility of either a valve-in-valve procedure or conventional surgery. |
|
Publication: J Neurol Surg A Cent Eur Neurosurg. 2013 Mar;74(2):71-6. PMID: 23404553 Authors: Inoue D, Cho B, Mori M, Kikkawa Y, Amano T, Nakamizo A, Yoshimoto K, Mizoguchi M, Tomikawa M, Hong J, Hashizume M, Sasaki T. Institution: Department of Neurosurgery, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan. Background/Purpose: To develop an augmented reality (AR) neuronavigation system with Web cameras and examine its clinical utility. The utility of the system was evaluated in three patients with brain tumors. One patient had a glioblastoma and two patients had convexity meningiomas. Our navigation system comprized the open-source software 3D Slicer (Brigham and Women's Hospital, Boston, MA, USA), the infrared optical tracking sensor Polaris (Northern Digital Inc., Waterloo, Canada), and Web cameras. We prepared two different types of Web cameras: a handheld type and a headband type. Optical markers were attached to each Web camera. We used this system for skin incision planning before the operation, during craniotomy, and after dural incision. Results: We were able to overlay these images in all cases. In Case 1, accuracy could not be evaluated because the tumor was not on the surface, though it was generally suitable for the outline of the external ear and the skin. In Cases 2 and 3, the augmented reality error was ∼2 to 3 mm. AR technology was examined with Web cameras in neurosurgical operations. Our results suggest that this technology is clinically useful in neurosurgical procedures, particularly for brain tumors close to the brain surface. |
Quantitative MRI Analysis of Craniofacial Bone Marrow in Patients with Sickle Cell Disease
|
Publication: AJNR Am J Neuroradiol. 2013 Mar;34(3):622-7. PMID: 22878006| PDF Authors: Elias EJ, Liao JH, Jara H, Watanabe M, Nadgir RN, Sakai Y, Erbay K, Saito N, Ozonoff A, Steinberg MH, Sakai O. Institution: Departments of Radiology and Medicine, Boston Medical Center, Boston University School of Medicine, Boston, MA, USA. Background/Purpose: Assessment of bone marrow is most commonly performed qualitatively in the spine or other large long bones. The craniofacial bones are less ideal for bone marrow analysis because of the relatively small bone marrow volume. Because patients with SCD often undergo repeated brain imaging to evaluate for cerebral vaso-occlusive disease, quantitative assessment of craniofacial bone marrow is a reasonable possibility in these patients. The purpose of this study was to investigate specific sickle cell disease changes in craniofacial bone marrow quantitatively by analyzing T1, T2 and secular-T2 relaxation times and volume with the use of quantitative MRI. Fourteen patients with SCD and 17 control subjects were imaged with the mixed TSE pulse sequence at 1.5T. The craniofacial bones were manually segmented by using 3D Slicer to generate bone marrow volumes and to provide T1, T2, and secular-T2 relaxation times. All subjects exhibited a bimodal T1 histogram. In the SCD group, there was a decrease in amplitude in the first T1 peak and an increase in amplitude in the second T1 peak. The first T1 peak showed a significant increase in relaxation time compared with control subjects (P < .0001), whereas there was no significant difference in the second T1 peak. T2 and secular-T2 relaxation times were significantly shorter in the SCD group (T2, P < .0001; secular-T2, P < .0001). Increasing numbers of blood transfusions resulted in a decrease in T2 and secular-T2 times. Patients with SCD exhibited a larger bone marrow volume compared with control subjects, even after standardization. Patients with SCD exhibited significant quantifiable changes in the craniofacial bone marrow because of failure of red-to-yellow marrow conversion and iron deposition that can be identified by qMRI relaxometry and volumetry. Both qMRI relaxometry and volumetry may be used as noninvasive tools for assessment of disease severity. |
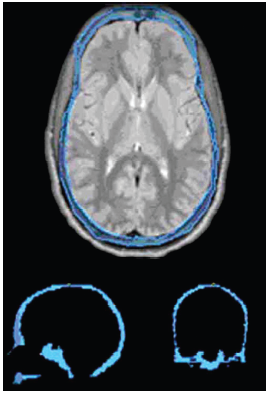 Craniofacial bone marrow segmentation. The bone marrow of a 24.5-year-old man with sickle cell disease (outlined in blue) has been segmented on the axial proton attenuation–weighted images with 3 mm thickness. Approximately 75 images were segmented per subject. After segmentation was complete, 3D Slicer was used to layer the images over each other to create a 3D model. Shown below are sagittal (bottom left) and coronal (bottom right) images cut through the fully segmented cranial bone marrow after 3D reconstruction. After segmentation, the image data were analyzed in Mathcad for T1, T2, and secular-T2 relaxation times and volume. |
Software for MR Image Overlay Guided Needle Insertions: The Clinical Translation Process
|
Publication: Proc. SPIE 8671, Medical Imaging 2013: Image-Guided Procedures, Robotic Interventions, and Modeling, 867116 (March 12, 2013). Authors: Ungi T, U-Thainual P, FritzJ, Iordachita II, Flammang AJ, Carrino JA, Fichtinger G. Institution: School of Computing, Queen's University, Kingston, ON, Canada. Background/Purpose: Needle guidance software using augmented reality image overlay was translated from the experimental phase to support preclinical and clinical studies. Major functional and structural changes were needed to meet clinical requirements. We present the process applied to fulfill these requirements, and selected features that may be applied in the translational phase of other image-guided surgical navigation systems. Methods: We used an agile software development process for rapid adaptation to unforeseen clinical requests. The process is based on iterations of operating room test sessions, feedback discussions, and software development sprints. The open-source application framework of 3D Slicer and the NA-MIC kit provided sufficient flexibility and stable software foundations for this work. Results: All requirements were addressed in a process with 19 operating room test iterations. Most features developed in this phase were related to workflow simplification and operator feedback. Conclusion: Efficient and affordable modifications were facilitated by an open source application framework and frequent clinical feedback sessions. Results of cadaver experiments show that software requirements were successfully solved after a limited number of operating room tests. |
Analysis of Conventional Swept-source OCT of Subglottic Stenosis in a Rabbit Model
|
Publication: Proc. SPIE 8565, Photonic Therapeutics and Diagnostics IX, 856521 (March 8, 2013). Authors: Hamamoto A, Su E, Peaks Y, Chen Z, Wong BJF. Institution: Beckman Laser Institute and Medical Clinic, Irvine, CA, USA. Background/Purpose: Acquired subglottic stenosis is a narrowing of the airway caused by prolonged endotracheal intubation. Currently, there are no non-invasive means to diagnose the disease. A previous study by this same group introduced optical coherence tomography (OCT) as a means of monitoring the progression of stenosis. The aim of the current study was to qualitatively and quantitatively analyze OCT images obtained from a subglottic stenosis model of the rabbit airway. 15 rabbits were used throughout the study, and a MEMs based OCT probe was utilized. The OCT images obtained were analyzed using a free software program, 3D Slicer. The region of scarred tissue was grown out and measured quantitatively. This study demonstrated the feasibility of using a program to quantify the progression of scarring in OCT images, in addition to qualitatively correlating between histology, endoscopic, and OCT images. Future works may include utilization of a long-range probe and use of a pressure necrosis model to better emulate the actual onset of neonatal subglottic stenosis. |
Three-dimensional Volumetric Rendition of Cannon Ball Pulmonary Metastases by the Use of 3D Slicer, an Open Source Free Software Package
|
Publication: BMJ Case Rep. 2013 Feb 4;2013. PMID: 23386494 | PDF Authors: Revannasiddaiah S, Susheela SP, Madhusudhan N, Mallarajapatna GJ. Institution: Department of Radiation Oncology, HealthCare Global-Bangalore Institute of Oncology, Bengaluru, Karnataka, India. Background/Purpose: A gentleman treated 6 years ago for colonic carcinoma (stage-IIA) had been on regular follow-up for a span of 4 years, when he was apparently disease-free. After being lost to follow-up in the past 2 years, he was recently diagnosed with a pathological fracture of the seventh thoracic vertebra for which he underwent surgery (vertebral fixation and cord decompression) on an emergency basis. Postoperatively, he underwent a CT simulation of the thorax with the purpose of planning radiotherapy (RT) to the involved vertebrae. The CT-scan demonstrated multiple bilateral pulmonary nodules. After palliative RT to the involved vertebral column, in the interest of academics, we utilised the CT-scan data for volumetric reconstructions to attempt a better depiction of the well-known phenomenon of ‘cannon ball metastases’. This was achieved by the use of 3D Slicer 4.2, an open source software package (distributed under a BSD-style open source license) intended for advanced visualization and analysis of medical image datasets. This, to our knowledge, is possibly the first publication providing a three-dimensional depiction of ‘cannon ball’ pulmonary metastases. |
In Vivo Imaging of Dopaminergic Neurotransmission after Transient Focal Ischemia in Rats
|
Publication: J Cereb Blood Flow Metab. 2013 Feb;33(2):244-52. PMID: 23149560 | PDF Authors: Martín A, Gómez-Vallejo V, San Sebastián E, Padró D, Markuerkiaga I, Llarena I, Llop J. Institution: Molecular Imaging Unit, CIC biomaGUNE, San Sebastián, Spain. Background/Purpose: The precise biologic mechanisms involved in functional recovery processes in response to stroke such as dopaminergic neurotransmission are still largely unknown. For this purpose, we performed in parallel in vivo magnetic resonance imaging and positron emission tomography (PET) with [(18)F]fluorodeoxyglucose ([(18)F]FDG) and [(11)C]raclopride at 1, 3, 7, 14, 21, and 28 days after middle cerebral artery occlusion in rats. In the ischemic territory, PET [(18)F]FDG showed a initial decrease in cerebral metabolism followed by a time-dependent recovery to quasi-normal values at day 14 after ischemia. The PET with [(11)C]raclopride, a ligand for dopamine D(2) receptor, showed a sustained binding during the first week after ischemia that declined dramatically from day 14 to day 28. Interestingly, a slight increase in [(11)C]raclopride binding was observed at days 1 to 3 followed by the uppermost binding at day 7 in the contralateral territory. Likewise, in vitro autoradiography using [(3)H]raclopride confirmed these in vivo results. Finally, the neurologic test showed major neurologic impairment at day 1 followed by a recovery of the cerebral function at day 28 after cerebral ischemia. Taken together, these results might suggest that dopamine D(2) receptor changes in the contralateral hemisphere could have a key role in functional recovery after cerebral ischemia. |
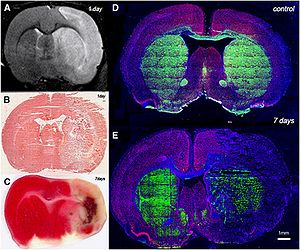 Brain lesion evolution after cerebral ischemia. magnetic resonance imaging (MRI) alterations in T2-weighted (T2W) signal (A) and hematoxyline-eosine stained brain section at day 1 after reperfusion (B). 2,3,5-Triphenyltetrazolium chloride (TTC) stained section at day 7 (C). Immunofluorescent labeling of tyrosine hydroxylase (TH) (green), NeuN (red), and 4′-6′-diamidino-2-phenylindole (DAPI) (blue) of an axial section of a control brain (D) and at day 7 after cerebral ischemia (E). Regions of interest were manually defined using the Open Source software 3D Slicer image analysis software (Version 3.6.3. for each rat on the region of increased signal in the ipsilateral hemisphere. |
MRI Evidence for Altered Venous Drainage and Intracranial Compliance in Mild Traumatic Brain Injury
|
Publication: PLoS One. 2013 Feb;8(2):e55447. PMID: 23405151 | PDF Authors: Pomschar A, Koerte I, Lee S, Laubender RP, Straube A, Heinen F, Ertl-Wagner B, Alperin N. Institution: Institute of Clinical Radiology, University of Munich - Grosshadern Campus, Ludwig-Maximilians-University, Munich, Germany. Background/Purpose: To compare venous drainage patterns and associated intracranial hydrodynamics between subjects who experienced mild traumatic brain injury (mTBI) and age- and gender-matched controls. Thirty adult subjects (15 with mTBI and 15 age- and gender-matched controls) were investigated using a 3T MR scanner. Time since trauma was 0.5 to 29 years (mean 11.4 years). A 2D-time-of-flight MR-venography of the upper neck was performed to visualize the cervical venous vasculature. Cerebral venous drainage through primary and secondary channels, and intracranial compliance index and pressure were derived using cine-phase contrast imaging of the cerebral arterial inflow, venous outflow, and the craniospinal CSF flow. The intracranial compliance index is the defined as the ratio of maximal intracranial volume and pressure changes during the cardiac cycle. MR estimated ICP was then obtained through the inverse relationship between compliance and ICP. Funding:
|
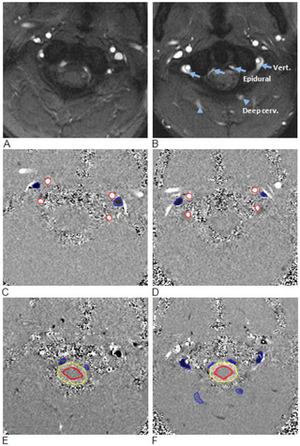 Examples of high and low velocity encoded phase contrast images from a control subject (left) and a subject with mTBI (right). A–B: Flow compensated magnitude images showing the bright signal from blood vessels. The augmented venous outflow through the epidural, vertebral veins (arrows) and the deep cervical veins (arrow heads) is well visualized. C–D: High-velocity encoding images used for measurements of arterial inflow and venous outflow through the jugular veins. E–F: Low-velocity encoding images used for measurements of the flow through the secondary channels (epidural, vertebral, and deep cervical veins) and the CSF flow. The lumen boundaries (red – arteries, blue- veins and yellow and red – CSF and cord) were identified using the PUBS automated segmentation method. |
A Robust Variational Approach for Simultaneous Smoothing and Estimation of DTI
|
Publication: Neuroimage. 2013 Feb 15;67:33-41. PMID: 23165324 | PDF Authors: Liu M, Vemuri BC, Deriche R. Institution: Siemens Corporate Research & Technology, Princeton, NJ, USA. Background/Purpose: Estimating diffusion tensors is an essential step in many applications - such as diffusion tensor image (DTI) registration, segmentation and fiber tractography. Most of the methods proposed in the literature for this task are not simultaneously statistically robust and feature preserving techniques. In this paper, we propose a novel and robust variational framework for simultaneous smoothing and estimation of diffusion tensors from diffusion MRI. Our variational principle makes use of a recently introduced total Kullback-Leibler (tKL) divergence for DTI regularization. tKL is a statistically robust dissimilarity measure for diffusion tensors, and regularization by using tKL ensures the symmetric positive definiteness of tensors automatically. Further, the regularization is weighted by a non-local factor adapted from the conventional non-local means filters. Finally, for the data fidelity, we use the nonlinear least-squares term derived from the Stejskal-Tanner model. We present experimental results depicting the positive performance of our method in comparison to competing methods on synthetic and real data examples. Funding:
|
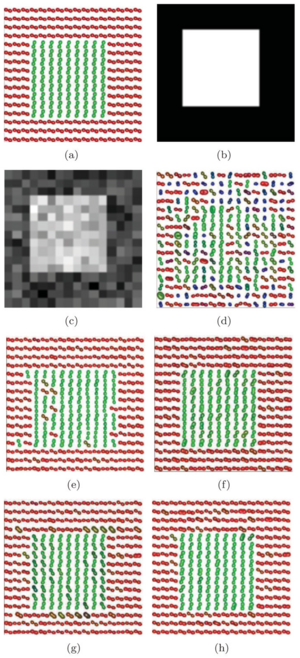 (a) Ground truth synthetic DTI field, (b) the original DWI corresponding to g1, (c) the Rician noise affected DWI, the DTI estimation using (d) MRE, (e) VF, (f) LMMSE, (g) NLM, and (h) the proposed technique. For LMMSE, we used the implementation in 3D Slicer 3.6. |
Augmented Reality Visualization Using an Image Overlay System for MR-guided Interventions: Technical Performance of Spine Injection Procedures in Human Cadavers at 1.5 Tesla
|
Publication: Eur Radiol. 2013 Jan;23(1):235-45. PMID: 22797956 Authors: Fritz J, U-Thainual P, Ungi T, Flammang AJ, Fichtinger G, Iordachita II, Carrino JA. Institution: Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins University School of Medicine, Baltimore, MD, USA. Background/Purpose: To prospectively assess the technical performance of an augmented reality system for MR-guided spinal injection procedures. The augmented reality system was used with a clinical 1.5-T MRI system. A total of 187 lumbosacral spinal injection procedures (epidural injection, spinal nerve root injection, facet joint injection, medial branch block, discography) were performed in 12 human cadavers. Needle paths were planned with the Perk Station module of 3D Slicer software on high-resolution MR images. Needles were placed under augmented reality MRI navigation. MRI was used to confirm needle locations. T1-weighted fat-suppressed MRI was used to visualize the injectant. Outcome variables assessed were needle adjustment rate, inadvertent puncture of non-targeted structures, successful injection rate and procedure time. Needle access was achieved in 176/187 (94.1 %) targets, whereas 11/187 (5.9 %) were inaccessible. Six of 11 (54.5 %) L5-S1 disks were inaccessible, because of an axial obliquity of 30˚ (27˚-34˚); 5/11 (45.5 %) facet joints were inaccessible because of osteoarthritis or fusion. All accessible targets (176/187, 94.1 %) were successfully injected, requiring 47/176 (26.7 %) needle adjustments. There were no inadvertent punctures of vulnerable structures. Median procedure time was 10.2 min (5-19 min). Image overlay navigated MR-guided spinal injections were technically accurate. Disks with an obliquity ≥27˚ may be inaccessible. Funding:
|
2012
Comparative Evaluation of Mitral Valve Strain by Deformation Tracking in 3D-Echocardiography
|
Publication: Cardiovascular Engineering and Technology 2012 Dec, 3(4):402-12. | PDF Authors: Zekry B, Lawry G, Little S, Zoghbi W, Freeman J, Jajoo a, Jain s, He J, Martynenko A, Azencott R. Institution: The Methodist Hospital Research Institute, Houston, TX. Background/Purpose: We present new algorithms to compute patient specific strain maps for mitral valve leaflets, by tracking and modeling deformations of the mitral valve apparatus in 3D echocardiography. We can then quantify comparisons of mitral leaflets strain maps between normal patients and cases of mitral valve prolapse or regurgitation. For patients with mitral valve regurgitation, we compare mitral leaflets strain maps between pre-surgery and post-surgery, to quantify the strain reduction due to mitral valve repair surgery. Funding:
|
Perk Tutor: An Open-source Training Platform for Ultrasound-guided Needle Insertions
|
Publication: IEEE Trans Biomed Eng. 2012 Dec;59(12):3475-81. PMID: 23008243 Authors: Ungi T, Sargent D, Moult E, Lasso A, Pinter C, McGraw RC, Fichtinger G. Institution: School of Computing, Queen's University, Kingston, ON, Canada. Background/Purpose: mage-guided needle placement, including ultrasound (US)-guided techniques, have become commonplace in modern medical diagnosis and therapy. To ensure that the next generations of physicians are competent using this technology, efficient and effective educational programs need to be developed. This paper presents the Perk Tutor: a configurable, open-source training platform for US-guided needle insertions. The Perk Tutor was successfully tested in three different configurations to demonstrate its adaptability to different procedures and learning objectives. 1) The Targeting Tutor, designed to develop US-guided needle targeting skills, 2) the Lumbar Tutor, designed for practicing US-guided lumbar spinal procedures, and (3) the Prostate Biopsy Tutor, configured for US-guided prostate biopsies. The Perk Tutor provides the trainee with quantitative feedback on progress toward the specific learning objectives of each configuration. Configurations were implemented through simple rearrangement of hardware and software components, attesting to the modularity and ease of configuration. The Perk Tutor is provided as a free resource to enable research and development of educational programs for US-guided intervention. |
Pituitary Adenoma Volumetry with 3D Slicer
|
Publication: PLoS One. 2012 Dec;7(12):e51788. PMID: 23240062 | PDF Authors: Egger J, Kapur T, Nimsky C, Kikinis R. Institution: Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: In this study, we present pituitary adenoma volumetry using the free and open source medical image computing platform for biomedical research: 3D Slicer. Volumetric changes in cerebral pathologies like pituitary adenomas are a critical factor in treatment decisions by physicians and in general the volume is acquired manually. Therefore, manual slice-by-slice segmentations in magnetic resonance imaging (MRI) data, which have been obtained at regular intervals, are performed. In contrast to this manual time consuming slice-by-slice segmentation process, 3D Slicer is an alternative which can be significantly faster and less user intensive. In this contribution, we compare pure manual segmentations of ten pituitary adenomas with semi-automatic segmentations with 3D Slicer. Thus, physicians drew the boundaries completely manually on a slice-by-slice basis and performed a Slicer-enhanced segmentation using the competitive region-growing based module of 3D Slicer named GrowCut. Results showed that the time and user effort required for GrowCut-based segmentations were on average about thirty percent less than the pure manual segmentations. Furthermore, we calculated the Dice Similarity Coefficient (DSC) between the manual and the Slicer-based segmentations to proof that the two are comparable yielding an average DSC of 81.9763.39%. Funding:
|
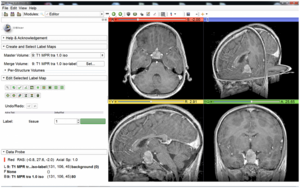 3D Slicer interface with the Slicer-Editor on the left side and a loaded pituitary adenoma data set on the right side: axial slice (upper left window), sagittal slice (lower left window), coronal slice (lower right window) and the three slices shown in a 3D visualization (upper right window). |
Differences in Simple Morphological Variables in Ruptured and Unruptured Middle Cerebral Artery Aneurysms
|
Publication: J Neurosurg. 2012 Nov;117(5):913-9. PMID: 22957531 | PDF Authors: Lin N, Ho A, Gross BA, Pieper S, Frerichs KU, Day AL, Du R. Institution: Department of Neurosurgery, and Surgical Planning Laboratory, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Object Management of unruptured intracranial aneurysms remains controversial in neurosurgery. The contribution of morphological parameters has not been included in the treatment paradigm in a systematic manner or for any particular aneurysm location. The authors present a large sample of middle cerebral artery (MCA) aneurysms that were assessed using morphological variables to determine the parameters associated with aneurysm rupture. Methods: Preoperative CT angiography (CTA) studies were evaluated using 3D Slicer software to generate 3D models of the aneurysms and their surrounding vascular architecture. Morphological parameters examined in each model included 5 variables already defined in the literature (aneurysm size, aspect ratio, aneurysm angle, vessel angle, and size ratio) and 3 novel variables (flow angle, distance to the genu, and parent-daughter angle). Univariate and multivariate statistical analyses were performed to determine statistical significance. Results Between 2005 and 2008, 132 MCA aneurysms were treated at a single institution, and CTA studies of 79 aneurysms (40 ruptured and 39 unruptured) were analyzed. Fifty-three aneurysms were excluded because of reoperation (4), associated AVM (2), or lack of preoperative CTA studies (47). Ruptured aneurysms were associated with larger size, greater aspect ratio, larger aneurysm and flow angles, and smaller parent-daughter angle. Multivariate logistic regression revealed that aspect ratio, flow angle, and parent-daughter angle were the strongest factors associated with ruptured aneurysms. Aspect ratio, flow angle, and parent-daughter angle are more strongly associated with ruptured MCA aneurysms than size. The association of parameters independent of aneurysm morphology with ruptured aneurysms suggests that these parameters may be associated with an increased risk of aneurysm rupture. These factors are readily applied in clinical practice and should be considered in addition to aneurysm size when assessing the risk of aneurysm rupture specific to the MCA location. Funding:
|
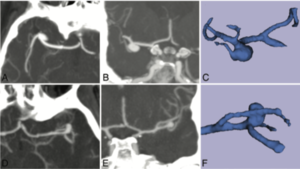 Computed tomography angiograms and 3D models of unruptured and ruptured aneurysms. A and B: Axial (A) and coronal (B) MIP images showing an unruptured right MCA aneurysm. D and E: Axial (D) and coronal (E) MIP images showing a ruptured left MCA aneurysm. C and F: Corresponding 3D reconstructed 3D Slicer images. |
3D Slicer as an Image Computing Platform for the Quantitative Imaging Network
|
Publication: Magn Reson Imaging. 2012 Nov;30(9):1323-41. PMID: 22770690 | PDF Authors: Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin JC, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M, Buatti J, Aylward S, Miller JV, Pieper S, Kikinis R. Institution: Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Quantitative analysis has tremendous but mostly unrealized potential in healthcare to support objective and accurate interpretation of the clinical imaging. In 2008, the National Cancer Institute began building the Quantitative Imaging Network (QIN) initiative with the goal of advancing quantitative imaging in the context of personalized therapy and evaluation of treatment response. Computerized analysis is an important component contributing to reproducibility and efficiency of the quantitative imaging techniques. The success of quantitative imaging is contingent on robust analysis methods and software tools to bring these methods from bench to bedside. 3D Slicer is a free open-source software application for medical image computing. As a clinical research tool, 3D Slicer is similar to a radiology workstation that supports versatile visualizations but also provides advanced functionality such as automated segmentation and registration for a variety of application domains. Unlike a typical radiology workstation, 3D Slicer is free and is not tied to specific hardware. As a programming platform, 3D Slicer facilitates translation and evaluation of the new quantitative methods by allowing the biomedical researcher to focus on the implementation of the algorithm and providing abstractions for the common tasks of data communication, visualization and user interface development. Compared to other tools that provide aspects of this functionality, 3D Slicer is fully open source and can be readily extended and redistributed. In addition, 3D Slicer is designed to facilitate the development of new functionality in the form of 3D Slicer extensions. In this paper, we present an overview of 3D Slicer as a platform for prototyping, development and evaluation of image analysis tools for clinical research applications. To illustrate the utility of the platform in the scope of QIN, we discuss several use cases of 3D Slicer by the existing QIN teams, and we elaborate on the future directions that can further facilitate development and validation of imaging biomarkers using 3D Slicer. Funding:
|
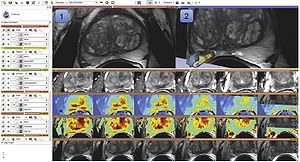 Visualization capabilities and 3D Slicer user interface are utilized for exploration of the multiparametric MRI of the prostate. The T2w MR scans (top left image and the bottom row of consecutive slices) provide anatomical detail and context for interpretation of the registered ADC map (first row of the image matrix) calculated from the DWI and various pharmacokinetic maps computed from DCE MRI, as shown in the 2D axial slice viewer (marked by “1”) and the Compare View layout below. Spatial context of the annotated tumor ROI is provided by composed view of the tumor ROI surface and the T2w image cross-section in the 3D viewer (marked by “2”). |
SlicerRT: Radiation Therapy Research oolkit for 3D Slicer
|
Publication: Med Phys. 2012 Oct;39(10):6332-8. PMID: 23039669 | PDF Authors: Pinter C, Lasso A, Wang A, Jaffray D, Fichtinger G. Institution: School of Computing, Queen's University, Kingston, ON, Canada. Background/Purpose: Interest in adaptive radiation therapy research is constantly growing, but software tools available for researchers are mostly either expensive, closed proprietary applications, or free open-source packages with limited scope, extensibility, reliability, or user support. To address these limitations, we propose SlicerRT, a customizable, free, and open-source radiation therapy research toolkit. SlicerRT aspires to be an open-source toolkit for RT research, providing fast computations, convenient workflows for researchers, and a general image-guided therapy infrastructure to assist clinical translation of experimental therapeutic approaches. It is a medium into which RT researchers can integrate their methods and algorithms, and conduct comparative testing. SlicerRT was implemented as an extension for the widely used 3D Slicer medical image visualization and analysis application platform. SlicerRT provides functionality specifically designed for radiation therapy research, in addition to the powerful tools that 3D Slicer offers for visualization, registration, segmentation, and data management. The feature set of SlicerRT was defined through consensus discussions with a large pool of RT researchers, including both radiation oncologists and medical physicists. The development processes used were similar to those of 3D Slicer to ensure software quality. Standardized mechanisms of 3D Slicer were applied for documentation, distribution, and user support. The testing and validation environment was configured to automatically launch a regression test upon each software change and to perform comparison with ground truth results provided by other RT applications. Modules have been created for importing and loading DICOM-RT data, computing and displaying dose volume histograms, creating accumulated dose volumes, comparing dose volumes, and visualizing isodose lines and surfaces. The effectiveness of using 3D Slicer with the proposed SlicerRT extension for radiation therapy research was demonstrated on multiple use cases. A new open-source software toolkit has been developed for radiation therapy research. SlicerRT can import treatment plans from various sources into 3D Slicer for visualization, analysis, comparison, and processing. The provided algorithms are extensively tested and they are accessible through a convenient graphical user interface as well as a flexible application programming interface. |
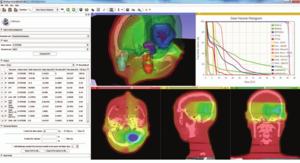 Dose volume histogram module in a standard 3D Slicer layout with basic visualization. The module toolbox can be seen on the left side, and the DVH chart is found in the upper right corner. |
Developmental Trajectories of Amygdala and Hippocampus from Infancy to Early Adulthood in Healthy Individuals
|
Publication: PLoS One. 2012 Oct;7(10):e46970. PMID: 23056545 | PDF Authors: Uematsu A, Matsui M, Tanaka C, Takahashi T, Noguchi K, Suzuki M, Nishijo H. Institution: Department of Psychology, Graduate School of Medicine and Pharmaceutical Sciences, University of Toyama, Toyama, Japan. Background/Purpose: Knowledge of amygdalar and hippocampal development as they pertain to sex differences and laterality would help to understand not only brain development but also the relationship between brain volume and brain functions. However, few studies investigated development of these two regions, especially during infancy. The purpose of this study was to examine typical volumetric trajectories of amygdala and hippocampus from infancy to early adulthood by predicting sexual dimorphism and laterality. We performed a cross-sectional morphometric MRI study of amygdalar and hippocampal growth from 1 month to 25 years old, using 109 healthy individuals. The findings indicated significant non-linear age-related volume changes, especially during the first few years of life, in both the amygdala and hippocampus regardless of sex. The peak ages of amygdalar and hippocampal volumes came at the timing of preadolescence (9-11 years old). The female amygdala reached its peak age about one year and a half earlier than the male amygdala did. In addition, its rate of growth change decreased earlier in the females. Furthermore, both females and males displayed rightward laterality in the hippocampus, but only the males in the amygdala. The robust growth of the amygdala and hippocampus during infancy highlight the importance of this period for neural and functional development. The sex differences and laterality during development of these two regions suggest that sex-related factors such as sex hormones and functional laterality might affect brain development. Funding:
|
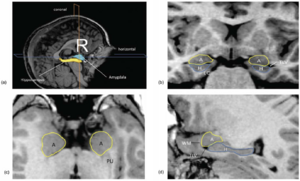 Orthogonal views for segmenting the amygdala and hippocampus on MRI sections. A three-dimensional reconstruction of images (a) in which lines indicate the position of the horizontal plane (b), sagittal plane (c), and coronal plane (d) is shown. A, Amygdala; EC, entorhinal cortex; H, hippocampus; PU, putamen; TLV, temporal horn of the lateral ventricle; WM, subamygdaloid white matter. For the amygdala and hippocampus volumes, the images were imported into the 3D Slicer software and manually defined. |
Extra-Hippocampal Subcortical Limbic Involvement Predicts Episodic Recall Performance in Multiple Sclerosis
|
Publication: PLoS One. 2012 Oct;7(10):e44942. PMID: 23056187 | PDF Authors: Dineen RA, Bradshaw CM, Constantinescu CS, Auer DP. Institution: Division of Radiological and Imaging Sciences, University of Nottingham, Nottingham, UK. Background/Purpose: Episodic memory impairment is a common but poorly-understood phenomenon in multiple sclerosis (MS). We aim to establish the relative contributions of reduced integrity of components of the extended hippocampal-diencephalic system to memory performance in MS patients using quantitative neuroimaging. 34 patients with relapsing-remitting MS and 24 healthy age-matched controls underwent 3 T MRI including diffusion tensor imaging and 3D T1-weighted volume acquisition. Manual fornix regions-of-interest were used to derive fornix fractional anisotropy (FA). Normalized hippocampal, mammillary body and thalamic volumes were derived by manual segmentation. MS subjects underwent visual recall, verbal recall, verbal recognition and verbal fluency assessment. Significant differences between MS patients and controls were found for fornix FA (0.38 vs. 0.46, means adjusted for age and fornix volume, P<.0005) and mammillary body volumes (age-adjusted means 0.114 ml vs. 0.126 ml, P<.023). Multivariate regression analysis identified fornix FA and mammillary bodies as predictor of visual recall (R(2) = .31, P = .003, P = .006), and thalamic volume as predictive of verbal recall (R(2) = .37, P<.0005). No limbic measures predicted verbal recognition or verbal fluency. These findings indicate that structural and ultrastructural alterations in subcortical limbic components beyond the hippocampus predict performance of episodic recall in MS patients with mild memory dysfunction. Funding:
|
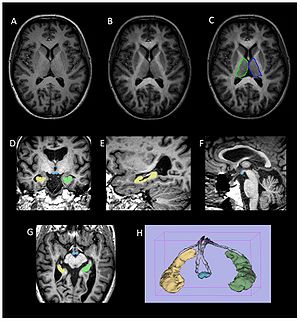 Volumetric segmentation of brain images. (a–c) Thalamic segmentation. Axial MPRAGE image from a control subject (a) before and (b) after the addition of FA weighting from the co-registered FA image. Note the increase in clarity of the lateral border of the thalamus that facilitates (c) manual segmentation of the thalamus. (d–g) axial, coronal and sagittal images from a participant with MS demonstrating ROIs drawn for the mammillary bodies (blue) and right (yellow) and left (green) hippocampi. (h) Surface rendered representation of the segmented hippocampi and mammillary bodies from a participant with MS. The manually defined fornix ROI used to derive fornix FA is also shown (grey). Volumes of the hippocampi, mammillary bodies and thalami were obtained manually from the MPRAGE images using 3D Slicer software |
Advanced Neuroimaging in Traumatic Brain Injury
|
Publication: Semin Neurol. 2012 Sep;32(4):374-400. PMID: 23361483 | PDF Authors: Edlow BL, Wu O. Institution: Department of Neurology, Massachusetts General Hospital, Boston, MA, USA. Background/Purpose: Advances in structural and functional neuroimaging have occurred at a rapid pace over the past two decades. Novel techniques for measuring cerebral blood flow, metabolism, white matter connectivity, and neural network activation have great potential to improve the accuracy of diagnosis and prognosis for patients with traumatic brain injury (TBI), while also providing biomarkers to guide the development of new therapies. Several of these advanced imaging modalities are currently being implemented into clinical practice, whereas others require further development and validation. Ultimately, for advanced neuroimaging techniques to reach their full potential and improve clinical care for the many civilians and military personnel affected by TBI, it is critical for clinicians to understand the applications and methodological limitations of each technique. In this review, we examine recent advances in structural and functional neuroimaging and the potential applications of these techniques to the clinical care of patients with TBI. We also discuss pitfalls and confounders that should be considered when interpreting data from each technique. Finally, given the vast amounts of advanced imaging data that will soon be available to clinicians, we discuss strategies for optimizing data integration, visualization, and interpretation. Funding:
|
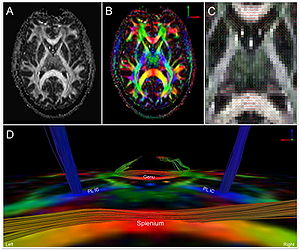 DTI and diffusion tensor tractography in a 32-year-old healthy man. Greyscale FA map (A), color-coded FA map (B), and color-coded principle eigenvector (i.e. tensor) map (C) are displayed in the axial plane at the level of the mid-thalami. A diffusion tensor tractography analysis is shown in (D) from a posterior perspective, superimposed on the axial color FA map shown in (B). In (A), the signal intensity of the FA map corresponds to the magnitude of the FA in each voxel, on a scale from 0 (black) to 1 (white). In (B, C, and D), color-coding is according to convention, with medial-lateral fibers coded red, anterior-posterior fibers coded green, and superior-inferior fibers coded blue. In (D), fiber tracts were reconstructed with TrackVis software using a deterministic, streamline tractography model. Tract termination criteria included FA < 0.2 and intervoxel angle curvature > 60 degrees. Fiber tracts in the splenium were generated using a single voxel region of interest (ROI) that was manually traced at the center of the splenium. Fiber tracts in the bilateral posterior limbs of the internal capsule (PL IC) were also generated using single voxel ROIs traced at the centers of the PL IC. Tracts in the genu were generated using a single voxel ROI traced in the forceps minor fasciculus of the right frontal lobe. |
Posterior Vaginal Prolapse Shape and Position Changes at Maximal Valsalva Seen in 3D MRI-based Models
|
Publication: Int Urogynecol J. 2012 Sep;23(9):1301-6. PMID: 22527556 | PDF Authors: Luo J, Larson KA, Fenner DE, Ashton-Miller JA, Delancey JO. Institution: Pelvic Floor Research Group, University of Michigan, Ann Arbor, MI, USA. Background/Purpose: Two-dimensional magnetic resonance imaging (MRI) of posterior vaginal prolapse has been studied. However, the three-dimensional (3D) mechanisms causing such prolapse remain poorly understood. This discovery project was undertaken to identify the different 3D characteristics of models of rectocele-type posterior vaginal prolapse (PVP(R)) in women. Ten women with (cases) and ten without (controls) PVP(R) were selected from an ongoing case-control study. Supine, multiplanar MR imaging was performed at rest and maximal Valsalva. Three-dimensional reconstructions of the posterior vaginal wall and pelvic bones were created using 3D Slicer v.3.4.1. In each slice the posterior vaginal wall and perineal skin were outlined to the anterior margin of the external anal sphincter to include the area of the perineal body. Women with predominant enteroceles or anterior vaginal prolapse were excluded. The case and control groups had similar demographics. In women with PVP(R) two characteristics were consistently visible (10/10): (1) the posterior vaginal wall displayed a folding phenomenon similar to a person beginning to kneel ("kneeling" shape) and (2) a downward displacement in the upper two thirds of the vagina. Also seen in some, but not all of the scans were: (3) forward protrusion of the distal vagina (6/10), (4) perineal descent (5/10), and (5) distal widening in the lower third of the vagina (3/10). Increased folding (kneeling) of the vagina and an overall downward displacement are consistently present in rectocele. Forward protrusion, perineal descent, and distal widening are sometimes seen as well. Funding:
|
Talairach Methodology in the Multimodal Imaging and Robotics Era
|
Publication: Book Chapter in: Jean-Marie Scarabin Ed. Stereotaxy and Epilepsy Surgery. John Libbey Eurotext LTD. 2012 Sep; p.245-72. ISBN-10: 2742007679. Authors: Cardinale F, Miserocchi A, Moscato A, Cossu M, Castana L, Schiariti M P, Gozzo F, Pero G, Quilici L, Citterio A, Minella M, Torresin A, Lo Russo G. Institution: Centro Claudio Munari per la Chirurgica dell' Epilessia e del Parkinson, Ospedale Niguarda Ca' Grande, Milan, Italy. Background/Purpose: The original Talairach methodology was based on three main features. Neuroimaging techniques to collect patient-specific brain anatomical data, a probabilistic morpho-functional atlas and surgical tools developed to implant intracerebral electrodes in accurate and safe conditions. Brain anatomy was obtained indirectly by means of cerebral angiography and ventriculography. Both techniques were performed in stereotactic (coordinate system), telemetric (reduced magnification and distortion) and stereoscopic (pseudo-3D effect) conditions. The following step was to normalize patient’s specific data to the atlas space using the bicommissural coordinate system. The normalization to the atlas was fundamental in order to integrate the images with structural (gyri and sulci), cytoarchitectural (Brodmann areas) and functional (electrical stimulations) data. Then, in order to position the guiding screws along the pre-planned trajectory, a double grid was attached onto the frame, allowing drilling in the orthogonal direction. Nowadays modern technological tools facilitate the workflow, but the main concepts of this methodology are still valid. We use algorithms completely automated with software applications to expand the multimodal integration of data so that MRI, rotational angiography, fMRI and DTI-FT data can all be coregistered together. It is now possible to obtain real 3D viewing by multi-planar reconstructions (MPR), volume and surface rendering. The tool holder for the surgical implantation is now fixed onto the passive robotic arm of the stereotactic image-guided system Renishaw neuromate®, so that the number of possible trajectories is no more discrete (as using the double grid), but virtually infinite with any desired obliquity. The aim of this chapter is to describe our present workflow. We will underline the methodological continuity with basic Talairach and Bancaud principles, highlighting how modern tools can help in saving time and improve safety, accuracy and the amount of information. Moreover, we report our quantitative results regarding geometrical accuracy at the cortical entry point with this new methodology. |
 3D Slicer scene with MPR and 3D views (crossed viewing) During long-term Video-SEEGmonitoring, for several days following implantation, it is important to have intuitive and accurate mapping tools for localizing the sources of the signal. In order to reach this aim, we integrate all the information in 3D Slicer, a package able to load all data. It is in fact possible to import all datasets and surface models computed by FreeSurfer (white and gray matter, with parcellations and labels). Moreover, it is possible to create other models such as the vascular tree and the electrodes leads. This is done very simply with the Gray Scale Model Maker tool. 3D Slicer is installed on all team members’ computers, so that epileptologists are able to look at these scenes when interpreting the SEEG traces. (A and B) constitute a pair of stereoscopic images with the reconstruction of pial surface, vessels and labeled electrodes. (C, D and E) are the MPR views, with the visualization fading 50% for MRI and 50% for post-implant O-arm dataset. The crosshair indicates the second lead of an electrode exploring first temporal gyrus, temporal transverse gyri and insular long gyri. |
SARRP Dose Planning System
|
Company: Xstrahl Ltd., Camberley, UK. Background: The SARRP dose planning system (DPS) is a dedicated in vivo treatment planning system designed to calculate dose distributions in pre-clinical radiation studies. The SARRP DPS is specifically validated for use with in vivo—uniquely enabling the user to treat very precise areas of the animal by defining the area and visualizing the dose and as a result, enabling a more accurate experiment and final result. More... |
Three-dimensional Image Quantification as a New Morphometry Method for Microvascular Tissue Engineering
|
Publication: Tissue Eng Part C Methods. 2012 Jul;18(7):507-16. PMID: 22224751 | PDF Authors: Rytlewski JA, Geuss LR, Anyaeji CI, Lewis EW, Suggs L. Institution: University of Texas at Austin, Biomedical Engineering, Austin, TX, USA. Background/Purpose: Morphological analysis is an essential step in verifying the success of a tissue engineering strategy where researchers must determine the presence of a desired cellular phenotype. While morphometry has transitioned from observational grading to computational quantification, established quantitative methods eliminate information by relying on two-dimensional (2D) analysis to describe three-dimensional (3D) niches. In this study, we demonstrate the validity and utility of 3D morphological quantification using two common angiogenesis assays in our fibrin-based in vitro model: (1) the microcarrier bead assay with human mesenchymal stem cells and (2) the rat aortic ring outgrowth assay. The quantification method is based on collecting and segmenting fluorescent confocal z-stacks into 3D models with 3D Slicer, an open-source MRI/CT analysis program. Data from 3D models are then processed into biologically relevant metrics in MATLAB for statistical analysis. Metrics include descriptive parameters such as vascular network length, volume, number of network segments, and degree of network branching. Our results indicate that 2D measures are significantly different than their 3D counterparts unless the vascular network exhibits anisotropic growth along the plane of imaging. Additionally, the statistical outcomes of 3D morphological quantification agreed with our initial qualitative observations among different test groups. This novel quantification approach generates more spatially accurate and objective measures, representing an important step towards improving the reliability of morphological comparisons. |
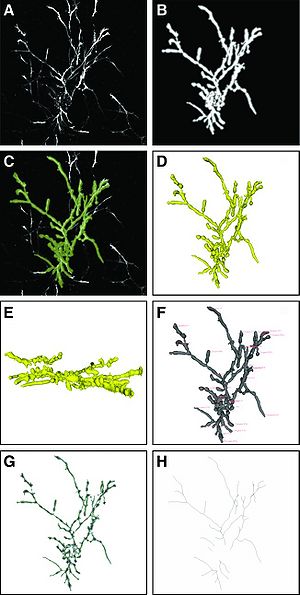 Image processing steps in three-dimensional 3D Slicer's Vascular Modeling Toolkit. Sample shown is from the 10 mg/mL PEGylated fibrin group. (A) Z-projection of the original confocal volume using standard deviation of pixel values; (B) Z-projection of the enhanced confocal volume after applying Frangi's vesselness; (C) image from (A) with overlay of segmented 3D model in green; (D, E) evolved model from (C) shown in the XY- and YZ-planes, respectively; (F) evolved model with source and target fiducial placement; (G) Voronoi diagram of evolved model; (H) centerlines skeleton extracted from (G). |
Prostate: Registration of Digital Histopathologic Images to in Vivo MR Images Acquired by Using Endorectal Receive Coil
|
Publication: Radiology. 2012 Jun;263(3):856-64. PMID: 22474671 | PDF Authors: Ward AD, Crukley C, McKenzie CA, Montreuil J, Gibson E, Romagnoli C, Gomez JA, Moussa M, Chin J, Bauman G, Fenster A. Institution: Imaging Research Laboratories, Robarts Research Institute, Schulich School of Medicine and Dentistry, University of Western Ontario, London, ON, Canada. Background/Purpose: To develop and evaluate a technique for the registration of in vivo prostate magnetic resonance (MR) images to digital histopathologic images by using image-guided specimen slicing based on strand-shaped fiducial markers relating specimen imaging to histopathologic examination.The study was approved by the institutional review board (University of Western Ontario Health Sciences Research Ethics Board, London, Ontario, Canada), and written informed consent was obtained from all patients. This work proposed and evaluated a technique utilizing developed fiducial markers and real-time three-dimensional visualization in support of image guidance for ex vivo prostate specimen slicing parallel to the MR imaging planes prior to digitization, simplifying the registration process. The registration was performed interactively by using 3D Slicer (Surgical Planning Laboratory, Harvard Medical School, Boston, MA). Means, standard deviations, root-mean-square errors, and 95% confidence intervals are reported for all evaluated measurements. The slicing error was within the 2.2 mm thickness of the diagnostic-quality MR imaging sections, with a tissue block thickness standard deviation of 0.2 mm. Rigid registration provided negligible postregistration overlap of the smallest clinically important tumors (0.2 cm3) at histologic examination and MR imaging, whereas the tested nonrigid registration method yielded a mean target registration error of 1.1 mm and provided useful coregistration of such tumors. This method for the registration of prostate digital histopathologic images to in vivo MR images acquired by using an endorectal receive coil was sufficiently accurate for coregistering the smallest clinically important lesions with 95% confidence. |
 Image-guided specimen slicing process. The first step is to select a desired slicing plane orientation and location from the 3D in vivo image. By using image-based registration, this plane is transformed to the space of the ex vivo specimen image. Corresponding fiducial markers are localized on the ex vivo image (by using software) and on the physical specimen (by using a tracked stylus), and a landmark transform aligning these fiducial markers transforms the slicing plane into the space of the tracker. The tracked stylus is used to direct the insertion of three slicing plane–defining pins into the specimen, which align the specimen in a slotted forceps for slicing. This permits the establishment of a correspondence between stained histologic slices and in vivo imaging planes, which are registered by using a nonrigid registration. |
A Comparison of the Effect of Age on Levator Ani and Obturator Internus Muscle Cross-sectional Areas and Volumes in Nulliparous Women
|
Publication: Neurourol Urodyn. 2012 Apr;31(4):481-6. PMID: 22378544 | PDF Authors: Morris VC, Murray MP, Delancey JO, Ashton-Miller JA. Institution: University College London Hospital, London, UK. Background/Purpose: Functional tests have demonstrated minimal loss of vaginal closure force with age. So we tested the null hypotheses that age neither affects the maximum cross-sectional area (CSA) nor the volume of the levator muscle. Corresponding hypotheses were also tested in the adjacent obturator internus muscle, which served as a control for the effect of age on appendicular muscle in these women. Magnetic resonance images of 15 healthy younger (aged 21-25 years) and 12 healthy older nulliparous women (aged >63 years) were selected to avoid the confounding effect of childbirth. Models were created from tracing outlines of the levator ani muscle in the coronal plane, and obturator internus in the axial plane using 3D Slicer v.3.4. Muscle volumes were calculated using 3D Slicer, while CSA was measured using Imageware™ at nine locations. The hypotheses were tested using repeated measures analysis of variance with P < 0.05 being considered significant. The effect of age did not reach statistical significance for the decrease in levator ani muscle maximum CSA or the decrease in volume (4.3%, P = 0.62 and 10.9%, 0.12, respectively). However, age did significantly adversely decrease obturator internus muscle maximum CSA and volume (24.5% and 28.2%, P < 0.001, respectively). Significant local age-related changes were observed dorsally in both muscles. Unlike the adjacent appendicular muscle, obturator internus, the levator ani muscle in healthy nullipara does not show evidence of significant age-related atrophy. Funding:
|
|
Publication: IEEE Trans Med Imaging. 2012 Apr;31(4):963-76. PMID: 22113772 Authors: Mirota DJ, Wang H, Taylor RH, Ishii M, Gallia GL, Hager GD. Institution: Department of Computer Science, Johns Hopkins University, Baltimore, MD, USA. Background/Purpose: Surgeries of the skull base require accuracy to safely navigate the critical anatomy. This is particularly the case for endoscopic endonasal skull base surgery (ESBS) where the surgeons work within millimeters of neurovascular structures at the skull base. Today’s navigation systems provide approximately 2 mm accuracy. Accuracy is limited by the indirect relationship of the navigation system, the image and the patient. We propose a method to directly track the position of the endoscope using video data acquired from the endoscope camera. Our method first tracks image feature points in the video and reconstructs the image feature points to produce three-dimensional (3D) points, and then registers the reconstructed point cloud to a surface segmented from pre-operative computed tomography (CT) data. After the initial registration, the system tracks image features and maintains the two-dimensional (2D)-3D correspondence of image features and 3D locations. These data are then used to update the current camera pose. We present a method for validation of our system, which achieves sub-millimeter (0.70 mm mean) target registration error (TRE) results. Funding:
|
Levator Ani Subtended Volume: A Novel Parameter to Evaluate Levator Ani Muscle Laxity in Pelvic Organ Prolapse
|
Publication: Am J Obstet Gynecol. 2012 Mar;206(3):244.e1-9. PMID: 22075059 | PDF Authors: Rodrigues AA Jr, Bassaly R, McCullough M, Terwilliger HL, Hart S, Downes K, Hoyte L. Institution: Division of Female Pelvic Medicine and Reconstructive Surgery, Department of Obstetrics and Gynecology, University of South Florida College of Medicine, Tampa, FL. Background/Purpose: We describe a new parameter based on magnetic resonance 3-dimensional (3D) reconstructions proposed to evaluate levator ani muscle (LAM) laxity in women with pelvic organ prolapse (POP). This is an institutional review board-approved, retrospective chart review of 35 women with POP, stages I-IV. The 3D Slicer software package was used to perform 2-dimensional and 3D measurements and the levator ani subtended volume (LASV) was described. Basically, the LASV represents the volume contained by LAM between 2 planes, which coincides with pubococcygeal line and H line. Correlations among measurements, ordinal POP stages, POP Quantification (POPQ) individual measurements, and validated questionnaires were performed. The LASV differentiated major (III and IV) from minor (I and II) POPQ stages, which positively correlated to POP stages and POPQ individual measurements. The LASV is a promising parameter to evaluate the LAM laxity. |
 Two sequences showing segmentation processA, Midsagittal views of pelvic floor; representations of pubococcygeal line (PCL), H line, and M line (white); and anterior (yellow) and posterior (green) limits of levator hiatus volume. B, Levator ani muscle (LAM) and levator hiatus segmentation following caudal-cranial orientation. Levator hiatus was segmented based on previous limits obtained from midsagittal slice and inner boundaries of LAM, obturator internus muscle, and pubic bone.Rodrigues. A new parameter proposed to evaluate the levator ani laxity. |
Tractography Delineates Microstructural Changes in the Trigeminal Nerve After Focal Radiosurgery for Trigeminal Neuralgia
|
Publication: PLoS One. 2012 Mar;7(3):e32745. PMID:22412918 | PDF Authors: Hodaie M, Chen DQ, Quan J, Laperriere N. Institution: Division of Neurosurgery, Toronto Western Hospital and University of Toronto, Toronto, ON, Canada. Background/Purpose: Focal radiosurgery is a common treatment modality for trigeminal neuralgia (TN), a neuropathic facial pain condition. Assessment of treatment effectiveness is primarily clinical, given the paucity of investigational tools to assess trigeminal nerve changes. Since diffusion tensor imaging (DTI) provides information on white matter microstructure, we explored the feasibility of trigeminal nerve tractography and assessment of DTI parameters to study microstructural changes after treatment. We hypothesized that trigeminal tractography provides more information than 2D-MR imaging, allowing detection of unique, focal changes in the target area after radiosurgery. Changes in specific diffusivities may provide insight into the mechanism of action of radiosurgery on the trigeminal nerve. Funding: |
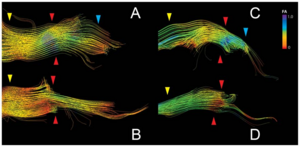 Tractography outlines detailed FA changes in the trigeminal nerve after GKRS treatment. Panels A-D depict the trigeminal nerve tracts pre and post-treatment for subjects S1(A,B) and S2 (C,D). The area between the yellow and blue arrows delineates the cisternal segment, with the yellow arrow being proximal to the brainstem and the blue arrow distal. The red arrow denotes the target area, which corresponds to the region where the greatest change in FA was observed. In S1, FA change affects primarily the outlying fibers of the nerve, while for S2, FA changes are seen in the inferior portion of the cisternal segment of the trigeminal nerve. Tractography were performed using the 3D Slicer software. |
Square-cut: A Segmentation Algorithm on the Basis of a Rectangle Shape
|
Publication: PLoS One. 2012 Feb;7(2):e31064. PMID: 22363547 | PDF Authors: Egger J, Kapur T, Dukatz T, Kolodziej M, Zukić D, Freisleben B, Nimsky C. Institution: Surgical Planning Laboratory, Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: We present a rectangle-based segmentation algorithm that sets up a graph and performs a graph cut to separate an object from the background. However, graph-based algorithms distribute the graph's nodes uniformly and equidistantly on the image. Then, a smoothness term is added to force the cut to prefer a particular shape. This strategy does not allow the cut to prefer a certain structure, especially when areas of the object are indistinguishable from the background. We solve this problem by referring to a rectangle shape of the object when sampling the graph nodes, i.e., the nodes are distributed non-uniformly and non-equidistantly on the image. This strategy can be useful, when areas of the object are indistinguishable from the background. For evaluation, we focus on vertebrae images from Magnetic Resonance Imaging (MRI) datasets to support the time consuming manual slice-by-slice segmentation performed by physicians. The ground truth of the vertebrae boundaries were manually extracted by two clinical experts (neurological surgeons) with several years of experience in spine surgery and afterwards compared with the automatic segmentation results of the proposed scheme yielding an average Dice Similarity Coefficient (DSC) of 90.97±2.2%. Funding:
|
Anatomical and Functional Correlates of Human Hippocampal Volume Asymmetry
|
Publication: Psychiatry Res. 2012 Jan; 201(1): 48-53. PMID: 22285719 | PDF Authors: Woolard AA, Heckers S. Institution: Department of Osychiatry, Vaderbilt University, Nashville, TN, USA. Background/Purpose: Hemispheric asymmetry of the human hippocampus is well established, but poorly understood. We studied 110 healthy subjects with 3-Tesla MRI to explore the anatomical and functional correlates of the R>L volume asymmetry. We found that the asymmetry is limited to the anterior hippocampus (hemisphere×region interaction: F(1,109)=42.6, p<.001). Anterior hippocampal volume was correlated strongly with the volumes of all four cortical lobes. In contrast, posterior hippocampal volume was correlated strongly only with occipital lobe volume, moderately with the parietal and temporal lobe volumes and not with the frontal lobe volume. The degree of R>L anterior hippocampal volume asymmetry predicted performance on a measure of basic cognitive abilities. This provides evidence for regional specificity and functional implications of the well-known hemispheric asymmetry of hippocampal volume. We suggest that the developmental profile, genetic mechanisms and functional implications of R>L anterior hippocampal volume asymmetry in the human brain deserve further study. Funding:
|
Hippocampal Subregions are Differentially Affected in the Progression to Alzheimer's Disease
|
Publication: Anat Rec (Hoboken). 2012 Jan;295(1):132-40. PMID: 22095921 | PDF Authors: Greene SJ, Killiany RJ; Alzheimer's Disease Neuroimaging Initiative Institution: Department of Anatomy and Neurobiology, University of Vermont College of Medicine, Burlington, VT, USA. Background/Purpose: Atrophy within the hippocampus (HP) as measured by magnetic resonance imaging (MRI) is a promising biomarker for the progression to Alzheimer's disease (AD). Subregions of the HP along the longitudinal axis have been found to demonstrate unique function, as well as undergo differential changes in the progression to AD. Little is known of relationships between such HP subregions and other potential biomarkers, such as neuropsychological (NP), genetic, and cerebral spinal fluid (CSF) beta amyloid and tau measures. The purpose of this study was to subdivide the hippocampus to determine how the head, body, and tail were affected in normal control, mild cognitively impaired, and AD subjects, and investigate relationships with HP subregions and other potential biomarkers. MRI scans of 120 participants of the Alzheimer's Disease Neuroimaging Initiative were processed using FreeSurfer, and the HP was subdivided using 3D Slicer. Each subregion was compared among groups, and correlations were used to determine relationships with NP, genetic, and CSF measures. Results suggest that HP subregions are undergoing differential atrophy in AD, and demonstrate unique relationships with NP and CSF data. Discriminant function analyses revealed that these regions, when combined with NP and CSF measures, were able to classify by diagnostic group, and classify MCI subjects who would and would not progress to AD within 12 months. Funding:
|
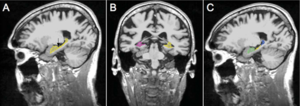 Methods for identifying boundaries for the head, body, and tail of the hippocampus. A: Arrow is pointing to the head/body boundary. B: View of body/tail boundary in left hemisphere where the fimbria of the fornix comes into view; body/tail boundary. C: Subregions after relabeling has been completed (green: head; yellow: body; blue: tail). |
Long-term Memory Search Across the Visual Brain
|
Publication: Neural Plast. 2012;2012:392695. PMID: 22900206 | PDF Authors: Fedurco M. Institution: Michelin Recherche Technique, Fribourg, Switzerland. Background/Purpose: Signal transmission from the human retina to visual cortex and connectivity of visual brain areas are relatively well understood. How specific visual perceptions transform into corresponding long-term memories remains unknown. Here, I will review recent Blood Oxygenation Level-Dependent functional Magnetic Resonance Imaging (BOLD fMRI) in humans together with molecular biology studies (animal models) aiming to understand how the retinal image gets transformed into so-called visual (retinotropic) maps. The broken object paradigm has been chosen in order to illustrate the complexity of multisensory perception of simple objects subject to visual - rather than semantic - type of memory encoding. The author explores how amygdala projections to the visual cortex affect the memory formation and proposes the choice of experimental techniques needed to explain our massive visual memory capacity. Maintenance of the visual long-term memories is suggested to require recycling of GluR2-containing α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors (AMPAR) and β(2)-adrenoreceptors at the postsynaptic membrane, which critically depends on the catalytic activity of the N-ethylmaleimide-sensitive factor (NSF) and protein kinase PKMζ. |
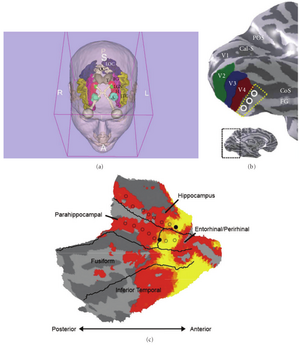 Parcellation of the human visual cortex and brain areas involved in visual object perception: (a) eye bulb—grey, optical tract/optical chiasm—white, lateral geniculate nucleus (LGN)—green, occipital visual cortex (OC)—white, lateral occipital gyrus (LOC)—navy blue, inferior temporal gyrus (ITC)—creamy yellow, fusiform gyrus (FG)—magenta, hippocampus (H)—red, amygdala (A)—cyan, thalamus (T)—grey (created using the 3D Slicer). (b) Ventral occipital visual field map models: Cal-S (V1)—calcarine sulcus, V2—green, V3—blue, V4 (brick red), FG—fusiform gyrus, CoS—collateral sulcus, POS—parietal occipital sulcus. The dotted yellow line and white circles denote the region of cortex in which the V4 and V8 models diverge (inset shows inflated model of the left human hemisphere). (c) Anterior part of the fusiform gyrus is located in the vicinity of the hippocampal formation. (b) reproduced, with permission, from [25] Macmillan Publishers Ltd. (c) (right) reproduced, with permission, from [39] the American Physiological Society. |
Temporal Course of Cerebrospinal Fluid Dynamics and Amyloid Accumulation in the Aging Rat Brain from Three to Thirty Months
|
Publication: Fluids Barriers CNS. 2012 Jan 23;9(1):3. PMID: 22269091 | PDF Authors: Chiu C, Miller MC, Caralopoulos IN, Worden MS, Brinker T, Gordon ZN, Johanson CE, Silverberg GD. Institution: Department of Neurosurgery, Warren Alpert Medical School, Brown University and Aldrich Neurosurgery Research Laboratories, Rhode Island Hospital, Providence, RI, USA. Background/Purpose: Amyloid accumulation in the brain parenchyma is a hallmark of Alzheimer's disease (AD) and is seen in normal aging. Alterations in cerebrospinal fluid (CSF) dynamics are also associated with normal aging and AD. This study analyzed CSF volume, production and turnover rate in relation to amyloid-beta peptide (Aβ) accumulation in the aging rat brain. Aging Fischer 344/Brown-Norway hybrid rats at 3, 12, 20, and 30 months were studied. CSF production was measured by ventriculo-cisternal perfusion with blue dextran in artificial CSF; CSF volume by MRI; and CSF turnover rate by dividing the CSF production rate by the volume of the CSF space. Aβ40 and Aβ42 concentrations in the cortex and hippocampus were measured by ELISA. There was a significant linear increase in total cranial CSF volume with age: 3-20 months (p < 0.01); 3-30 months (p < 0.001). CSF production rate increased from 3-12 months (p < 0.01) and decreased from 12-30 months (p < 0.05). CSF turnover showed an initial increase from 3 months (9.40 day-1) to 12 months (11.30 day-1) and then a decrease to 20 months (10.23 day-1) and 30 months (6.62 day-1). Aβ40 and Aβ42 concentrations in brain increased from 3-30 months (p < 0.001). Both Aβ42 and Aβ40 concentrations approached a steady state level by 30 months. In young rats there is no correlation between CSF turnover and Aβ brain concentrations. After 12 months, CSF turnover decreases as brain Aβ continues to accumulate. This decrease in CSF turnover rate may be one of several clearance pathway alterations that influence age-related accumulation of brain amyloid. Funding:
|
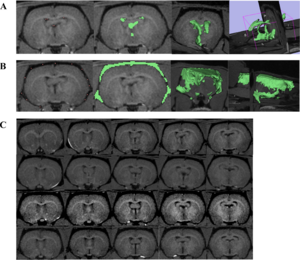 Total CSF volume. A) CSF in the ventricles was measured by placing fiducial points (pink dots) on black pixels within the region of interest. FastMarching Segmentation in 3D Slicer generates a rough sketch of the region of interest (green areas), as well as a 3D model. Volume is calculated from this model. B) Similar steps were taken to measure CSF in the subarachnoid space. All measurements were done by one reader for consistency. C) T1-weighted MR images. Each row represents five coronal slices from one rat brain (top row = 3 month, second row = 12 month, third row = 20 month, bottom row = 30 month). Images were magnified and brightened for printing purposes. |
Intact Relational Memory and Normal Hippocampal Structure in the Early Stage of Psychosis
|
Publication: Biol Psychiatry. 2012 Jan 15;71(2):105-13. PMID: 22055016 | PDF Authors: Williams LE, Avery SN, Woolard AA, Heckers S. Institution: Department of Psychiatry, Vanderbilt University, Nashville, TN, USA. Background/Purpose: Previous studies indicate that the transition to psychosis is associated with dynamic changes of hippocampal integrity. Here we explored hippocampal volume and neural activation during a relational memory task in patients who were in the early stage of a psychotic illness. Forty-one early psychosis patients and 34 healthy control subjects completed a transitive inference (TI) task used previously in chronic schizophrenia patients. Participants learned to select the "winner" of two sets of stimulus pairs drawn from an overlapping sequence (A > B > C > D > E) and a non-overlapping set (a > b, c > d, e > f, g > h). During a functional magnetic resonance imaging scan, participants were tested on the trained pairs and made inferential judgments on novel pairings that could be solved based on training (e.g., B vs. D). Hippocampal volumes were manually segmented and compared between groups. Functional magnetic resonance imaging analyses included 27 early psychosis patients and 30 control subjects who met memory training criteria. Groups did not differ on inference performance or hippocampal volume and exhibited similar activation of medial temporal regions when judging nonoverlapping pairs. However, patients who failed to meet memory training criteria had smaller hippocampal volumes. Neural activity during TI was less widespread in early psychosis patients, but between-group differences were not significant. Hippocampal activity during TI was positively correlated with inference performance only in control subjects. Our results provide evidence that relational memory impairment and hippocampal abnormalities, well established in chronic schizophrenia, are not fully present in early psychosis patients. This provides a rationale for early intervention, targeting the possible delay, reduction, or prevention of these deficits. Funding:
|
 Significant clusters of activation during transitive inference, p < .05 corrected cluster threshold: bilateral medial and superior frontal gyri (A control), bilateral cingulate (B, C, D controls, C early psychosis), middle temporal gyrus (left B, C, D control, bilateral D, E early psychosis), left superior temporal gyrus (B control), left paracentral lobule (B control), bilateral angular gyrus (D control), bilateral precuneus (D early psychosis), bilateral middle/inferior occipital gyrus (E control), and bilateral cerebellum (D, E). A direct comparison between groups revealed no significant differences. |
TREK: An Integrated System Architecture for Intraoperative Cone-beam CT-guided Surgery
|
Publication: Int J Comput Assist Radiol Surg. 2012 Jan;7(1):159-73. PMID: 21744085 Authors: Uneri A, Schafer S, Mirota DJ, Nithiananthan S, Otake Y, Taylor RH, Siewerdsen JH. Institution: Department of Computer Science, Johns Hopkins University, Baltimore, MD, USA. Background/Purpose: A system architecture has been developed for integration of intraoperative 3D imaging [viz., mobile C-arm cone-beam CT (CBCT)] with surgical navigation (e.g., trackers, endoscopy, and preoperative image and planning data). The goal of this paper is to describe the architecture and its handling of a broad variety of data sources in modular tool development for streamlined use of CBCT guidance in application-specific surgical scenarios. Methods: The architecture builds on two proven open-source software packages, namely the cisst package (Johns Hopkins University, Baltimore, MD) and 3D Slicer (Brigham and Women's Hospital, Boston, MA), and combines data sources common to image-guided procedures with intraoperative 3D imaging. Integration at the software component level is achieved through language bindings to a scripting language (Python) and an object-oriented approach to abstract and simplify the use of devices with varying characteristics. The platform aims to minimize offline data processing and to expose quantitative tools that analyze and communicate factors of geometric precision online. Modular tools are defined to accomplish specific surgical tasks, demonstrated in three clinical scenarios (temporal bone, skull base, and spine surgery) that involve a progressively increased level of complexity in toolset requirements. The resulting architecture (referred to as "TREK") hosts a collection of modules developed according to application-specific surgical tasks, emphasizing streamlined integration with intraoperative CBCT. These include multi-modality image display; 3D-3D rigid and deformable registration to bring preoperative image and planning data to the most up-to-date CBCT; 3D-2D registration of planning and image data to real-time fluoroscopy; infrared, electromagnetic, and video-based trackers used individually or in hybrid arrangements; augmented overlay of image and planning data in endoscopic or in-room video; and real-time "virtual fluoroscopy" computed from GPU-accelerated digitally reconstructed radiographs (DRRs). Application in three preclinical scenarios (temporal bone, skull base, and spine surgery) demonstrates the utility of the modular, task-specific approach in progressively complex tasks. The design and development of a system architecture for image-guided surgery has been reported, demonstrating enhanced utilization of intraoperative CBCT in surgical applications with vastly different requirements. The system integrates C-arm CBCT with a broad variety of data sources in a modular fashion that streamlines the interface to application-specific tools, accommodates distinct workflow scenarios, and accelerates testing and translation of novel toolsets to clinical use. The modular architecture was shown to adapt to and satisfy the requirements of distinct surgical scenarios from a common code-base, leveraging software components arising from over a decade of effort within the imaging and computer-assisted interventions community. Funding:
|
Cholesterol Increases Ventricular Volume in a Rabbit Model of Alzheimer's Disease
|
Publication: J Alzheimers Dis. 2012;29(2):283-92. PMID: 22232012 | PDF Authors: Deci S, Lemieux SK, Smith-Bell CA, Sparks DL, Schreurs BG. Institution: Department of Physiology and Pharmacology and the Blanchette Rockefeller Neurosciences Institute, West Virginia University, Morgantown, WV, USA. Background/Purpose: One of the hallmarks of Alzheimer's disease is a significant increase in ventricular volume. To date we and others have shown that a cholesterol-fed rabbit model of Alzheimer's disease displays as many as fourteen different pathological markers of Alzheimer's disease including amyloid-β accumulation, thioflavin-S staining, blood brain barrier breach, microglia activation, cerebrovasculature changes, and alterations in learning and memory. Using structural magnetic resonance imaging at 3T, we now report that cholesterol-fed rabbits also show a significant increase in ventricular volume following 10 weeks on a diet of 2% cholesterol. The increase in volume is attributable in large part to increases in the size of the third ventricle. These changes are accompanied by significant increases in the number of amyloid-β immuno-positive cells in the cortex and hippocampus. Increases in the number of amyloid-β neurons in the cortex also occurred with the addition of 0.24 ppm copper to the drinking water. Together with a list of other pathological markers, the current results add further validity to the value of the cholesterol-fed rabbit as a non-transgenic animal model of Alzheimer's disease. Funding:
|
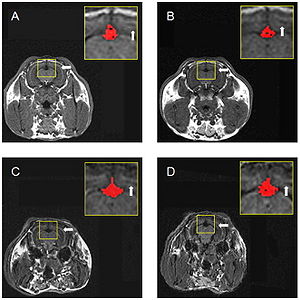 Panels show analysis of ventricular volume in a sample MRI axial scan for a rabbit that received chow and distilled water (A), chow and 0.24 ppm copper in distilled water (B), chow plus 2% cholesterol and distilled water (C), or chow with 2% cholesterol and 0.24 ppm copper in distilled water (D). The inset of each panel shows the third ventricle selected using the intensity-based threshold painting method. The white arrows indicate the barely detectable lateral ventricle. |
2011
Atlas-guided Segmentation of Vervet Monkey Brain MRI
|
Publication: Open Neuroimag J. 2011 Dec;5:186-97. PMID: 22253661 | PDF Authors: Fedorov A, Li X, Pohl KM, Bouix S, Styner M, Addicott M, Wyatt C, Daunais JB, Wells WM, Kikinis R. Institution: Surgical Planning Laboratory, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: User interaction is required for reliable segmentation of brain tumors in clinical practice and in clinical research. By incorporating current research tools, 3D Slicer provides a set of interactive, easy to use tools that can be efficiently used for this purpose. One of the modules of 3D Slicer is an interactive editor tool, which contains a variety of interactive segmentation effects. Use of these effects for fast and reproducible segmentation of a single glioblastoma from magnetic resonance imaging data is demonstrated. The innovation in this work lies not in the algorithm, but in the accessibility of the algorithm because of its integration into a software platform that is practical for research in a clinical setting. Funding:
|
Comparison of Acute and Chronic Traumatic Brain Injury Using Semi-automatic Multimodal Segmentation of MR Volumes
|
Publication: J Neurotrauma. 2011 Nov;28(11):2287-306. PMID: 21787171 | PDF Authors: Irimia A, Chambers MC, Alger JR, Filippou M, Prastawa MW, Wang B, Hovda DA, Gerig G, Toga AW, Kikinis R, Vespa PM, Van Horn JD. Institution: Laboratory of Neuro Imaging, University of California, Los Angeles, CA, USA. Background/Purpose: Though neuroimaging is essential for prompt and proper management of TBI, there is regrettable and acute lack of robust methods for the visualization and assessment of TBI pathophysiology, especially for of the purpose of improving clinical outcome metrics. Until now, the application of automatic segmentation algorithms to TBI in a clinical setting has remained an elusive goal because existing methods have, for the most part, been insufficiently robust to faithfully capture TBI-related changes in brain anatomy. This article introduces and illustrates the combined use of multimodal TBI segmentation and time point comparison using 3D Slicer, a widely-used software environment whose TBI data processing solutions are openly available. For three representative TBI cases, semi-automatic tissue classification and 3D model generation are performed to perform intra-patient time point comparison of TBI using multimodal volumetrics and clinical atrophy measures. Identification and quantitative assessment of extra- and intra-cortical bleeding, lesions, edema and diffuse axonal injury are demonstrated. The proposed tools allow cross-correlation of multimodal metrics from structural imaging (structural volume, atrophy measurements, etc.) with clinical outcome variables and other potential factors predictive of recovery. In addition, the workflows described are suitable for TBI clinical practice and patient monitoring, particularly for assessing damage extent and for the measurement of neuroanatomical change over time. With knowledge of general location, extent, and degree of change, such metrics can be associated with clinical measures and subsequently used to suggest viable treatment options. Funding:
|
 Three-dimensional models of TBI anatomy for Patient 1 (acute baseline time point), as generated in 3D Slicer. Each row displays one of six canonical views of the brain, whereas each column corresponds to a structure type (ventricles, non-hemorrhagic lesions, hemorrhagic lesions, and full model). In (A), ventricles are shown as opaque, whereas extracerebral injuries, gray matter (GM) and white matter (WM) volumes are shown as transparent to facilitate visualization of each structure in relationship to cortical landmarks. In (B–D), ventricles are also shown as transparent for similar reasons. Arrows indicate TBI-related pathology of interest (see text for elaboration). |
3D Slicer
|
Publication: PDF Video. 2011 November 18. Authors: Muschelli J, Zipunnikov V. Institution: Department of Biostatistics, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA. Background/Purpose: Quick tutorial of how to make 3D models in 3D Slicer. |
An Open Environment CT-US Fusion for Tissue Segmentation During Interventional Guidance
|
Publication: PLoS One. 2011 Novemeber;6(11):e27372. PMID: 22132098 | PDF Authors: Caskey CF, Hlawitschka M, Qin S, Mahakian LM, Cardiff RD, Boone JM, Ferrara KW. Institution: Department of Biomedical Engineering, University of California Davis, Davis, CA, USA. Background/Purpose: Therapeutic ultrasound (US) can be noninvasively focused to activate drugs, ablate tumors and deliver drugs beyond the blood brain barrier. However, well-controlled guidance of US therapy requires fusion with a navigational modality, such as magnetic resonance imaging (MRI) or X-ray computed tomography (CT). Here, we developed and validated tissue characterization using a fusion between US and CT. The performance of the CT/US fusion was quantified by the calibration error, target registration error and fiducial registration error. Met-1 tumors in the fat pads of 12 female FVB mice provided a model of developing breast cancer with which to evaluate CT-based tissue segmentation. Hounsfield units (HU) within the tumor and surrounding fat pad were quantified, validated with histology and segmented for parametric analysis (fat: −300 to 0 HU, protein-rich: 1 to 300 HU, and bone: HU>300). Our open source CT/US fusion system differentiated soft tissue, bone and fat with a spatial accuracy of ~1 mm. Region of interest (ROI) analysis of the tumor and surrounding fat pad using a 1 mm2 ROI resulted in mean HU of 68±44 within the tumor and −97±52 within the fat pad adjacent to the tumor (p<0.005). The tumor area measured by CT and histology was correlated (r2 = 0.92), while the area designated as fat decreased with increasing tumor size (r2 = 0.51). Analysis of CT and histology images of the tumor and surrounding fat pad revealed an average percentage of fat of 65.3% vs. 75.2%, 36.5% vs. 48.4%, and 31.6% vs. 38.5% for tumors <75 mm3, 75-150 mm3 and >150 mm3, respectively. Further, CT mapped bone-soft tissue interfaces near the acoustic beam during real-time imaging. Combined CT/US is a feasible method for guiding interventions by tracking the acoustic focus within a pre-acquired CT image volume and characterizing tissues proximal to and surrounding the acoustic focus. Funding:
|
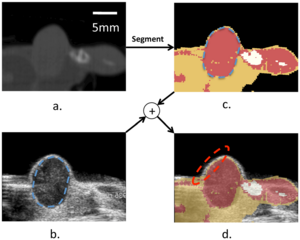 Combined CT/US characterizes tissue. (a) CT slice of a hindlimb tumor corresponding to the US slice in (b). The segmented CT slice is shown in (c) and overlaid on the US image in (d). The combined segmented CT/US image identifies fat proximal to and surrounding the tumor during ultrasonic imaging, with registration accuracy on the order of 1 mm. Nearby bone is obvious in the CT image (c) but not immediately visualized by US (b). |
|
Publication: Brain Behav. 2011 November; 1(2): 125-34. PMID: 22399092 | PDF Authors: Cherbuin N, Sachdev PS, Anstey KJ. Institution: Centre for Mental Health Research, Australian National University, Canberra, Australia. Background/Purpose: Handedness has been found to be associated with structural and functional cerebral differences. Left handedness and mixed handedness also appear to be associated with an elevated risk of some developmental and immunological disorders that may contribute to pathological processes developing in aging. Inconsistent reports show that left handedness may be more prevalent in early-onset as well as late-onset Alzheimer's disease, but might also be associated with slower decline. Such inconsistencies may be due to handedness being usually modeled as a binary construct while substantial evidence suggests it to be a continuous trait. The aim of this study was to investigate the relationship between brain structures known to be implicated in pathological ageing and strength and direction of handedness. The association between handedness and hippocampal and amygdalar atrophy was investigated in 327 cognitively healthy older individuals. Handedness was measured with the Edinburgh Inventory. Two measures were computed from this index, one reflecting the direction (left = 0/right = 1) and the other the degree of handedness (ranging from 0 to 1). Hippocampal and amygdalar volumes were manually traced on scans acquired 4 years apart. Regression analyses were used to assess the relationship between strength and direction of handedness and incident hippocampal and amygdalar atrophy. Analyses showed that strength but not direction of handedness was a significant predictor of hippocampal (Left: beta = 0.118, P = 0.013; Right: beta = 0.116, P = 0.010) and amygdalar (Right: beta = 0.105, P = 0.040) atrophy. The present findings suggest that mixed but not left handedness is associated with greater hippocampal and amygdalar atrophy. This effect may be due to genetic, environmental, or behavioral differences that will need further investigation in future studies. Funding:
|
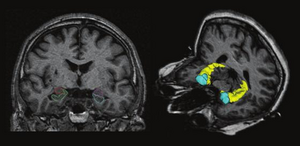 Left: Manual tracings from the analyze package of the left and right hippocampi (green and blue) and of the left and right amygdala (red and purple). Right: 3D model of the hippocampus (yellow) and of the amygdala (blue) rendered in 3D Slicer. |
Multiple Costal Cartilage Graft Reconstruction for the Treatment of a Full-length Laryngotracheal Stenosis after an Inhalation Burn
|
Publication: Interact Cardiovasc Thorac Surg. 2011 Oct;13(4):453-5. PMID: 21798888 | PDF Authors: Furák J, Szakács L, Nagy A, Rovó L. Institution: Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University of Szeged, Szeged, Hungary. Background/Purpose: After suffering an inhalation burn, a 22-year-old male was intubated for seven days. Full-length massive scar formation in the upper airway necessitated tracheostomy five months later. After this, the stenosis became complete in the cricoid region, and a long cannula was needed to maintain the severely damaged middle-distal trachea. After unsuccessful laser dilatation, the more stenotic 3 cm distal tracheal segment was resected, but two months later the stenosis recurred. As resection was ineffective, tracheoplasty was performed via a right-sided thoracotomy; the re-stenotized trachea was incised in length and successfully extended with 5 cm long, oval-shaped rib cartilage. Three months later, the complete cricotracheal stenosis was fixed by combined laryngofissure and cricoid laminotomy with two 6 cm×2.5 cm cartilage pieces sutured into the incisions. The middle portion of the trachea was expanded with a similar graft inserted into the anterior wall below the tracheostomy. The fixing T-tube was removed three months later, and the patient had an adequate airway two years after the last procedure. We conclude that multiple cartilage graft reconstruction can be successful even after the development of an extremely long airway stenosis following inhalation burn injury. |
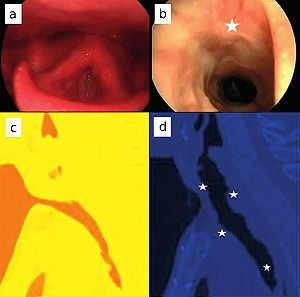 Pre- and postoperative (two years after tracheoplasty) images. (a, b) Endoscopic pictures. (c, d) Median sagittal computed tomography reconstruction (3D Slicer software, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA). Stars show the site of the grafts. |
A Supervised Patch-based Approach for Human Brain Labeling
|
Publication: IEEE Trans Med Imaging. 2011 Oct;30(10):1852-62. PMID: 21606021 | PDF Authors: Rousseau F, Habas PA, Studholme C. Institution: Laboratoire des Sciences de l’Image, de l’Informatique et de la Télédétection (LSIIT), University of Strasbourg, Illkirch, France. Background/Purpose: We propose in this work a patch-based image labeling method relying on a label propagation framework. Based on image intensity similarities between the input image and an anatomy textbook, an original strategy which does not require any nonrigid registration is presented. Following recent developments in nonlocal image denoising, the similarity between images is represented by a weighted graph computed from an intensity-based distance between patches. Experiments on simulated and in vivo magnetic resonance images show that the proposed method is very successful in providing automated human brain labeling. Funding:
|
The Chronic Bronchitic Phenotype of COPD: An Analysis of the COPDGene Study
|
Publication: Chest. 2011 Sep;140(3):626-33. PMID: 21474571 | PDF Authors: Kim V, Han MK, Vance GB, Make BJ, Newell JD, Hokanson JE, Hersh CP, Stinson D, Silverman EK, Criner GJ; COPDGene Investigators. Institution: Temple University School of Medicine, Philadelphia, PA, USA. Background/Purpose: Chronic bronchitis (CB) in patients with COPD is associated with an accelerated lung function decline and an increased risk of respiratory infections. Despite its clinical significance, the chronic bronchitic phenotype in COPD remains poorly defined. We analyzed data from subjects enrolled in the Genetic Epidemiology of COPD (COPDGene) Study. A total of 1,061 subjects with GOLD (Global Initiative for Chronic Obstructive Lung Disease) stage II to IV were divided into two groups: CB (CB+) if subjects noted chronic cough and phlegm production for ≥ 3 mo/y for 2 consecutive years, and no CB (CB-) if they did not. There were 290 and 771 subjects in the CB+ and CB- groups, respectively. Despite similar lung function, the CB+ group was younger (62.8 ± 8.4 vs 64.6 ± 8.4 years, P = .002), smoked more (57 ± 30 vs 52 ± 25 pack-years, P = .006), and had more current smokers (48% vs 27%, P < .0001). A greater percentage of the CB+ group reported nasal and ocular symptoms, wheezing, and nocturnal awakenings secondary to cough and dyspnea. History of exacerbations was higher in the CB+ group (1.21 ± 1.62 vs 0.63 ± 1.12 per patient, P < .027), and more patients in the CB+ group reported a history of severe exacerbations (26.6% vs 20.0%, P = .024). There was no difference in percent emphysema or percent gas trapping, but the CB+ group had a higher mean percent segmental airway wall area (63.2% ± 2.9% vs 62.6% ± 3.1%, P = .013). CB in patients with COPD is associated with worse respiratory symptoms and higher risk of exacerbations. This group may need more directed therapy targeting chronic mucus production and smoking cessation not only to improve symptoms but also to reduce risk, improve quality of life, and improve outcomes. Funding:
|
Airway Inspector: Phenotyping the Lung in COPD
|
Publication: Airway Inspector Contact Person: Raul San Jose Estepar Institution: Surgical Planning Laboratory, Brigham and Women's Hospital, Harvard Medical School, Boston, MA. Background/Purpose: Airway Inspector is a free open source tool for CT-based image quantitative analysis of the lung. It provides the tools that clinical scientist can used to explore airway morphology and desitometric characteristics. Airway Inspector is the gateway to phenotype airway diseases. Airway Inspector is maintained by the Applied Chest Imaging Laboratory (ACIL) and is based on the 3D Slicer. The 3D Slicer is a general purpose open source platform for medical image analysis maintained by the Surgical Planning Laboratory at Brigham and Women's Hospital, Boston, MA. Funding:
|
Distance Measurement in Middle Ear Surgery using a Telemanipulator
|
Publication: Med Image Comput Comput Assist Interv. 2011;14(Pt 1):41-8. PMID: 22003598 | PDF Authors: Maier T, Strauss G, Bauer F, Grasser A, Hata N, Lueth TC. Institution: Institute of Microtechnology and Medical Device Technology (MiMed), Technische Universität München, Munich, Germany. Background/Purpose: In this article, a new tool for the intraoperative measurement of distances within the middle ear by means of a micromanipulator is presented. The purpose of this work was to offer the surgeon a highly accurate tool for measuring the distances between two points in the 3D operational field. The tool can be useful in various operations; this article focuses, however, on measuring the distance between the stapes footplate and the long process of the incus of the middle ear. This distance is important for estimating the proper prosthesis length in stapedotomy for treating otosclerosis. We evaluated the system using a simplified mechanical model. Our results show that the system can measure distances with a maximum error of 0.04 mm. Funding:
|
3D Slicer as a Tool for Interactive Brain Tumor Segmentation
|
Publication: Conf Proc IEEE Eng Med Biol Soc. 2011 Aug;2011:6982-4. PMID: 22255945 | PDF Authors: Kikinis R, Pieper S. Institution: Surgical Planning Laboratory, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: User interaction is required for reliable segmentation of brain tumors in clinical practice and in clinical research. By incorporating current research tools, 3D Slicer provides a set of interactive, easy to use tools that can be efficiently used for this purpose. One of the modules of 3D Slicer is an interactive editor tool, which contains a variety of interactive segmentation effects. Use of these effects for fast and reproducible segmentation of a single glioblastoma from magnetic resonance imaging data is demonstrated. The innovation in this work lies not in the algorithm, but in the accessibility of the algorithm because of its integration into a software platform that is practical for research in a clinical setting. Funding:
|
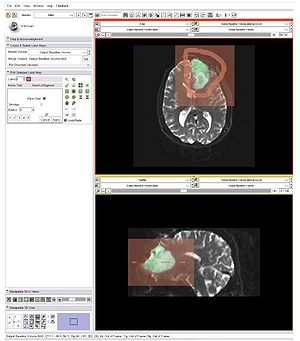 Partial screenshot of 3D Slicer, demonstrating the use of the “GrowCut” effect for segmentation of the solid and cystic components of a brain tumor. Axial and sagittal cross-sections are displayed. The algorithm was initialized on a single slice, but segmented the entire tumor. Initialization is seen in solid colors; segmentation results are displayed as a semi-transparent overlay on the T2 weighted image. Note that two shades of green were used for the solid and cystic components. |
The Effect of Augmented Reality Training on Percutaneous Needle Placement in Spinal Facet Joint Injections
|
Publication: IEEE Trans Biomed Eng. 2011 Jul;58(7):2031-7. PMID: 21435970 | PDF Authors: Yeo CT, Ungi T, U-Thainual P, Lasso A, McGraw RC, Fichtinger G. Institution: School of Medicine, Queen’s University, Kingston, ON, Canada. Background/Purpose: The purpose of this study was to determine if augmented reality image overlay and laser guidance systems can assist learn how to perform the procedure without the risk of errors medical trainees in learning the correct placement of a needle for causing harm to the patient [2]. Additionally, simulation allows percutaneous facet joint injection. The Perk Station training suite was used to conduct and record the needle insertion procedures. A total of 40 volunteers were randomized into two groups of 20. 1) The Overlay group received a training session that consisted of four insertions with image and laser guidance, followed by two insertions with laser overlay only. 2) The Control group received a training session of six classical freehand insertions. Both groups then conducted two freehand insertions. The movement of the needle was tracked during the series of insertions. The final insertion procedure was assessed to determine if there was a benefit to the overlay method compared to the freehand insertions. The Overlay group had a better success rate (83.3% versus 68.4%, p = 0.002), and potential for less tissue damage as measured by the amount of needle movement inside the phantom (3077.6 mm2 versus 5607.9 mm2, p = 0.01). These results suggest that an augmented reality overlay guidance system can assist medical trainees in acquiring technical competence in a percutaneous needle insertion procedure. Funding:
|
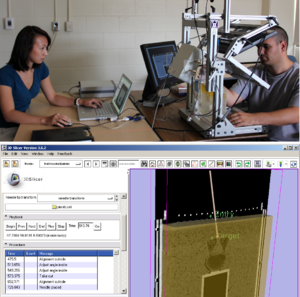 Image overlay simulator for the training of facet joint injections (upper image). 3D Slicer module for offline evaluation of the trainee performance from tracked needle trajectories (lower image). |
Optimal Transseptal Puncture Location for Robot-assisted Left Atrial Catheter Ablation
|
Publication: Int J Med Robot. 2011 Jun;7(2):193-201. PMID: 21538767 | PDF Authors: Jayender J, Patel RV, Michaud GF, Hata N. Institution: Surgical Planning Laboratory, Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: The preferred method of treatment for atrial fibrillation (AF) is by catheter ablation, in which a catheter is guided into the left atrium through a transseptal puncture. However, the transseptal puncture constrains the catheter, thereby limiting its manoeuvrability and increasing the difficulty in reaching various locations in the left atrium. In this paper, we address the problem of choosing the optimal transseptal puncture location for performing cardiac ablation to obtain maximum manoeuvrability of the catheter. We have employed an optimization algorithm to maximize the global isotropy index (GII) to evaluate the optimal transseptal puncture location. As part of this algorithm, a novel kinematic model for the catheter has been developed, based on a continuum robot model. Pre-operative MR/CT images of the heart are segmented using the open source image-guided therapy software, 3D Slicer, to obtain models of the left atrium and septal wall. These models are input to the optimization algorithm to evaluate the optimal transseptal puncture location. Funding:
|
Using KinectTM and a Haptic Interface for Implementation of Real-Time Virtual Fixtures
|
Publication: Proceedings of the 2nd Workshop on RGB-D: Advanced Reasoning with Depth Cameras, June 2011. | PDF Authors: Ryden F, Chizeck HJ, Kosari SN, King H, Hannaford B. Institution: BioRobotics Laboratory, University of Washington, Seattle, WA, USA. Background/Purpose: The use of haptic virtual fixtures is a potential tool to improve the safety of robotic and telerobotic surgery. They can “push back” on the surgeon to prevent unintended surgical tool movements into protected zones. Previous work has suggested generating virtual fixtures from preoperative images like CT scans. However these are difficult to establish and register in dynamic environments. This paper demonstrates automatic generation of real-time haptic virtual fixtures using a low cost Xbox KinectTMdepth camera connected to a virtual environment. This allows generation of virtual fixtures and calculation of haptic forces, which are then passed on to a haptic device. This paper demonstrates that haptic forces can be successfully rendered from real-time environments containing both non-moving and moving objects. This approach has the potential to generate virtual fixtures from the patient in real-time during robotic surgery. Funding:
|
Multiple Indices of Diffusion Identifies White Matter Damage in Mild Cognitive Impairment and Alzheimer's Disease
|
Publication: PLoS One. 2011 Jun;6(6):e21745. PMID: 21738785 | PDF Authors: O'Dwyer L, Lamberton F, Bokde AL, Ewers M, Faluyi YO, Tanner C, Mazoyer B, O'Neill D, Bartley M, Collins DR, Coughlan T, Prvulovic D, Hampel H. Institution: Department of Psychiatry, Psychosomatic Medicine and Psychotherapy, Goethe University, Frankfurt, Germany. Background/Purpose: The study of multiple indices of diffusion, including axial (DA), radial (DR) and mean diffusion (MD), as well as fractional anisotropy (FA), enables WM damage in Alzheimer's disease (AD) to be assessed in detail. Here, tract-based spatial statistics (TBSS) were performed on scans of 40 healthy elders, 19 non-amnestic MCI (MCIna) subjects, 14 amnestic MCI (MCIa) subjects and 9 AD patients. Significantly higher DA was found in MCIna subjects compared to healthy elders in the right posterior cingulum/precuneus. Significantly higher DA was also found in MCIa subjects compared to healthy elders in the left prefrontal cortex, particularly in the forceps minor and uncinate fasciculus. In the MCIa versus MCIna comparison, significantly higher DA was found in large areas of the left prefrontal cortex. For AD patients, the overlap of FA and DR changes and the overlap of FA and MD changes were seen in temporal, parietal and frontal lobes, as well as the corpus callosum and fornix. Analysis of differences between the AD versus MCIna, and AD versus MCIa contrasts, highlighted regions that are increasingly compromised in more severe disease stages. Microstructural damage independent of gross tissue loss was widespread in later disease stages. Our findings suggest a scheme where WM damage begins in the core memory network of the temporal lobe, cingulum and prefrontal regions, and spreads beyond these regions in later stages. DA and MD indices were most sensitive at detecting early changes in MCIa. |
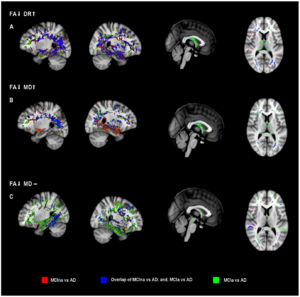 Analysis of disease progression with MCIna versus AD, and, MCIa versus AD. MCIna versus AD is shown in red, MCIa versus AD is shown in green, and areas where these contrasts overlap is shown in blue. (a) FA decreases together with DR increases. (b) FA decreases together with MD increases. (c) FA decreases where MD remains unchanged. See text main text for anatomical description and explanation of the three combinations of indices. Areas of significant difference were visualized using the 3D Slicer program. |
Assessment of Abdominal Adipose Tissue and Organ Fat Content by Magnetic Resonance Imaging
|
Publication: Obes Rev. 2011 May; 12(501):e504-15. PMID: 21348916 | PDF Authors: Hu HH, Nayak KS, Goran MI. Institution: Ming Hsieh Department of Electrical Engineering, Viterbi School of Engineering, University of Southern California, Los Angeles, CA, USA. Background/Purpose: As the prevalence of obesity continues to rise, rapid and accurate tools for assessing abdominal body and organ fat quantity and distribution are critically needed to assist researchers investigating therapeutic and preventive measures against obesity and its comorbidities. Magnetic resonance imaging (MRI) is the most promising modality to address such need. It is non-invasive, utilizes no ionizing radiation, provides unmatched 3D visualization, is repeatable, and is applicable to subject cohorts of all ages. This article is aimed to provide the reader with an overview of current and state-of-the-art techniques in MRI and associated image analysis methods for fat quantification. The principles underlying traditional approaches such as T(1) -weighted imaging and magnetic resonance spectroscopy as well as more modern chemical-shift imaging techniques are discussed and compared. The benefits of contiguous 3D acquisitions over 2D multislice approaches are highlighted. Typical post-processing procedures for extracting adipose tissue depot volumes and percent organ fat content from abdominal MRI data sets are explained. Furthermore, the advantages and disadvantages of each MRI approach with respect to imaging parameters, spatial resolution, subject motion, scan time and appropriate fat quantitative endpoints are also provided. Practical considerations in implementing these methods are also presented. Funding:
|
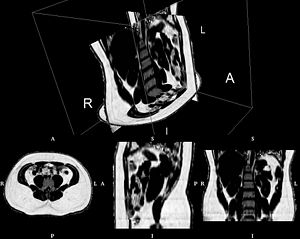 Abdominal fat fraction volume from IDEAL, illustrating the contiguous 3D nature of the data. The volume consists of more than 70 native axial slices and was obtained with five 15 second breath-holds (R: right, L: left, A: anterior, P: posterior, I: inferior, S: superior). Rendering created with 3D Slicer software. |
Subject-specific Musculoskeletal Modeling of the Lower Extremities in Persons with Unilateral Cerebral Palsy
|
Publication: Technical Report 2011 May; | PDF Author: Olesya Klets Institution: Department of Mechanics, Royal Institute of Technology, Stockholm, Sweden. Background/Purpose: The computational musculoskeletal models that are used to study muscle moment-generating capacities of persons with movement disorders and planning treatment options must be accurate, and take into account the inter-individual variability of musculoskeletal geometry. In Paper I the methods of creating the subject-specific musculoskeletal model of the lower extremities from magnetic resonance images (MRIs) were developed. The subject-specific model was used to analyze hip, knee and ankle muscle moment arms (MALs) and muscle-tendon lengths (MTLs) during gait in a subject with unilateral cerebral palsy (CP), and to evaluate the accuracy of widespread and commonly used scaled generic model. It was found that the scaled generic model delivered accurate values for changes in MTLs in most muscles. However, the scaled generic and the subject-specific lower extremity musculoskeletal models showed substantial differences in MALs calculated during gait. In Paper II subject-specific musculoskeletal models of nine subjects with unilateral CP were created to study muscles volumes, MTLs and MALs; and to examine the accuracy of MALs calculated by the scaled generic models. It was shown that the scaled generic model significantly underestimated hip MALs discrepancies between the affected and the non-affected sides of the lower extremities. However, it significantly overestimated hip adduction/abduction of gluteus maximus, gluteus medius, gluteus minimus, tensor fascia latae and biceps femoris long head; and hip flexion of adductor longus and rectus femoris in the affected and the non-affected sides. It was also found that muscle volumes and hip abduction MALs in gluteus medius and gluteus minimus, hip flexion MALs in iliacus and hip rotation in gluteus maximus were smaller in the affected side of lower extremities. MTLs in the affected and the non-affected sides throughout the range of hip motion were similar. This thesis suggests the need for the subject-specific musculoskeletal models that can account for variability of muscle attachments and musculoskeletal geometry of persons with movement disorders. Based on inaccuracies of the scaled generic model reported here, the generic models that are used to guide treatment decisions must be tested, and interpreted with care. Funding:
|
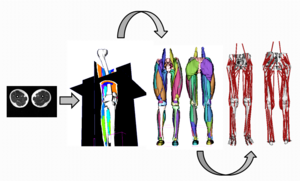 The workflow of building subject-specific musculoskeletal model of the lower extremities from MRIs. Bones and muscles contours were manually outlined by assigning label maps, where each voxel is a number indicating the type of tissue at that location in 3D Slicer, which is a free open- source software for visualization and image computing and can perform different medical image processing activities including surface reconstruction from MRI. |
|
Publication: Neurobiol Aging. 2011 May;32(5):916-32. PMID: 19570593 | PDF Authors: Walhovd KB, Westlye LT, Amlien I, Espeseth T, Reinvang I, Raz N, Agartz I, Salat DH, Greve DN, Fischl B, Dale AM, Fjell AM. Institution: Center for the Study of Human Cognition, Department of Psychology, University of Oslo, Norway. Background/Purpose: Magnetic resonance imaging (MRI) is the principal method for studying structural age-related brain changes in vivo. However, previous research has yielded inconsistent results, precluding understanding of structural changes of the ageing brain. This inconsistency is due to methodological differences and/or different aging patterns across samples. To overcome these problems, we tested age effects on 17 different neuroanatomical structures and total brain volume across five samples, of which one was split to further investigate consistency (883 participants). Widespread age-related volume differences were seen consistently across samples. In four of the five samples, all structures, except the brainstem, showed age-related volume differences. The strongest and most consistent effects were found for cerebral cortex, pallidum, putamen and accumbens volume. Total brain volume, cerebral white matter, caudate, hippocampus and the ventricles consistently showed non-linear age functions. Healthy aging appears associated with more widespread and consistent age-related neuroanatomical volume differences than previously believed. Funding:
|
Enhancement of a Master-Slave Robotic System for Natural Orifice Transluminal Endoscopic Surgery
|
Publication: Ann Acad Med Singapore. 2011 May;40(5):223-30. PMID: 21678013 | PDF Authors: Sun Z, Ang RY, Lim EW, Wang Z, Ho KY, Phee SJ. Institution: School of Mechanical & Aerospace Engineering, Nanyang Technological University, Singapore. Background/Purpose: A novel robotic platform for Natural Orifice Transluminal Endoscopic Surgery (NOTES) is presented in this paper. It aims to tackle two crucial technical barriers which hinder its smooth transition from animal studies to clinical trials: providing effective instrumentations to perform complex NOTES procedures and maintaining the spatial orientation for endoscopic navigation. Materials and Methods: The technical barriers are overcome by the design of the robotic system considering size, triangulation, dexterity, maneuverability and complexity. It is also shown that haptic feedback and interventional navigation system could solve the problem of off-axis manipulation of the camera angle and loss of spatial orientation upon entering the peritoneal cavity in transgastric NOTES procedure, respectively. Results: Successful ESD (endoscopic submucosal dissection) and wedge hepatic resection have been performed on live pigs with our Master And Slave Transluminal Endoscopic Robot (MASTER) system, showing its capability to perform advanced endoscopic surgical and NOTES procedures. It is found that the MASTER exhibited good grasping and cutting efficiency. And the lesion resection time could be significantly reduced with more practice between the endoscopist and the robot operator. Conclusion: This study evaluates the feasibility of MASTER system as a platform overcoming the barriers to NOTES. It is also demonstrated that the MASTER could effectively mitigate the technical constraints normally encountered in NOTES procedures. |
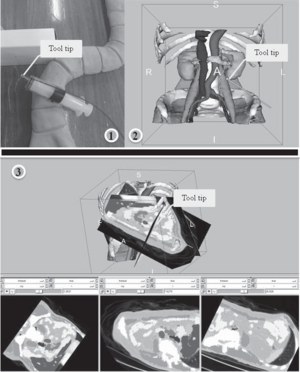 Real-time tracking system in the 3D Slicer interface. |
Brain Regional Lesion Burden and Impaired Mobility in the Elderly
|
Publication: Neurobiol Aging. 2011 Apr;32(4):646-54. PMID: 19428145 | PDF Authors: Moscufo N, Guttmann C, Meier D, Csapo I, Hildenbrand P, Healy B, Schmidt J, Wolfson L Institution: Center for Neurological Imaging, Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: This study investigated the relationship of brain white matter (WM) lesions affecting specific neural networks with decreased mobility in ninety-nine healthy community-dwelling subjects ≥75 years old prospectively enrolled by age and mobility status. We assessed lesion burden in the genu, body and splenium of corpus callosum; anterior, superior and posterior corona radiata; anterior and posterior limbs of internal capsule; corticospinal tract; and superior longitudinal fasciculus. Burden in the splenium of corpus callosum (SCC) demonstrated the highest correlation particularly with walking speed (r=0.4, p<10-4), and in logistic regression it was the best regional predictor of low mobility performance. We also found that independent of mobility, corona radiata has the largest lesion burden with anterior (ACR) and posterior (PCR) aspects being the most frequently affected. The results suggest that compromised inter-hemispheric integration of visuospatial information through the SCC plays an important role in mobility impairment in the elderly. The relatively high lesion susceptibility of ACR and PCR in all subjects may obscure the importance of these lesions in mobility impairment. 3D Slicer application has been used in all the imaging analysis steps, which included intracranial cavity outline, one- and two-channel brain tissue segmentation, labelmap outputs expert review and manual correction, image comparison, volume determination, and three-dimensional modeling. Funding:
|
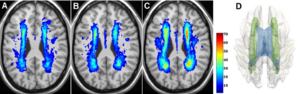 White matter lesion distribution and frequency (color bar) in the study subjects at baseline: normal (A), intermediate (B), and impaired (C) mobility. Panel D shows a 3D model reconstruction of the most affected structure, the corona radiata (green), within the white matter (transparent gray), and with ventricles (blue) also shown. |
Three Dimensional in Vivo Modelling of Vestibular Schwannomas and Surrounding Cranial Nerves using Diffusion Imaging Tractography
|
Publication: Neurosurgery. 2011 Apr;68(4):1077-83. PMID: 21242825 Authors: Chen DQ, Quan J, Guha A, Tymianski M, Mikulis D, Hodaie M. Institution: Division of Neurosurgery, Toronto Western Hospital and University of Toronto, Toronto, Ontario, Canada. Background/Purpose: Preservation of cranial nerves (CN) is of paramount concern in the treatment of vestibular schwannomas (VS), particularly in large tumors with thinned and distorted CN fibers. However, imaging of the CN fibers surrounding VS has been limited using 2D imaging alone. We assessed whether tractography of the CN combined with anatomical MR imaging of the tumor can provide superior 3D visualization of tumor/CN complexes. 3T MR imaging including diffusion tensor imaging (DTI) and anatomical images were analyzed in three subjects with VS using 3D Slicer software. The DTI images were used to tract the courses of trigeminal, abducens, facial, and vestibulocochlear nerves. The anatomical images were used to model the 3D volume reconstruction of the tumor. The two sets of images were then superimposed using linear registration. Combined 3D tumor modelling and cranial nerve tractography can effectively and consistently reconstruct the 3D spatial relationship of CN/tumor complexes, and allows for superior visualization compared with 2D imaging. Lateral and superior distortion of the trigeminal nerve was observed in all cases. The position of the facial nerve was primarily anteriorly and inferiorly. The Gasserian ganglion and early postganglionic branches could also be visualized. Tractography and anatomical imaging were successfully combined to demonstrate the precise location of surrounding CN fibers. This technique can be useful in both neuronavigation and radiosurgical planning. Since knowledge of the course of these fibers is of important clinical interest, implementation of this technique may help decrease injury to cranial nerves during treatment of these lesions. |
|
Publication: Neurosurgery. 2011 Apr;68(4):1077-83. PMID: 21135719 | PDF
Institution: Surgical Planning Laboratory, Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Brain surgery faces important challenges when trying to achieve maximum tumor resection while avoiding post-operative neurological deficits. In order for surgeons to have optimal intraoperative information concerning white matter anatomy, we developed a platform that allows the intra-operative real-time querying of tractography datasets during frameless stereotactic neuronavigation. Structural magnetic resonance imaging (MRI), functional MRI, and diffusion tensor imaging (DTI) were performed on 5 patients before undergoing lesion resection using neuronavigation. During the procedure, the tracked surgical tool tip position was transferred from the navigation system to the 3D Slicer software package, which used this position to seed the white matter tracts around the tool tip location, rendering a geometric visualization of these tracts on the pre-operative images previously loaded onto the navigation system. The clinical feasibility of this approach was evaluated during five cases of lesion resection. In addition, system performance was evaluated by measuring the latency between surgical tool tracking and visualization of the seeded white matter tracts. Lesion resection was performed successfully in all five patients. The seeded white matter tracts close to the lesion and other critical structures, as defined by the functional and structural images, were interactively visualized during the intervention to determine their spatial relationships relative to the lesion and critical cortical areas. Latency between tracking and visualization of tracts was less than a second for fiducial radius size of 4-5mm. Interactive tractography can provide an intuitive way of inspecting critical white matter tracts in the vicinity of the surgical region, allowing the surgeon to have increased intra-operative white matter information to execute the planned surgical resection. Funding:
|
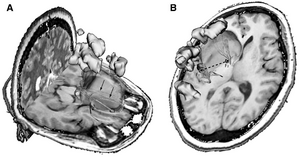 Images shown in the 3D Slicer using the intraoperative tractography navigation software module. The light green volume delineates the tumor location, the orange sphere represents the seed fiducial that is located at the tracked surgical tool tip location, the yellow regions indicate eloquent cortex as shown by language task-associated functional magnetic resonance imaging, and the tubular fibers represent the white matter tracts seeded by the fiducial location. White matter tracts are color coded according to their fractional anisotropy (color scale). A, white matter fibers being seeded by a fiducial representing tool tip position. Some infiltrating fibers can be seen within the segmented tumor volume (arrows). B, intraoperative querying of tractography data sets using the tool offset function. Fiducials F1 and F2 represent the surgical tool tip location and a fixed geometric offset respectively. The navigation module allows for geometric offsets from 280 to 80 mm from the tool tip position. The 2 fiducials can seed the tractography data set simultaneously. |
Three-dimensional Visualization of Subdural Electrodes for Presurgical Planning
|
Publication: Neurosurgery. 2011 Mar;68(1 Suppl Operative):152-60; discussion 160-1. PMID: 21206319 | PDF Authors: LaViolette PS, Rand SD, Raghavan M, Ellingson BM, Schmainda KM, Mueller W. Institution: Department of Biophysics, Medical College of Wisconsin, Milwaukee, WI, USA. Background/Purpose: Accurate localization and visualization of subdural electrodes implanted for intracranial electroencephalography in cases of medically refractory epilepsy remains a challenging clinical problem. |
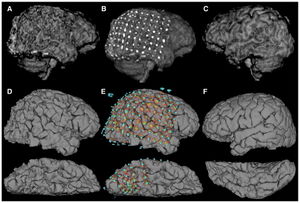 Comparison of 3D representations of the same cortex (patient S6). A, 3D volume rendering of the right hemisphere produced by skull stripping and 3D rendering with the Analyze software package, compared with D produced with Freesurfer software (ventral surface below). B and E show projections of electrodes onto the corresponding brain surfaces. Gyral and sulcal patterns are clearly visible in D and E, but are distorted in A and B by metallic electrode susceptibility artifacts. C and F show the corresponding cortical reconstructions of the unimplanted left hemisphere. Freesurfer-generated pial surfaces bearing electrode shadow were loaded into 3D Slicer for viewing. |
Segmentations of MRI Images of the Female Pelvic Floor: A Study of Inter- and Intra-reader Reliability
|
Publication: J Magn Reson Imaging. 2011 Mar;33(3):684-91. PMID: 21563253 | PDF Authors: Hoyte L, Ye W, Brubaker L, Fielding JR, Lockhart ME, Heilbrun ME, Brown MB, Warfield SK; Pelvic Floor Disorders Network Institution: Urogynecology Division, College of Medicine, University of South Florida, Tampa, FL, USA. Background/Purpose: To describe the inter- and intra-operator reliability of segmentations of female pelvic floor structures. Materials and Methods: Three segmentation specialists were asked to segment out the female pelvic structures in 20 MR datasets on three separate occasions using the 3D Slicer software. The STAPLE algorithm was used to compute inter- and intra-segmenter agreement of each organ in each dataset. STAPLE computed the sensitivity, specificity, and positive predictive values (PPV) for inter- and intra-segmenter repeatability. These parameters were analyzed using intra-class correlation analysis. Correlation of organ volume to PPV and sensitivity was also computed.
|
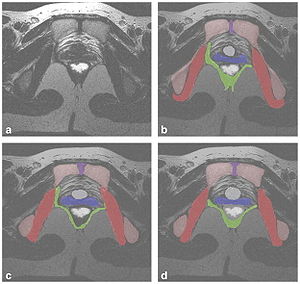 a–d: A sample T2-weighted axial MRI slice, taken at the level of the bladder neck is given in Figure 2a. Example individual segmentations of all organs from each of the three readers is given in Figure 2b–d. Legend: red, obturator internus; green, levator ani; blue, vagina; white, rectum; gray, bladder neck; violet, symphysis; pink, pelvic bones. |
3D Visualization of Subdural Electrode Shift as Measured at Craniotomy Reopening
|
Publication: Epilepsy Res. 2011 Mar;94(1-2):102-9. PMID: 21334178 | PDF Authors: LaViolette PS, Rand SD, Ellingson BM, Raghavan M, Lew SM, Schmainda KM, Mueller W. Institution: Department of Biophysics, Medical College of Wisconsin, Milwaukee, WI, USA. Background/Purpose: Subdural electrodes are implanted for recording intracranial EEG (iEEG) in cases of medically refractory epilepsy as a means to locate cortical regions of seizure onset amenable to surgical resection. Without the aid of imaging-derived 3D electrode models for surgical planning, surgeons have relied on electrodes remaining stationary from the time between placement and follow-up resection. This study quantifies electrode shift with respect to the cortical surface occurring between electrode placement and subsequent reopening. |
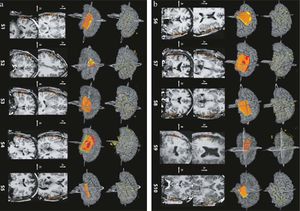 Patients S1—S5 grid placement and shift maps. Top row shows CT-derived electrode models overlaid on post-grid MRI-derived 3D brain surface models. Row 2 shows reconstructed grid sheet models overlaid on the 3D brain model. Sheets are limited to those electrodes whose positions were visible and available for measurement in the OR (at the discretion of the surgeon). Yellow sheet indicates CT-derived electrode positions, Red indicates Stealth OR coordinate-derived sheet, and Orange indicates overlap. Rows 3 and 4 show coronal and axial slices indicating location of red and yellow sheets above. Slices shown are included in the 3D rendering in Rows 1 and 2 (b) Patients S6—S10 grid placement and shift maps. Freesurfer-generated pial surfaces were loaded into 3D Slicer for viewing. |
Lung Volumes and Emphysema in Smokers with Interstitial Lung Abnormalities
|
Publication: N Engl J Med. 2011 Mar 10;364(10):897-906. PMID: 21388308 | PDF Authors: Washko GR, Hunninghake GM, Fernandez IE, Nishino M, Okajima Y, Yamashiro T, Ross JC, Estépar RS, Lynch DA, Brehm JM, Andriole KP, Diaz AA, Khorasani R, D'Aco K, Sciurba FC, Silverman EK, Hatabu H, Rosas IO. Institution: Pulmonary and Critical Care Division, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Cigarette smoking is associated with emphysema and radiographic interstitial lung abnormalities. The degree to which interstitial lung abnormalities are associated with reduced total lung capacity and the extent of emphysema is not known. We looked for interstitial lung abnormalities in 2416 (96%) of 2508 high-resolution computed tomographic (HRCT) scans of the lung obtained from a cohort of smokers. We used linear and logistic regression to evaluate the associations between interstitial lung abnormalities and HRCT measurements of total lung capacity and emphysema. Quantitative measures of total lung capacity and emphysema were performed with the Airway Inspector, the tool based on 3D Slicer for lung image analysis. Funding:
|
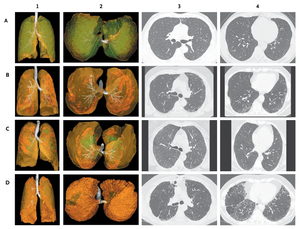 Four Major Radiographic Subtypes of Interstitial Lung Abnormalities. Each row of radiographs and reconstructions represents data from a single study participant. The images in Panel A are characteristic of centrilobular interstitial lung abnormalities; Panel B, subpleural interstitial lung abnormalities; Panel C, mixed centrilobular and subpleural interstitial lung abnormalities; and Panel D, radiographic interstitial lung disease. The images in the first two columns are three-dimensional reconstructions of an anterior-to-posterior view of the lungs (column 1) and a caudal-to-cephalad view (column 2). The translucent yellow-green represents the lung parenchyma; white, the tracheobronchial tree; opaque green, centrilobular opacities; and opaque orange, subpleural abnormalities. Columns 3 and 4 present axial high-resolution computed tomographic images of the chest, with images in column 3 approximately at the level of the carina and those in column 4 approximately at the level of the right inferior pulmonary vein. |
Integration of 3D Anatomical Data Obtained by CT Imaging and 3D Optical Scanning for Computer Aided Implant Surgery
|
Publication: BMC Medical Imaging 2011 Feb; 11:5. PMID: 21338504 | PDF Authors: Frisardi G, Chessa G, Barone S, Paoli A, Razionale A, Frisardi F. Institution: "Epochè" Orofacial Pain Center, Nettuno (Rome), Italy. Background/Purpose: A precise placement of dental implants is a crucial step to optimize both prosthetic aspects and functional constraints. In this context, the use of virtual guiding systems has been recognized as a fundamental tool to control the ideal implant position. In particular, complex periodontal surgeries can be performed using preoperative planning based on CT data. The critical point of the procedure relies on the lack of accuracy in transferring CT planning information to surgical field through custom-made stereo-lithographic surgical guides. Methods: In this work, a novel methodology is proposed for monitoring loss of accuracy in transferring CT dental information into periodontal surgical field. The methodology is based on integrating 3D data of anatomical (impression and cast) and preoperative (radiographic template) models, obtained by both CT and optical scanning processes. A clinical case, relative to a fully edentulous jaw patient, has been used as test case to assess the accuracy of the various steps concurring in manufacturing surgical guides. In particular, a surgical guide has been designed to place implants in the bone structure of the patient. The analysis of the results has allowed the clinician to monitor all the errors, which have been occurring step by step manufacturing the physical templates. The use of an optical scanner, which has a higher resolution and accuracy than CT scanning, has demonstrated to be a valid support to control the precision of the various physical models adopted and to point out possible error sources. A case study regarding a fully edentulous patient has confirmed the feasibility of the proposed methodology. |
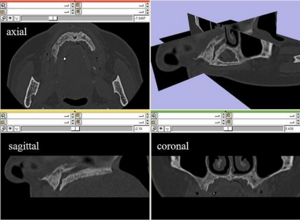 Maxilla CT data in the axial, sagittal and coronal planes and a full 3D view in 3D Slicer. |
Anisotropy of Transcallosal Motor Fibres Indicates Functional Impairment in Children with Periventricular Leukomalacia
|
Publication: Dev Med Child Neurol. 2011 Feb;53(2):179-86. PMID: 21121906 | PDF Authors: Koerte I, Pelavin P, Kirmess B, Fuchs T, Berweck S, Laubender RP, Borggraefe I, Schroeder S, Danek A, Rummeny C, Reiser M, Kubicki M, Shenton ME, Ertl-Wagner B, Heinen F. Institution: Institute of Clinical Radiology, Ludwig-Maximilians-University, Munich, Germany. Background/Purpose: In children with bilateral spastic cerebral palsy (CP), periventricular leukomalacia (PVL) is commonly identified on magnetic resonance imaging. We characterized this white matter condition by examining callosal microstructure, interhemispheric inhibitory competence (IIC), and mirror movements. Method: We examined seven children (age range 11y 9mo-17y 9mo, median age 15y 10mo, four females, three males) with bilateral spastic CP/PVL (Gross Motor Function Classification System level I or II, Manual Ability Classification System level I) and 12 age-matched controls (age range 11y 7mo-17y 1mo, median age 15y 6mo, seven females, five males). Fractional anisotropy of the transcallosal motor fibres (TCMF) and the corticospinal tract (CST) of both sides were calculated. The parameters of IIC (transcranial magnetic stimulation) and mirror movements were measured using a standardized clinical examination and a computer-based hand motor test. Results Fractional anisotropy was lower in children with bilateral spastic CP/PVL regarding the TCMF, but not the left or right CST. Resting motor threshold was elevated in children with bilateral spastic CP/PVL whereas measures of IIC tended to be lower. Mirror movements were markedly elevated in bilateral spastic CP/PVL. Interpretation This study provides new information on different aspects of motor function in children with bilateral spastic CP/PVL. Decreased fractional anisotropy of TCMF is consistent with impairment of hand motor function in children with bilateral spastic CP/PVL. The previously overlooked microstructure of the TCMF may serve as a potential indicator for hand motor function in patients with bilateral spastic CP/PVL. Funding:
|
Automatic Lung Segmentation in CT Images with Accurate Handling of the Hilar Region
|
Publication: J Digit Imaging. 2011 Feb;24(1):11-27. PMID: 19826872 | PDF Authors: De Nunzio G, Tommasi E, Agrusti A, Cataldo R, De Mitri I, Favetta M, Maglio S, Massafra A, Quarta M, Torsello M, Zecca I, Bellotti R, Tangaro S, Calvini P, Camarlinghi N, Falaschi F, Cerello P, Oliva P. Institution: Department of Materials Science, University of Salento, and INFN, Lecce, Italy. Background/Purpose: A fully automated and three-dimensional (3D) segmentation method for the identification of the pulmonary parenchyma in thorax X-ray computed tomography (CT) datasets is proposed. It is meant to be used as pre-processing step in the computer-assisted detection (CAD) system for malignant lung nodule detection that is being developed by the Medical Applications in a Grid Infrastructure Connection (MAGIC-5) Project. In this new approach the segmentation of the external airways (trachea and bronchi), is obtained by 3D region growing with wavefront simulation and suitable stop conditions, thus allowing an accurate handling of the hilar region, notoriously difficult to be segmented. Particular attention was also devoted to checking and solving the problem of the apparent 'fusion' between the lungs, caused by partial-volume effects, while 3D morphology operations ensure the accurate inclusion of all the nodules (internal, pleural, and vascular) in the segmented volume. The new algorithm was initially developed and tested on a dataset of 130 CT scans from the Italung-CT trial, and was then applied to the ANODE09-competition images (55 scans) and to the LIDC database (84 scans), giving very satisfactory results. In particular, the lung contour was adequately located in 96% of the CT scans, with incorrect segmentation of the external airways in the remaining cases. Segmentation metrics were calculated that quantitatively express the consistency between automatic and manual segmentations: the mean overlap degree of the segmentation masks is 0.96 ± 0.02, and the mean and the maximum distance between the mask borders (averaged on the whole dataset) are 0.74 ± 0.05 and 4.5 ± 1.5, respectively, which confirms that the automatic segmentations quite correctly reproduce the borders traced by the radiologist. Moreover, no tissue containing internal and pleural nodules was removed in the segmentation process, so that this method proved to be fit for the use in the framework of a CAD system. Finally, in the comparison with a two-dimensional segmentation procedure, inter-slice smoothness was calculated, showing that the masks created by the 3D algorithm are significantly smoother than those calculated by the 2D-only procedure. Funding:
|
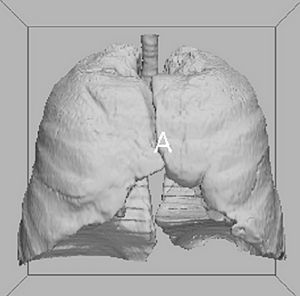 3D binary mask of the respiratory system (step B output). It contains both the external airways (trachea and bronchi) and the lungs. The picture (and the following 3D ones) were rendered by the 3D Slicer visualization and processing software package. |
Using 3D Slicer in Astronomy
|
Institution: The Initiative in Innovative Computing (IIC), Harvard University, Cambridge, MA, USA. Project: IIC AstroMed Project Background/Purpose: While astronomy and medical imaging seem very different, both fields search large amounts of image data looking for meaningful patterns. For example, a physician may inspect a patient's MRI scans looking for signs of disease, while an astronomer will analyze radio telescope image data to find evidence of a new star being born. The two sciences have separately developed many techniques to analyze, visualize, and catalog complex multi-dimensional imaging data, but seldom have experts from the two areas worked together. The 3D Slicer software package is AstroMed's core tool for astronomical 3D data visualization. Originally designed for medical image analysis, 3D Slicer has many capabilities that are uncommon in astronomy software. The AstroMed project brings together researchers from the Harvard Medical School and the Harvard-Smithsonian Center for Astrophysics, along with both national and international collaborators, to combine their knowledge and advance the state-of-the-art in both medical imaging and astronomy. Related article in the February 11, 2011 issue of Science Magazine. |
Brain Morphometry in Autism Spectrum Disorders: A Unified Approach for Structure-specific Statistical Analysis of Neuroimaging Data
|
Publication: Biomed Sci Instrum. 2011;47:135-41. PMID: 21525610 Authors: Vatta F, Di Salle F. Institution: Maastricht University, Maastricht, The Netherlands. Background/Purpose: Autism spectrum disorders (ASD) are a neurodevelopmental condition with multiple causes, comorbid conditions, and a wide range in the type and severity of symptoms expressed by different individuals. This makes the neuroanatomy of autism inherently difficult to describe. It has been assumed in the scientific literature that deviations in regional brain size in clinical samples are directly related to maldevelopment or pathogenesis. The performed clinical studies analyzed specific brain structures that are assumed to be correlated to autistic brain behaviors. Examples of performed analyses, based upon manual or semi-automated segmentation from magnetic resonance imaging (MRI) scans, include volumetric measures of specific brain structures, or small groups of structures, as caudate, corpus callosum, putamen, hippocampus, nucleus accumbens, evaluating differences between groups of subjects with autism and control subjects. Nonetheless, the brain regions analyzed that differ between patients and control subjects have not been always consistent over the performed studies. This inconsistency might be due to the fact that the specific single volume differences that have been reported in the literature for the different brain structures under investigation may, instead, be not independent during pathogenesis. Hence, this issue comes into play in logically framing a comprehensive assessment of putative abnormalities in regional brain volumes. To this aim, a whole brain investigation system for a semi-automated morphometric statistical analysis of brain anatomy is presented in this paper and validated on a selected group of patients diagnosed with ASD that completed a 1.5 T magnetic resonance image (MRI) of the brain. The proposed system, which is mainly built basing upon the FreeSurfer and the 3D Slicer software frameworks for the volumetric analysis of brain imaging data, lies its foundations on the higher statistical power of the region of interest (ROI) approach, but equally aims at a higher exploratory power as it doesn't restrict its focus to a small number of specific regions, thanks to a whole brain unified approach. |
Cognitive Profile and Brain Morphological Changes in Obstructive Sleep Apnea
|
Publication: Neuroimage. 2011 Jan 15;54(2):787-93. PMID: 20888921 | PDF Authors: Torelli F, Moscufo N, Garreffa G, Placidi F, Romigi A, Zannino S, Bozzali M, Fasano F, Giulietti G, Djonlagic I, Malhotra A, Marciani MG, Guttmann CR. Institution: Center for Neurological Imaging, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: Obstructive sleep apnea (OSA) is accompanied by neurocognitive impairment, likely mediated by injury to various brain regions. We evaluated brain morphological changes in patients with OSA and their relationship to neuropsychological and oximetric data. Sixteen patients affected by moderate-severe OSA (age: 55.8±6.7 years, 13 males) and fourteen control subjects (age: 57.6±5.1 years, 9 males) underwent 3.0 Tesla brain magnetic resonance imaging (MRI) and neuropsychological testing evaluating short- and long-term memory, executive functions, language, attention, praxia and non-verbal learning. Volumetric segmentation of cortical and subcortical structures and voxel-based morphometry (VBM) were performed. Patients and controls differed significantly in Rey Auditory-Verbal Learning test (immediate and delayed recall), Stroop test and Digit span backward scores. Volumes of cortical gray matter (GM), right hippocampus, right and left caudate were smaller in patients compared to controls, with also brain parenchymal fraction (a normalized measure of cerebral atrophy) approaching statistical significance. Differences remained significant after controlling for comorbidities (hypertension, diabetes, smoking, hypercholesterolemia). VBM analysis showed regions of decreased GM volume in right and left hippocampus and within more lateral temporal areas in patients with OSA. Our findings indicate that the significant cognitive impairment seen in patients with moderate-severe OSA is associated with brain tissue damage in regions involved in several cognitive tasks. We conclude that OSA can increase brain susceptibility to the effects of aging and other clinical and pathological occurrences. Funding:
|
 Series from 3D Slicer segmentation module. Figure shows a same-level slice from the MPRAGE (A), FLAIR (B) and T2 (C) series and the segmentation output of 3D Slicer module (D) which was obtained using MPRAGE and FLAIR as inputs. Colors in panel D: yellow (WM), pale blue (GM), pink (CSF), red (WMH) and white (putamen). The ICV is outlined in green (panel C) and includes cortical CSF. |
Go to 2017 :: 2016:: 2015 :: 2014-2011 :: 2010-2005