Main Page/SlicerCommunity
Contents
- 1 3D Slicer Enabled Research
- 2 2017
- 2.1 Biomaterial Shell Bending with 3D-printed Templates in Vertical and Alveolar Ridge Augmentation: A Technical Note
- 2.2 Application of the 3D Slicer Chest Imaging Platform Segmentation Algorithm for Large Lung Nodule Delineation
- 2.3 3D Printed Pathological Sectioning Boxes to Facilitate Radiological-Pathological Correlation in Hepatectomy Cases
- 2.4 Retrospective Validation of a Computer-Assisted Quantification Model of Intracerebral Hemorrhage Volume on Accuracy, Precision, and Acquisition Time, Compared with Standard ABC/2 Manual Volume Calculation
- 2.5 Theoretical Observation on Diagnosis Maneuver for Benign Paroxysmal Positional Vertigo
- 2.6 High Expression of Glypican-1 Predicts Dissemination and Poor Prognosis in Glioblastomas
- 2.7 1.5 T Augmented Reality Navigated Interventional MRI: Paravertebral Sympathetic Plexus Injections
- 2.8 3D Printing and Modelling of Customized Implants and Surgical GUides for Non-human Primates
- 2.9 Theoretical Observation on Diagnosis Maneuver for Benign Paroxysmal Positional Vertigo
- 2.10 Quality of Radiomic Features in Glioblastoma Multiforme: Impact of Semi-Automated Tumor Segmentation Software
- 2.11 Prognostic Implications of the Subcellular Localization of Survivin in Glioblastomas Treated with Radiotherapy Plus Concomitant and Adjuvant Temozolomide
- 2.12 An Ovine Model of Cerebral Catheter Venography for Implantation of an Endovascular Neural Interface
- 2.13 Effectiveness of Endoscopic Surgery for Supratentorial Hypertensive Intracerebral Hemorrhage: A Comparison with Craniotomy
- 2.14 Quantitative CT ventriculography for Assessment and Monitoring of Hydrocephalus: a Pilot Study and Description of Method in Subarachnoid Hemorrhage (SAH)
- 2.15 Infantile Cranial Fasciitis: Case-based Review and Operative Technique
- 2.16 The Effects of Iterative Reconstruction and Kernel Selection on Quantitative Computed Tomography Measures of Lung Density
- 2.17 Asymmetry in Dentition and Shape of Pharyngeal Arches in the Clonal Fish Chrosomus Eos-neogaeus: Phenotypic Plasticity and Developmental Instability
- 2.18 Scanning Laser Optical Tomography for in Toto Imaging of the Murine Cochlea.
- 2.19 Patient Education for Endoscopic Sinus Surgery: Preliminary Experience Using 3D-Printed Clinical Imaging Data
- 2.20 Comprehensive Evaluation of Ten Deformable Image Registration Algorithms for Contour Propagation between CT and Cone-beam CT Images in Adaptive Head & Neck Radiotherapy
- 2.21 A New Approach for Radiosynoviorthesis: A Dose-Optimized Planning method Based on Monte Carlo Simulation and Synovial Measurement Using 3D Slicer and MRI
- 2.22 Exercise Decreases Marrow Adipose Tissue Through ß-Oxidation in Obese Running Mice
- 2.23 Interactive Outlining of Pancreatic Cancer Liver Metastases in Ultrasound Images
- 2.24 The evolution of Cost-efficiency in Neural Networks during Recovery from Traumatic Brain Injury
- 2.25 Three‐Dimensional Printing: An Aid to Epidural Access for Neuromodulation
- 2.26 Biomechanical Flow Amplification Arising From the Variable Deformation of the Subglottic Mucosa
- 2.27 HTC Vive MeVisLab Integration via OpenVR for Medical Applications
- 2.28 What are the True Volumes of SEGA Tumors? Reliability of Planimetric and Popular Semi-automated Image Segmentation Methods
- 2.29 Anser EMT: The First Open-Source Electromagnetic Tracking Platform for Image-Guided Interventions
- 2.30 SLIDE: Automatic Spine Level Identification System using a Deep Convolutional Neural Network
- 2.31 Revealing Cancer Subtypes with Higher-Order Correlations Applied to Imaging and Omics Data
- 2.32 Three-Dimensional Volume Rendering of Pelvic Models and Paraurethral Masses Based on MRI Cross-Sectional Images
- 2.33 A Study of Volumetric Variations of Basal Nuclei in the Normal Human Brain by Magnetic Resonance Imaging
- 2.34 MITK-OpenIGTLink for Combining Open-Source Toolkits in Real-Time Computer-Assisted Interventions
- 2.35 Automated Catheter Navigation with Electromagnetic Image Guidance
- 2.36 Increased Cerebellar Gray Matter Volume in Head Chefs
- 2.37 Tumor Heterogeneity Assessed by Texture Analysis on Contrast-Enhanced CT in Lung Adenocarcinoma: Association with Pathologic Grade
- 2.38 Three-dimensional Printing of X-ray Computed Tomography Datasets with Multiple Materials using Open-source Data Processing
- 2.39 SEEG Assistant: A 3D Slicer Extension to Support Epilepsy Surgery
- 2.40 Associations of Radiomic Data Extracted from Static and Respiratory-Gated CT Scans with Disease Recurrence in Lung Cancer Patients Treated with SBRT
- 2.41 Early Experiences of Planning Stereotactic Radiosurgery using 3D Printed Models of Eyes with Uveal Melanomas
- 2.42 Intra-rater Variability in Low-grade Glioma Segmentation
- 2.43 Hybrid Positron Emission Tomography Segmentation of Heterogeneous Lung Tumors using 3D Slicer: Improved Growcut Algorithm with Threshold Initialization
- 2.44 Pre-clinical Validation of Virtual Bronchoscopy using 3D Slicer
- 2.45 Anatomical Study and Locating Nasolacrimal Duct on Computed Topographic Image
- 2.46 Intra-rater Variability in Low-grade Glioma Segmentation
- 2.47 Open Wedge High Tibial Osteotomy using Three-Dimensional Printed Models: Experimental Analysis using Porcine Bone
- 2.48 MRI Visible Fe3O4 Polypropylene Mesh: 3D Reconstruction of Spatial Relation to Bony Pelvis and Neurovascular Structures
3D Slicer Enabled Research
3D Slicer is a free open source software package distributed under a BSD style license. The majority of funding for the development of 3D slicer comes from a number of grants and contracts from the National Institutes of Health. See Slicer Acknowledgments for more information.
This page focuses on research that was done outside of our immediate collaboration community. That community is represented in the publication database.
We invite you to provide information on how you are using 3D Slicer to produce peer-reviewed research. Information about the scientific impact of this tool is helpful in raising funding for the continued support.
2016:: 2015 :: 2014-2011 :: 2010-2005
2017
Biomaterial Shell Bending with 3D-printed Templates in Vertical and Alveolar Ridge Augmentation: A Technical Note
|
Publication: Oral Surg Oral Med Oral Pathol Oral Radiol. 2017 Jun;123(6):651-60. PMID: 28215503 Authors: Draenert FG, Gebhart F, Mitov G, Neff A. Institution: Oral & Maxillofacial Surgery, University of Marburg, Germany. Background/Purpose:
Alveolar ridge and vertical augmentations are challenging procedures in dental implantology. Even material blocks with an interconnecting porous system are never completely resorbed. Shell techniques combined with autologous bone chips are therefore the gold standard. Using biopolymers for these techniques is well documented. We applied three-dimensional (3-D) techniques to create an individualized bending model for the adjustment of a plane biopolymer membrane made of polylactide.
|
Application of the 3D Slicer Chest Imaging Platform Segmentation Algorithm for Large Lung Nodule Delineation
|
Publication: PLoS One. 2017 Jun 8;12(6):e0178944. PMID: 28594880 | PDF Authors: Yip SSF, Parmar C, Blezek D, Estepar RSJ, Pieper S, Kim J, Aerts HJWL. Institution: Department of Radiation Oncology, Dana-Farber Cancer Institute, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. Background/Purpose: PURPOSE: Accurate segmentation of lung nodules is crucial in the development of imaging biomarkers for predicting malignancy of the nodules. Manual segmentation is time consuming and affected by inter-observer variability. We evaluated the robustness and accuracy of a publically available semiautomatic segmentation algorithm that is implemented in the 3D Slicer Chest Imaging Platform (CIP) and compared it with the performance of manual segmentation. METHODS: CT images of 354 manually segmented nodules were downloaded from the LIDC database. Four radiologists performed the manual segmentation and assessed various nodule characteristics. The semiautomatic CIP segmentation was initialized using the centroid of the manual segmentations, thereby generating four contours for each nodule. The robustness of both segmentation methods was assessed using the region of uncertainty (δ) and Dice similarity index (DSI). The robustness of the segmentation methods was compared using the Wilcoxon-signed rank test (pWilcoxon<0.05). The Dice similarity index (DSIAgree) between the manual and CIP segmentations was computed to estimate the accuracy of the semiautomatic contours. RESULTS: The median computational time of the CIP segmentation was 10 s. The median CIP and manually segmented volumes were 477 ml and 309 ml, respectively. CIP segmentations were significantly more robust than manual segmentations (median δCIP = 14ml, median dsiCIP = 99% vs. median δmanual = 222ml, median dsimanual = 82%) with pWilcoxon~10-16. The agreement between CIP and manual segmentations had a median DSIAgree of 60%. While 13% (47/354) of the nodules did not require any manual adjustment, minor to substantial manual adjustments were needed for 87% (305/354) of the nodules. CIP segmentations were observed to perform poorly (median DSIAgree≈50%) for non-/sub-solid nodules with subtle appearances and poorly defined boundaries. CONCLUSION: Semi-automatic CIP segmentation can potentially reduce the physician workload for 13% of nodules owing to its computational efficiency and superior stability compared to manual segmentation. Although manual adjustment is needed for many cases, CIP segmentation provides a preliminary contour for physicians as a starting point. Funding:
|
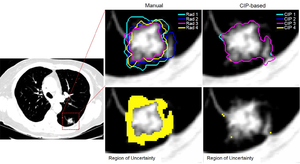 Comparison of manual (left) and CIP-based (right) segmentation. Yellow shaded region indicated the disagreement (or region of uncertainty) between contours performed by four radiologists (bottom left) or different CIP-based seed locations (bottom right). In this example, the region of uncertainty for manual segmentation was 3222 ml while the region was only 46 ml for the CIP-based segmentation. dsiCIP was ≈ 100%, while dsimanual was 88%. |
3D Printed Pathological Sectioning Boxes to Facilitate Radiological-Pathological Correlation in Hepatectomy Cases
|
Publication: J Clin Pathol. 2017 Jun 8. PMID: 28596154 Authors: Trout AT, Batie MR, Gupta A, Sheridan RM, Tiao GM, Towbin AJ. Institution: Department of Radiology, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, USA. Background/Purpose: Radiogenomics promises to identify tumour imaging features indicative of genomic or proteomic aberrations that can be therapeutically targeted allowing precision personalised therapy. An accurate radiological-pathological correlation is critical to the process of radiogenomic characterisation of tumours. An accurate correlation, however, is difficult to achieve with current pathological sectioning techniques which result in sectioning in non-standard planes. The purpose of this work is to present a technique to standardise hepatic sectioning to facilitateradiological-pathological correlation. We describe a process in which three-dimensional (3D)-printed specimen boxes based on preoperative cross-sectional imaging (CT and MRI) can be used to facilitate pathological sectioning in standard planes immediately on hepatic resection enabling improved tumour mapping. We have applied this process in 13 patients undergoing hepatectomy and have observed close correlation between imaging and gross pathology in patients with both unifocal and multifocal tumours. Following image review, a clinical engineering specialist (MRB) digitally isolates the liver from the cross-sectional imaging study using open-source software 3D Slicer. |
Retrospective Validation of a Computer-Assisted Quantification Model of Intracerebral Hemorrhage Volume on Accuracy, Precision, and Acquisition Time, Compared with Standard ABC/2 Manual Volume Calculation
|
Publication: AJNR Am J Neuroradiol. 2017 Jun 8. PMID: 28596188 Authors: Xue W, Vegunta S, Zwart CM, Aguilar MI, Patel AC, Hoxworth JM, Demaerschalk BM, Mitchell JR. Institution: Department of Biomedical Informatics, Arizona State University, Scottsdale, AZ, USA. Background/Purpose: BACKGROUND AND PURPOSE: Intracerebral hemorrhage accounts for 6.5%-19.6% of all acute strokes. Initial intracerebral hemorrhage volume and expansion are both independent predictors of clinical outcomes and mortality. Therefore, a rapid, unbiased, and precise measurement of intracerebral hemorrhage volume is a key component of clinical management. The most commonly used method, ABC/2, results in overestimation. We developed an interactive segmentation program, SegTool, using a novel graphic processing unit, level set algorithm. Until now, the speed, bias, and precision of SegTool had not been validated. MATERIALS AND METHODS: In a single stroke academic center, 2 vascular neurologists and 2 neuroradiologists independently performed a test-retest experiment that involved repeat measurements of static, unchanging intracerebral hemorrhage volumes on CT from 76 intracerebral hemorrhage cases. Measurements were made with SegTool and ABC/2. True intracerebral hemorrhage volumes were estimated from a consensus of repeat manual tracings by 2 operators. These data allowed us to estimate measurement bias, precision, and speed. Computer-assisted measurements were made with an intensity-threshold algorithm in 3D Slicer. RESULTS: The measurements with SegTool were not significantly different from the true intracerebral hemorrhage volumes, while ABC/2 overestimated volume by 45%. The interrater measurement variability with SegTool was 50% less than that with ABC/2. The average measurement times for ABC/2 and SegTool were 35.7 and 44.6 seconds, respectively. CONCLUSIONS: SegTool appears to have attributes superior to ABC/2 in terms of accuracy and interrater reliability with a 9-second delay in measurement time (on average); hence, it could be useful in clinical trials and practice. |
Theoretical Observation on Diagnosis Maneuver for Benign Paroxysmal Positional Vertigo
|
Publication: Acta Otolaryngol. 2017 Jun;137(6):567-71. PMID: 28084876 Authors: Yang XK, Zheng YY, Yang XG. Institution: Department of Neurology, Wenzhou People's Hospital, Wenzhou, Zhejiang, PR China. Background/Purpose: To make a comprehensive analysis with a variety of diagnostic maneuvers is conducive to the correct diagnosis and classification of BPPV. OBJECTIVE: Based on the standard spatial coordinate-based semicircular canal model for theoretical observation on diagnostic maneuvers for benign paroxysmal positional vertigo (BPPV) to analyze the meaning and key point of each step of the maneuver. MATERIALS AND METHODS: This study started by building a standard model of semicircular canal with space orientation by segmentation of the inner ear done with the 3D Slicer software based on MRI scans, then gives a demonstration and observation of BPPV diagnostic maneuvers by using the model. RESULTS: The supine roll maneuver is mainly for diagnosis of lateral semicircular canal BPPV. The Modified Dix-Hallpike maneuver is more specific for the diagnosis of posterior semicircular canal BPPV. The side-lying bow maneuver designed here is theoretically suitable for diagnosis of anterior semicircular canal BPPV. |
High Expression of Glypican-1 Predicts Dissemination and Poor Prognosis in Glioblastomas
|
Publication: World Neurosurg. 2017 Jun 5. PMID: 28602885 Authors:Saito T, Sugiyama K, Hama S, Yamasaki F, Takayasu T, Nosaka R, Onishi S, Muragaki Y, Kawamata T, Kurisu K. Institution: Department of Neurosurgery, Hiroshima University, Graduate School of Biomedical and Health Science, Hiroshima, Japan. Background/Purpose: OBJECTIVE: Glioblastoma (GBM) relapses locally or in a disseminated pattern, and is highly resistant to chemo-radiotherapy. Although dissemination is associated with poor prognosis for GBM patients, the clinico-pathological factors that promote dissemination have not been elucidated. Glypican-1 (GPC-1) is a heparin sulfate proteoglycan that is attached to the extracytoplasmic surface of the cell membrane and regulates cell motility. The aim of this study was to determine whether GPC-1 expression correlated with GBM dissemination and patient prognosis. METHODS: GPC-1 expression was examined by immunohistochemistry in 53 patients with GBM who received radiotherapy and temozolomide (TMZ) treatment. We assessed the relationship between dissemination and clinico-pathological factors, including GPC-1 expression. Additionally, we evaluated the relationship between GPC-1 expression and overall survival (OS) by uni- and multivariate analyses of a range of clinico-pathological factors, including age, Karnofsky Performance Status (KPS), extent of resection, and O6-methylguanine-DNA methyltransferase (MGMT) status. To evaluate the extent of resection by 13 semi-automatic volumetry, we used (http://www.slicer.org 3D Slicer], version 4.0 software. RESULTS: Logistic regression analysis revealed that GPC-1 expression correlated with dissemination (P = 0.0116). Log-rank tests revealed that age, KPS, extent of resection, MGMT status, dissemination (P = 0.0008) and GPC-1 expression (P = 0.0011) were significantly correlated with OS. Multivariate analysis indicated that age, MGMT status, and GPC-1 expression were significantly correlated with OS. GPC-1 expression had the highest hazard ratio (2.392) among all regressors. CONCLUSIONS: GPC-1 expression significantly correlated with OS in GBM patients who received radiotherapy and TMZ treatment. GPC-1 expression can help predict the occurrence of dissemination and shorter OS in GBM patients. |
|
Publication: Diagn Interv Radiol. 2017 May-Jun;23(3):227-32. PMID: 28420598 | PDF Authors: Marker DR, U Thainual P, Ungi T, Flammang AJ, Fichtinger G, Iordachita II, Carrino JA, Fritz J. Institution: Russel H. Morgan Department of Radiology and Radiological Science, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA. Background/Purpose: The high contrast resolution and absent ionizing radiation of interventional magnetic resonance imaging (MRI) can be advantageous for paravertebral sympathetic nerve plexus injections. We assessed the feasibility and technical performance of MRI-guided paravertebral sympathetic injections utilizing augmented reality navigation and 1.5 T MRI scanner. METHODS: A total of 23 bilateral injections of the thoracic (8/23, 35%), lumbar (8/23, 35%) and hypogastric (7/23, 30%) paravertebral sympathetic plexus were prospectively planned in twelve human cadavers using a 1.5 Tesla (T) MRI scanner and augmented reality navigation system. MRI-conditional needles were used. Gadolinium-DTPA-enhanced saline was injected. Outcome variables included the number of control magnetic resonance images, target error of the needle tip, punctures of critical nontarget structures, distribution of the injected fluid, and procedure length. The isotropic 3D MR images were transferred into the navigation module (PerkStation) of the 3D Slicer software for interactive 3D evaluation of the anatomy using its DICOM viewer function. RESULTS: Augmented-reality navigated MRI guidance at 1.5 T provided detailed anatomical visualization for successful targeting of the paravertebral space, needle placement, and perineural paravertebral injections in 46 of 46 targets (100%). A mean of 2 images (range, 1-5 images) were required to control needle placement. Changes of the needle trajectory occurred in 9 of 46 targets (20%) and changes of needle advancement occurred in 6 of 46 targets (13%), which were statistically not related to spinal regions (P = 0.728 and P = 0.86, respectively) and cadaver sizes (P = 0.893 and P 0.859, respectively). The mean error of the needle tip was 3.9±1.7 mm. There were no punctures of critical nontarget structures. The mean procedure length was 33±12 min. CONCLUSION: 1.5 T augmented reality-navigated interventional MRI can provide accurate imaging guidance for perineural injections of the thoracic, lumbar, and hypogastric sympathetic plexus. |
 Procedural photograph demonstrating the operator’s augmented reality consisting of a hybrid view of MR image and underlying cadaver. The hybrid view is being created by the reflection of the target MR image (black arrow) from a semitransparent mirror (white arrow) into the line of sight of the operator, where it merges with the underlying cadaver (gray arrow). Location, size, and skin contour of MR image and cadaver are matched through co-registration by the image-overlay navigation system. |
3D Printing and Modelling of Customized Implants and Surgical GUides for Non-human Primates
|
Publication: J Neurosci Methods. 2017 May 13. PMID: 28512008 Authors: Chen X, Possel JK, Wacongne C, van Ham AF, Klink PC, Roelfsema PR. Institution: Department of Vision & Cognition, Netherlands Institute for Neuroscience, Meibergdreef 47, 1105 BA, Amsterdam, Netherlands. Background/Purpose: Primate neurobiologists use chronically implanted devices such as pedestals for head stabilization and chambers to gain access to the brain and study its activity. Such implants are skull-mounted, and made from a hard, durable material, such as titanium. NEW METHOD: Here we present a low-cost method of creating customized 3D-printed cranial implants that are tailored to the anatomy of individual animals. We performed pre-surgical computed tomography (CT) and magnetic resonance (MR) scans to generate three-dimensional (3D) models of the skull and brain. We then used 3D modeling software to design implantable head posts, chambers, and a pedestal anchorage base, as well as craniotomy guides to aid us during surgery. Prototypes were made from plastic or resin, while implants were 3D-printed in titanium. The implants underwent post-processing and received a coating of osteocompatible material to promote bone integration. RESULTS: Their tailored fit greatly facilitated surgical implantation, and eliminated the gap between the implant and the bone. To date, our implants remain robust and well-integrated with the skull. COMPARISON WITH EXISTING METHOD(S): Commercial-off-the-shelf solutions typically come with a uniform, flat base, preventing them from sitting flush against the curved surface of the skull. This leaves gaps for fluid and tissue ingress, increasing the risk of microbial infection and tissue inflammation, as well as implant loss. CONCLUSIONS: The use of 3D printing technology enabled us to quickly and affordably create unique, complex designs, avoiding the constraints levied by traditional production methods, thereby boosting experimental success and improving the wellbeing of the animals. |
Theoretical Observation on Diagnosis Maneuver for Benign Paroxysmal Positional Vertigo
|
Publication: J Biomech. 2017 May 24;57:152-6. PMID: 28454908 Authors: Gray HA, Guan S, Pandy MG. Institution: Department of Mechanical Engineering, University of Melbourne, Victoria, Australia. Background/Purpose: The aim of this study was to evaluate the accuracy with which mobile biplane X-ray imaging can be used to measure patellofemoral kinematics of the intact knee during overground gait. A unique mobile X-ray imaging system tracked and recorded biplane fluoroscopic images of two human cadaver knees during simulated overground walking at a speed of 0.7m/s. Six-degree-of-freedom patellofemoral kinematics were calculated using a bone volumetric model-based method and the results then compared against those derived from a gold-standard bead-based method. RMS errors for patellar anterior translation, superior translation and lateral shift were 0.19mm, 0.34mm and 0.37mm, respectively. RMS errors for patellar flexion, lateral tilt and lateral rotation were 1.08°, 1.15° and 1.46°, respectively. The maximum RMS error for patellofemoral translations was approximately one-half that reported previously for tibiofemoral translations using the same mobile X-ray imaging system while the maximum RMS error for patellofemoral rotations was nearly two times larger than corresponding errors reported for tibiofemoral rotations. The lower accuracy in measuring patellofemoral rotational motion is likely explained by the symmetric nature of the patellar geometry and the smaller size of the patella compared to the tibia. |
Quality of Radiomic Features in Glioblastoma Multiforme: Impact of Semi-Automated Tumor Segmentation Software
|
Publication: Korean J Radiol. 2017 May-Jun;18(3):498-509. PMID: 28458602 | PDF Authors: Lee M, Woo B, Kuo MD, Jamshidi N, Kim JH. Institution: Center for Medical-IT Convergence Technology Research, Advanced Institutes of Convergence Technology, Seoul National University, Suwon, Korea. Background/Purpose: The purpose of this study was to evaluate the reliability and quality of radiomic features in glioblastoma multiforme (GBM) derived from tumor volumes obtained with semi-automated tumor segmentation software. MATERIALS AND METHODS: MR images of 45 GBM patients (29 males, 16 females) were downloaded from The Cancer Imaging Archive, in which post-contrast T1-weighted imaging and fluid-attenuated inversion recovery MR sequences were used. Two raters independently segmented the tumors using two semi-automated segmentation tools (TumorPrism3D and 3D Slicer). Regions of interest corresponding to contrast-enhancing lesion, necrotic portions, and non-enhancing T2 high signal intensity component were segmented for each tumor. A total of 180 imaging features were extracted, and their quality was evaluated in terms of stability, normalized dynamic range (NDR), and redundancy, using intra-class correlation coefficients, cluster consensus, and Rand Statistic. RESULTS: Our study results showed that most of the radiomic features in GBM were highly stable. Over 90% of 180 features showed good stability (intra-class correlation coefficient [ICC] ≥ 0.8), whereas only 7 features were of poor stability (ICC < 0.5). Most first order statistics and morphometric features showed moderate-to-high NDR (4 > NDR ≥1), while above 35% of the texture features showed poor NDR (< 1). Features were shown to cluster into only 5 groups, indicating that they were highly redundant. CONCLUSION: The use of semi-automated software tools provided sufficiently reliable tumor segmentation and feature stability; thus helping to overcome the inherent inter-rater and intra-rater variability of user intervention. However, certain aspects of feature quality, including NDR and redundancy, need to be assessed for determination of representative signature features before further development of radiomics. |
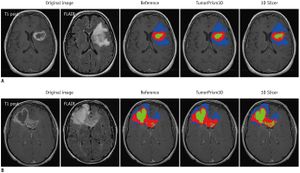 Example of segmentation results with two semi-automated software tools. Contrast-enhanced, necrotic, and non-enhancing T2 high signal intensity components are indicated by red, green, and blue color, respectively. A. Represents case in which similar segmentation results were produced. B. Represents case in which difference was observed in segmentation results. FLAIR = fluid-attenuated inversion recovery. |
Prognostic Implications of the Subcellular Localization of Survivin in Glioblastomas Treated with Radiotherapy Plus Concomitant and Adjuvant Temozolomide
|
Publication: J Neurosurg. 2017 Apr 21:1-6. PMID: 28430038 Authors: Saito T, Sugiyama K, Takeshima Y, Amatya VJ, Yamasaki F, Takayasu T, Nosaka R, Muragaki Y, Kawamata T, Kurisu K. Institution: Department of Neurosurgery, Tokyo Women's Medical University, Tokyo, Japan.. Background/Purpose: OBJECTIVE Currently, the standard treatment protocol for patients with newly diagnosed glioblastoma (GBM) includes surgery, radiotherapy, and concomitant and adjuvant temozolomide (TMZ). Various prognostic biomarkers for GBM have been described, including survivin expression. The aim of this study was to determine whether the subcellular localization of survivin correlates with GBM prognosis in patients who received the standard treatment protocol. METHODS The authors retrospectively examined the subcellular localization of survivin (nuclear, cytoplasmic, or both) using immunohistochemistry in 50 patients with GBM who had received the standard treatment. The relationship between survivin localization and overall survival (OS) was assessed with uni- and multivariate analyses including other clinicopathological factors (age, sex, Karnofsky Performance Scale [KPS] score, extent of resection, the use of second-line bevacizumab, O6-methylguanine-DNA methyltransferase [MGMT] status, and MIB-1 labeling index). RESULTS Log-rank tests revealed that patient age, KPS score, extent of resection, MGMT status, and survivin localization (p < 0.0001) significantly correlated with OS. Multivariate analysis indicated that patient age, MGMT status, and survivin localization significantly correlated with OS. Patients with nuclear localization of survivin had a significantly shorter OS than those in whom survivin expression was exclusively cytoplasmic (median OS 19.5 vs 31.7 months, respectively, HR 5.690, 95% CI 2.068-17.612, p = 0.0006). There was no significant difference in OS between patents whose survivin expression was exclusively nuclear or nuclear/cytoplasmic. CONCLUSIONS Nuclear expression of survivin is a factor for a poor prognosis in GBM patients. Subcellular localization of survivin can help to predict OS in GBM patients treated with the standard protocol. |
An Ovine Model of Cerebral Catheter Venography for Implantation of an Endovascular Neural Interface
|
Publication: J Neurosurg. 2017 Apr 28:1-8. PMID: 28452616 Authors: Oxley TJ, Opie NL, Rind GS, Liyanage K, John SE, Ronayne S, McDonald AJ, Dornom A, Lovell TJH, Mitchell PJ, Bennett I, Bauquier S, Warne LN, Steward C, Grayden DB, Desmond P, Davis SM, O'Brien TJ, May CN. Institution: Vascular Bionics Laboratory, Department of Medicine, The Royal Melbourne Hospital, Melbourne, Australia. Background/Purpose: Neural interface technology may enable the development of novel therapies to treat neurological conditions, including motor prostheses for spinal cord injury. Intracranial neural interfaces currently require a craniotomy to achieve implantation and may result in chronic tissue inflammation. Novel approaches are required that achieve less invasive implantation methods while maintaining high spatial resolution. An endovascular stent electrode array avoids direct brain trauma and is able to record electrocorticography in local cortical tissue from within the venous vasculature. The motor area in sheep runs in a parasagittal plane immediately adjacent to the superior sagittal sinus (SSS). The authors aimed to develop a sheep model of cerebral venography that would enable validation of an endovascular neural interface. METHODS Cerebral catheter venography was performed in 39 consecutive sheep. Contrast-enhanced MRI of the brain was performed on 13 animals. Multiple telescoping coaxial catheter systems were assessed to determine the largest wide-bore delivery catheter that could be delivered into the anterior SSS. Measurements of SSS diameter and distance from the motor area were taken. The location of the motor area was determined in relation to lateral and superior projections of digital subtraction venography images and confirmed on MRI. RESULTS The venous pathway from the common jugular vein (7.4 mm) to the anterior SSS (1.2 mm) was technically challenging to selectively catheterize. The SSS coursed immediately adjacent to the motor cortex (< 1 mm) for a length of 40 mm, or the anterior half of the SSS. Attempted access with 5-Fr and 6-Fr delivery catheters was associated with longer procedure times and higher complication rates. A 4-Fr catheter (internal lumen diameter 1.1 mm) was successful in accessing the SSS in 100% of cases with no associated complications. Complications included procedure-related venous dissection in two major areas: the torcular herophili, and the anterior formation of the SSS. The bifurcation of the cruciate sulcal veins with the SSS was a reliable predictor of the commencement of the motor area. CONCLUSIONS The ovine model for cerebral catheter venography has generalizability to the human cerebral venous system in relation to motor cortex location. This novel model may facilitate the development of the novel field of endovascular neural interfaces that may include preclinical investigations for cortical recording applications such as paralysis and epilepsy, as well as other potential applications in neuromodulation. |
Effectiveness of Endoscopic Surgery for Supratentorial Hypertensive Intracerebral Hemorrhage: A Comparison with Craniotomy
|
Publication: J Neurosurg. 2017 Apr 7:1-7. PMID: 28387618 Authors: Xu X, Chen X, Li F, Zheng X, Wang Q, Sun G, Zhang J, Xu B. Institution: Department of Neurosurgery, Chinese PLA General Hospital, Beijing, China. Background/Purpose: OBJECTIVE The goal of this study was to investigate the effectiveness and practicality of endoscopic surgery for treatment of supratentorial hypertensive intracerebral hemorrhage (HICH) compared with traditional craniotomy. METHODS The authors retrospectively analyzed 151 consecutive patients who were operated on for treatment of supratentorial HICH between January 2009 and June 2014 in the Department of Neurosurgery at Chinese PLA General Hospital. Patients were separated into an endoscopy group (82 cases) and a craniotomy group (69 cases), depending on the surgery they received. The hematoma evacuation rate was calculated using 3D Slicer software to measure the hematoma volume. Comparisons of operative time, intraoperative blood loss, Glasgow Coma Scale score 1 week after surgery, hospitalization time, and modified Rankin Scale score 6 months after surgery were also made between these groups. RESULTS There was no statistically significant difference in preoperative data between the endoscopy group and the craniotomy group (p > 0.05). The hematoma evacuation rate was 90.5% ± 6.5% in the endoscopy group and 82.3% ± 8.6% in the craniotomy group, which was statistically significant (p < 0.01). The operative time was 1.6 ± 0.7 hours in the endoscopy group and 5.2 ± 1.8 hours in the craniotomy group (p < 0.01). The intraoperative blood loss was 91.4 ± 93.1 ml in the endoscopy group and 605.6 ± 602.3 ml in the craniotomy group (p < 0.01). The 1-week postoperative Glasgow Coma Scale score was 11.5 ± 2.9 in the endoscopy group and 8.3 ± 3.8 in the craniotomy group (p < 0.01). The hospital stay was 11.6 ± 6.9 days in the endoscopy group and 13.2 ± 7.9 days in the craniotomy group (p < 0.05). The mean modified Rankin Scale score 6 months after surgery was 3.2 ± 1.5 in the endoscopy group and 4.1 ± 1.9 in the craniotomy group (p < 0.01). Patients had better recovery in the endoscopy group than in the craniotomy group. Data are expressed as the mean ± SD. CONCLUSIONS Compared with traditional craniotomy, endoscopic surgery was more effective, less invasive, and may have improved the prognoses of patients with supratentorial HICH. Endoscopic surgery is a promising method for treatment of supratentorial HICH. With the development of endoscope technology, endoscopic evacuation will become more widely used in the clinic. Prospective randomized controlled trials are needed. |
Quantitative CT ventriculography for Assessment and Monitoring of Hydrocephalus: a Pilot Study and Description of Method in Subarachnoid Hemorrhage (SAH)
|
Publication: World Neurosurg. 2017 Apr 26. PMID: 28456742 Authors: Multani JS, Oermann EK, Titano J, Mascitelli J, Nicol K, Feng R, Skovrlj B, Pain M, Mocco JD, Bederson JB, Costa A, Shrivastava R. Institution: Department of Neurological Surgery, Mount Sinai Health System, New York, NY, USA. Background/Purpose: There is no facile quantitative method for monitoring hydrocephalus (HCP). OBJECTIVE: We propose quantitative CT ventriculography (qCTV) as a novel computer vision tool for empirically assessing HCP in patients with subarachnoid hemorrhage (SAH). METHODS: Twenty patients with SAH who were evaluated for ventriculoperitoneal shunt (VPS) placement were selected for inclusion. Ten patients with normal CT head (CTH) were analyzed as negative controls. CTH scans were segmented both manually and automatically (qCTV) to generate measures of ventricular volume. RESULTS: Median manually calculated ventricular volume was 36.1cm3 (IQR 30-115cm3), which was similar to a median qCTV measured volume of 37.5cm3 (IQR 32-118cm3) (p=0.796). Patients undergoing VPS placement demonstrated an increase in ventricular volume on qCTV from 21cm3 to 40cm3 on Day T-2, and 51cm3 by Day 0, a change of 144%. This contrasts with patients who did not require shunting whose ventricular volumes decreased from 16cm3 to 14cm3 on Day T-2, and 13cm3 by Day 0, with an average overall decrease in volume of 19% (p=0.001). Average change in ventricular volume predicted which patients would require VPS placement, successfully identifying 7/10 patients (p=0.004). Using an optimized cutoff of change in ventricular volume of 2.5cm3 identified all patients who went on to require VPS placement (10/10, p=0.011). CONCLUSIONS: qCTV is a reliable means of quantifying ventricular volume and hydrocephalus. This technique offers a new tool for monitoring neurosurgical patients for hydrocephalus, and may be beneficial for use in future research studies as well as the routine care of patients with hydrocephalus. |
Infantile Cranial Fasciitis: Case-based Review and Operative Technique
|
Publication: Childs Nerv Syst. 2017 Apr 27. PMID: 28451777 Authors: Flouty OE, Piscopo AJ, Holland MT, Abode-Iyamah K, Bruch L, Menezes AH, Dlouhy BJ.
Background/Purpose: Cranial fasciitis (CF) is an uncommon benign primary lesion of the skull that typically affects the pediatric age group. Due to the rarity of CF, no prospective studies exist. Earliest description of this condition dates to 1980. The limited scientific and clinical literature regarding CF is dominated by case reports. For these reasons, questions pertaining to the true incidence, genetic risk factors, prognosis, and long-term outcome remain unanswered. DISCUSSION: Clinically, CF presents as a firm, painless, growing scalp mass that is typically not considered in the differential diagnosis. Preoperative pathognomonic signs and symptoms are absent, and imaging features are often nonspecific. Treatment is typically through complete surgical resection, at which time histopathological examination confirms the diagnosis of CF. Reconstruction of the skull defect in the child is critical. Autograft techniques help maintain a rigid construct that integrates with the native skull while preserving its continued ability to grow. Generally, a good outcome is observed with complete resection. EXEMPLARY CASE: We report a case of CF in an infant with emphasis on operative nuances and early follow-up results. CONCLUSION: CF is a rare fibroproliferative disease that has a poorly defined incidence and long-term follow-up. Due to its locally invasive nature and nonspecific presentation, CF is often difficult to differentiate from malignancies and infections. Complete surgical resection is the best approach for diagnosis and cure. Its occult clinical presentation often allows it to achieve considerable growth, leaving a sizeable skull defect following resection. Since CF presents in the pediatric population, allograft reconstruction is preferred over titanium mesh or other synthetic materials to allow osseous integration and continued uninterrupted skull growth. |
The Effects of Iterative Reconstruction and Kernel Selection on Quantitative Computed Tomography Measures of Lung Density
|
Publication: Med Phys. 2017 Apr 4. PMID: 28376262 Authors: Rodriguez A, Ranallo FN, Judy PF, Fain SB. Institution: Department of Medical Physics, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA. Background/Purpose: To determine the effects of iterative reconstruction (IR) and high frequency kernels on quantitative computed tomography (qCT) density measures at reduced X-ray dose. MATERIALS AND METHODS: The COPDGene 2 Phantom (CTP 698, The Phantom Laboratory, Salem, NY) with four embedded lung mimicking foam densities (12lb, 20lb, and 4lb), as well as water, air, and acrylic reference inserts was imaged using a GE 64 slice CT750 HD scanner in helical mode with four current-time products ranging from 12-100 mAs. The raw acquired data was reconstructed using standard (STD - low frequency) and Bone (high frequency) kernels with filtered back projection (FBP), 100% ASIR, and Veo reconstruction algorithms. The reference density inserts were manually segmented using 3D Slicer and the mean, standard deviation, and histograms of the segmented regions were generated using Fiji (http://fiji.sc/Fiji) for each reconstruction. Measurements of threshold values placed on the cumulative frequency distribution of voxels determined by these measured histograms at 5%, PD5phant , and 15%, PD15phant , (analogous to the relative area below -950 HU (RA950) and percent density 15 (PD15) in human lung emphysema quantification, respectively), were also performed. RESULTS: The use of high-resolution kernels in conjunction with ASIR, and Veo did not significantly affect the mean Hounsfield units (HU) of each of the density standards (<4 HU deviation) and current-time products within the phantom when compared with the STD+FBP reconstruction conventionally used in clinical applications. A truncation of the scanner reported HU values at -1024 that shifts the mean towards more positive values was found to cause a systematic error in lower attenuating regions. Use of IR drove convergence toward the mean of measured histograms (~100-137% increase in the number measured voxels at the mean of the histogram) while the combination of Bone+ASIR preserved the standard deviation of HU values about the mean compared to STD+FBP, with the added effect of improved spatial resolution and accuracy in airway measures. PD5phant and PD15phant were most similar between the Bone+ASIR and STD+FBP in all regions except those affected by the -1024 truncation artifact. CONCLUSIONS: Extension of the scanner reportable HU values below the present limit of -1024 will mitigate discrepancies found in qCT lung densitometry in low-density regions. The density histogram became more sharply peaked and standard deviation was reduced for IR, directly effecting density thresholds, PD5phant and PD15phant, placed on the cumulative frequency distribution of each region in the phantom, which serve as analogs to RA950 and PD15 typically used in lung density quantitation. The combination of high frequency kernels (Bone) with ASIR mitigates this effect and preserves density measures derived from the image histogram. Moreover, previous studies have shown improved accuracy of qCT airway measures of wall thickness (WT) and wall area percentage (WA%) when using high frequency kernels in combination with ASIR to better represent airway walls. The results therefore suggest an IR approach for accurate assessment of airway and parenchymal density measures in the lungs. |
Asymmetry in Dentition and Shape of Pharyngeal Arches in the Clonal Fish Chrosomus Eos-neogaeus: Phenotypic Plasticity and Developmental Instability
|
Publication: PLoS One. 2017 Apr 5;12(4):e0174235. PMID: 28380079 | PDF Authors: Leung C, Duclos KK, Grünbaum T, Cloutier R, Angers B. Institution: Department of Biological Sciences, Université de Montréal, Montreal, Quebec, Canada. Background/Purpose: The effect of the environment may result in different developmental outcomes. Extrinsic signals can modify developmental pathways and result in alternative phenotypes (phenotypic plasticity). The environment can also be interpreted as a stressor and increase developmental instability (developmental noise). Directional and fluctuating asymmetry provide a conceptual background to discriminate between these results. This study aims at assessing whether variation in dentition and shape of pharyngeal arches of the clonal fish Chrosomus eos-neogaeus results from developmental instability or environmentally induced changes. A total of 262 specimens of the Chrosomus eos-neogaeus complex from 12 natural sites were analysed. X-ray microcomputed tomography (X-ray micro-CT) was used to visualize the pharyngeal arches in situ with high resolution. Variation in the number of pharyngeal teeth is high in hybrids in contrast to the relative stability observed in both parental species. The basal dental formula is symmetric while the most frequent alternative dental formula is asymmetric. Within one lineage, large variation in the proportion of individuals bearing basal or alternative dental formulae was observed among sites in the absence of genetic difference. Both dentition and arch shape of this hybrid lineage were explained significantly by environmental differences. Only individuals bearing asymmetric dental formula displayed fluctuating asymmetry as well as directional left-right asymmetry for the arches. The hybrids appeared sensitive to environmental signals and intraspecific variation on pharyngeal teeth was not random but reflects phenotypic plasticity. Altogether, these results support the influence of the environment as a trigger for an alternative developmental pathway resulting in left-right asymmetry in dentition and shape of pharyngeal arches. Dicom files were subsequently loaded within the open-source software 3D Slicer (Version 4.5 ). 3D models were rendered from dicom files using the editor module within 3D Slicer and the thresholding algorithm. |
Scanning Laser Optical Tomography for in Toto Imaging of the Murine Cochlea.
|
Publication: PLoS One. 2017 Apr 7;12(4):e0175431. PMID: 28388662 | PDF Authors: Nolte L, Tinne N, Schulze J, Heinemann D, Antonopoulos GC, Meyer H, Nothwang HG, Lenarz T, Heisterkamp A, Warnecke A, Ripken T. Institution: Industrial and Biomedical Optics Department, Laser Zentrum Hannover e.V., Hannover, Germany. Background/Purpose: The mammalian cochlea is a complex macroscopic structure due to its helical shape and the microscopic arrangements of the individual layers of cells. To improve the outcomes of hearing restoration in deaf patients, it is important to understand the anatomic structure and composition of the cochlea ex vivo. Hitherto, only one histological technique based on confocal laser scanning microscopy and optical clearing has been developed for in toto optical imaging of the murine cochlea. However, with a growing size of the specimen, e.g., human cochlea, this technique reaches its limitations. Here, we demonstrate scanning laser optical tomography (SLOT) as a valuable imaging technique to visualize the murine cochlea in toto without any physical slicing. This technique can also be applied in larger specimens up to cm3 such as the human cochlea. Furthermore, immunolabeling allows visualization of inner hair cells (otoferlin) or spiral ganglion cells (neurofilament) within the whole cochlea. After image reconstruction, the 3D dataset was used for digital segmentation of the labeled region. As a result, quantitative analysis of position, length and curvature of the labeled region was possible. This is of high interest in order to understand the interaction of cochlear implants (CI) and cells in more detail. To enable correct overlay of the two excitation channels, the general registration algorithm (BRAINS) from the open source software 3D Slicer was used. |
 Maximum intensity projections (MIP) were performed on the reconstructed data of samples 1 and 2. (A) MIP of sample 1. The labeled neurofilament appears as a helical shape inside the cochlea. (B) Higher magnification of the highlighted area in A. The dendrites of the spiral ganglions are visible. (C) Negative control (sample 2). Only autofluorescence and nonspecific binding shows the outer shape of the cochlea. (D) Higher magnification of the highlighted area in C. |
Patient Education for Endoscopic Sinus Surgery: Preliminary Experience Using 3D-Printed Clinical Imaging Data
|
Publication: J Funct Biomater. 2017 Apr 7;8(2). PMID: 28387702 | PDF Authors: Sander IM, Liepert TT, Doney EL, Leevy WM, Liepert DR. Institution: Department of Biological Sciences, University of Notre Dame, South Bend, IN, USA. Background/Purpose: Within the Ear, Nose, and Throat (ENT) medical space, a relatively small fraction of patients follow through with elective surgeries to fix ailments such as a deviated septum or occluded sinus passage. Patient understanding of their diagnosis and treatment plan is integral to compliance, which ultimately yields improved medical outcomes and better quality of life. Here we report the usage of advanced, polyjet 3D printing methods to develop a multimaterial replica of human nasal sinus anatomy, derived from clinical X-ray computed tomography (CT) data, to be used as an educational aid during physician consultation. The final patient education model was developed over several iterations to optimize material properties, anatomical accuracy and overall display. A two-arm, single-center, randomized, prospective study was then performed in which 50 ENT surgical candidates (and an associated control group, n = 50) were given an explanation of their anatomy, disease state, and treatment options using the education model as an aid. Statistically significant improvements in patient ratings of their physician's explanation of their treatment options (p = 0.020), self-rated anatomical understanding (p = 0.043), self-rated understanding of disease state (p = 0.016), and effectiveness of the visualization (p = 0.007) were noted from the population that viewed the 3D education model, indicating it is an effective tool which ENT surgeons may use to educate and interact with patients. All volumes outside of the volume of interest were masked at a value of −1000 Hounsfield Units (HU). The data was exported in Nifti (.nii) format and opened in 3D Slicer. A 3D surface map for bone was generated using the “Grayscale Modelmaker” tool within 3D Slicer at a threshold of 300 HU. A separate 3D surface map was generated for soft tissue using the same tool and process with a threshold level of −300 HU. Each surface map was exported from 3DSlicer as a .stl file. |
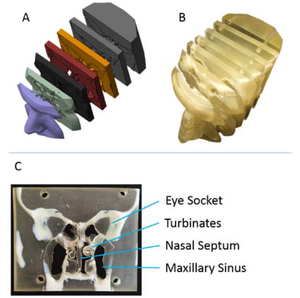 Nasal cavity model generation and fabrication. (A) 3D surface maps generated from CT scan slices of patient nasal cavity used to generate a 3D-printed model; (B) 3D-printed, sliced model, printed with two distinct polymers to represent hard and soft tissues; (C) Single coronal model slice with specific anatomical details highlighted. |
Comprehensive Evaluation of Ten Deformable Image Registration Algorithms for Contour Propagation between CT and Cone-beam CT Images in Adaptive Head & Neck Radiotherapy
|
Publication: PLoS One. 2017 Apr 17;12(4):e0175906. PMID: 28414799 | PDF Authors: Li X, Zhang Y, Shi Y, Wu S, Xiao Y, Gu X, Zhen X, Zhou L. Institution: Department of Biomedical Engineering, Southern Medical University, Guangzhou, Guangdong, China. Background/Purpose:Deformable image registration (DIR) is a critical technic in adaptive radiotherapy (ART) for propagating contours between planning computerized tomography (CT) images and treatment CT/cone-beam CT (CBCT) images to account for organ deformation for treatment re-planning. To validate the ability and accuracy of DIR algorithms in organ at risk (OAR) contour mapping, ten intensity-based DIR strategies, which were classified into four categories-optical flow-based, demons-based, level-set-based and spline-based-were tested on planning CT and fractional CBCT images acquired from twenty-one head & neck (H&N) cancer patients who underwent 6~7-week intensity-modulated radiation therapy (IMRT). Three similarity metrics, i.e., the Dice similarity coefficient (DSC), the percentage error (PE) and the Hausdorff distance (HD), were employed to measure the agreement between the propagated contours and the physician-delineated ground truths of four OARs, including the vertebra (VTB), the vertebral foramen (VF), the parotid gland (PG) and the submandibular gland (SMG). It was found that the evaluated DIRs in this work did not necessarily outperform rigid registration. DIR performed better for bony structures than soft-tissue organs, and the DIR performance tended to vary for different ROIs with different degrees of deformation as the treatment proceeded. Generally, the optical flow-based DIR performed best, while the demons-based DIR usually ranked last except for a modified demons-based DISC used for CT-CBCT DIR. These experimental results suggest that the choice of a specific DIR algorithm depends on the image modality, anatomic site, magnitude of deformation and application. Therefore, careful examinations and modifications are required before accepting the auto-propagated contours, especially for automatic re-planning ART systems. Before performing the rigid and deformable registration, all the images were pre-processed using an open source software 3D Slicer. |
A New Approach for Radiosynoviorthesis: A Dose-Optimized Planning method Based on Monte Carlo Simulation and Synovial Measurement Using 3D Slicer and MRI
|
Publication: Med Phys. 2017 Apr 17. PMID: 28419533 Authors: Torres Berdeguez MB, Thomas S, Rafful P, Arruda Sanchez T, Medeiros Oliveira Ramos S, Albernaz MS, Vasconcellos de Sá L, Lopes de Souza SA, Mas Milian F, Xavier da Silva A. Institution: Nuclear Engineering Department of Federal University of Rio de Janeiro, Rio de Janeiro, Brazil. Background/Purpose: Recently, there has been a growing interest in a methodology for dose planning in radiosynoviorthesis to substitute fixed activity. Clinical practice based on fixed activity frequently does not embrace radiopharmaceutical dose optimization in patients. The aim of this paper is to propose and discuss a dose planning methodology considering the radiological findings of interest obtained by three-dimensional magnetic resonance imaging combined with Monte Carlo simulation in radiosynoviorthesis treatment applied to hemophilic arthropathy. METHOD: The parameters analyzed were: surface area of the synovial membrane (synovial size), synovial thickness and joint effusion obtained by 3D MRI of nine knees from nine patients on a SIEMENS AVANTO 1.5 T scanner using a knee coil. The 3D Slicer software performed both the semiautomatic segmentation and quantification of these radiological findings. A Lucite phantom 3D MRI validated the quantification methodology. The study used Monte Carlo N-Particle eXtended code version 2.6 for calculating the S-values required to set up the injected activity to deliver a 100 Gy absorbed dose at a determined synovial thickness. The radionuclides assessed were: 90Y, 32P, 188Re, 186Re, 153Sm, and 177Lu, and the present study shows their effective treatment ranges. RESULT: The quantification methodology was successfully tested, with an error below 5% for different materials. S-values calculated could provide data on the activity to be injected into the joint, considering no extra-articular leakage from joint cavity. Calculation of effective treatment range could assist with the therapeutic decision, with an optimized protocol for dose prescription in RSO. CONCLUSION: Using 3D Slicer software, this study focused on segmentation and quantification of radiological features such as joint effusion, synovial size and thickness, all obtained by 3D MRI in patients knees with hemophilic arthropathy. The combination of synovial size and thickness with the parameters obtained by Monte Carlo simulation such as effective treatment range and S-value, from which is calculated the injected activity, could be used for treatment planning in RSO. Data from this methodology could be a potential aid to clinical decision making by selecting the most suitable radionuclide; justifying the procedure, fractioning the dose and the calculated injected activity for children and adolescents, considering both the synovial size and thickness. |
Exercise Decreases Marrow Adipose Tissue Through ß-Oxidation in Obese Running Mice
|
Publication: J Bone Miner Res. 2017 Apr 24. PMID: 28436105 Authors: Styner M, Pagnotti GM, McGrath C, Wu X, Sen B, Uzer G, Xie Z, Zong X, Styner MA, Rubin CT, Rubin J. Institution: Department of Medicine, Division of Endocrinology and Metabolism, University of North Carolina, Chapel Hill, NC, USA. Background/Purpose: The relationship between marrow adipose tissue (MAT) and bone health is poorly understood. We used running exercise to ask whether obesity-associated MAT can be attenuated via exercise and whether this correlates with gains in bone quantity and quality. C57BL/6 mice were divided into diet-induced obesity (DIO, n = 14) versus low-fat diet (LFD, n = 14). After 3 months, 16-week-old mice were allocated to an exercise intervention (LFD-E, DIO-E) or a control group (LFD, DIO) for 6 weeks (4 groups, n = 7/group). Marrow adipocyte area was 44% higher with obesity (p < 0.0001) and after exercise 33% lower in LFD (p < 0.0001) and 39% lower in DIO (p < 0.0001). In LFD, exercise did not affect adipocyte number; however, in DIO, the adipocyte number was 56% lower (p < 0.0001). MAT was 44% higher in DIO measured by osmium-μCT, whereas exercise associated with reduced MAT (-23% in LFD, -48% in DIO, p < 0.05). MAT was additionally quantified by 9.4TMRI, and correlated with osmium-µCT (r = 0.645; p < 0.01). Consistent with higher lipid beta oxidation, perilipin 3 (PLIN3) rose with exercise in tibial mRNA (+92% in LFD, +60% in DIO, p < 0.05). Tibial µCT-derived trabecular bone volume (BV/TV) was not influenced by DIO but responded to exercise with an increase of 19% (p < 0.001). DIO was associated with higher cortical periosteal and endosteal volumes of 15% (p = 0.012) and 35% (p < 0.01), respectively, but Ct.Ar/Tt.Ar was lower by 2.4% (p < 0.05). There was a trend for higher stiffness (N/m) in DIO, and exercise augmented this further. In conclusion, obesity associated with increases in marrow lipid-measured by osmium-μCT and MRI-and partially due to an increase in adipocyte size, suggesting increased lipid uptake into preexisting adipocytes. Exercise associated with smaller adipocytes and less bone lipid, likely invoking increased ß-oxidation and basal lipolysis as evidenced by higher levels of PLIN3. © 2017 American Society for Bone and Mineral Research. |
Interactive Outlining of Pancreatic Cancer Liver Metastases in Ultrasound Images
|
Publication: Sci Rep. 2017 Apr 18;7(1):892. PMID: 28420871 Authors: Egger J, Schmalstieg D, Chen X, Zoller WG, Hann A. Institution: Institute for Computer Graphics and Vision, Graz University of Technology, Graz, Austria. Background/Purpose: Ultrasound (US) is the most commonly used liver imaging modality worldwide. Due to its low cost, it is increasingly used in the follow-up of cancer patients with metastases localized in the liver. In this contribution, we present the results of an interactive segmentation approach for liver metastases in US acquisitions. A (semi-) automatic segmentation is still very challenging because of the low image quality and the low contrast between the metastasis and the surrounding liver tissue. Thus, the state of the art in clinical practice is still manual measurement and outlining of the metastases in the US images. We tackle the problem by providing an interactive segmentation approach providing real-time feedback of the segmentation results. The approach has been evaluated with typical US acquisitions from the clinical routine, and the datasets consisted of pancreatic cancer metastases. Even for difficult cases, satisfying segmentations results could be achieved because of the interactive real-time behavior of the approach. In total, 40 clinical images have been evaluated with our method by comparing the results against manual ground truth segmentations. This evaluation yielded to an average Dice Score of 85% and an average Hausdorff Distance of 13 pixels. We tested our data with the GrowCut implementation that is available in 3D Slicer. |
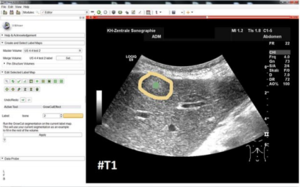 GrowCut segmentation results for the two metastases from Fig. 9. The left images show the manual initialization of GrowCut: the metastases were initialized with green, and the backgrounds were initialized with yellow. The images in the middle show the segmentation results of GrowCut (green). The right images show a closer view of the segmentation results (green) with a lower opacity. |
The evolution of Cost-efficiency in Neural Networks during Recovery from Traumatic Brain Injury
|
Publication: PLoS One. 2017 Apr 19;12(4):e0170541. PMID: 28422992 | PDF Authors: Roy A, Bernier RA, Wang J, Benson M, French JJ Jr, Good DC, Hillary FG. Institution: Department of Psychology, The Pennsylvania State University, University Park, Pennsylvania, USA. Background/Purpose: A somewhat perplexing finding in the systems neuroscience has been the observation that physical injury to neural systems may result in enhanced functional connectivity (i.e., hyperconnectivity) relative to the typical network response. The consequences of local or global enhancement of functional connectivity remain uncertain and this is particularly true for the overall metabolic cost of the network. We examine the hyperconnectivity hypothesis in a sample of 14 individuals with TBI with data collected at approximately 3, 6, and 12 months following moderate and severe TBI. As anticipated, individuals with TBI showed increased network strength and cost early after injury, but by one-year post injury hyperconnectivity was more circumscribed to frontal DMN and temporal-parietal attentional control regions. Cost in these subregions was a significant predictor of cognitive performance. Cost-efficiency analysis in the Power 264 data parcellation suggested that at 6 months post injury the network requires higher cost connections to achieve high efficiency as compared to the network 12 months post injury. These results demonstrate that networks self-organize to re-establish connectivity while balancing cost-efficiency trade-offs. To determine the influence of global pathology on brain networks, we created a 3-dimensional (3D) lesion model for each subject using 3D Slicer that utilizes information from multiple MR sequences, such as SWI, FLAIR, and T1 MPRAGE. |
Three‐Dimensional Printing: An Aid to Epidural Access for Neuromodulation
|
Publication: Neuromodulation. 2017 Apr 20 PMID: 28425137 Authors: Taverner MG, Monagle JP. Institution: Frankston Pain Management, Victoria, Australia. Background/Purpose: OBJECTIVE: The case report details to use of three-dimensional (3D) printing as an aid to neuromodulation. METHODS: A patient is described in whom previous attempts at spinal neuromodulation had failed due to lack of epidural or intrathecal access, and the use of a 3D printed model allowed for improved planning and ultimately, success. Thin-slices (0.625 mm) of a high-resolution CT scan of the patient's thoracolumbar spine and iliac crests was used to create a CAD model on 3D Slicer software (Surgical Planning Laboratory, Boston, MA RESULTS: Successful spinal cord stimulation was achieved with the plan developed by access to a 3D model of the patient's spine. CONCLUSION: Neuromodulation techniques can provide the optimal analgesic techniques for individual patients. At times these can fail due to lack of access to the site for intervention, in this case epidural access. 3D printing may provide additional information to improve the likelihood of access when anatomy is distorted and standard approaches prove difficult. |
Biomechanical Flow Amplification Arising From the Variable Deformation of the Subglottic Mucosa
|
Publication: J Voice. 2017 Apr 19. PMID: 28433346 | PDF Authors: Goodyer E, Müller F, Hess M, Kandan K, Farukh F. Institution: De Montfort University, Bio-Informatics Research Group, Leicester, UK. Background/Purpose: OBJECTIVE: This study mapped the variation in tissue elasticity of the subglottic mucosa, applied these data to provide initial models of the likely deformation of the mucosa during the myoelastic cycle, and hypothesized as to the impact on the process of phonation. STUDY DESIGN: Six donor human larynges were dissected along the sagittal plane to expose the vocal folds and subglottic mucosa. A linear skin rheometer was used to apply a controlled shear force, and the resultant displacement was measured. These data provided a measure of the stress/strain characteristics of the tissue at each anatomic point. A series of measurements were taken at 2-mm interval inferior of the vocal folds, and the change in elasticity was determined. CT images of the excised larynges have been used to create 3D reconstructions with the help of an open-source medical imaging software, 3D Slicer. RESULTS: It was found that the elasticity of the mucosa in the subglottic region increased linearly with distance from the vocal folds in all 12 samples. A simple deformation model indicated that under low pressure conditions the subglottic mucosa will deform to form a cone, which could result in a higher velocity, thus amplifying the low pressure effect resulting from the Venturi principle, and could assist in maintaining laminar flow. CONCLUSIONS: This study indicated that the deformation of the subglottic mucosa could play a significant role in the delivery of a low pressure airflow over the vocal folds. A large scale study will now be undertaken to secure more data to evaluate this hypothesis, and using computational fluid dynamics based on actual three-dimensional structure obtained from computed tomography scans the aerodynamics of this region will be investigated. |
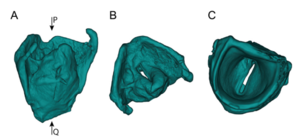 Three-dimensional (3D) model of a larynx constructed from a computed tomography scan images (A) showing the full 3D model. (B) and (C) Show the views of larynx looking down the arrow as indicated by the letter P and Q, respectively. CT images of the excised larynges have been used to create 3D reconstructions with the help of an open-source medical imaging software, 3D Slicer. |
HTC Vive MeVisLab Integration via OpenVR for Medical Applications
|
Publication: PLoS One. 2017 Mar 21;12(3):e0173972. PMID: 28323840 | PDF Authors: Egger J, Gall M, Wallner J, Boechat P, Hann A, Li X, Chen X, Schmalstieg D. Institution: Institute of Computer Graphics and Vision, Graz University of Technology, Graz, Austria. Background/Purpose:Virtual Reality, an immersive technology that replicates an environment via computer-simulated reality, gets a lot of attention in the entertainment industry. However, VR has also great potential in other areas, like the medical domain, Examples are intervention planning, training and simulation. This is especially of use in medical operations, where an aesthetic outcome is important, like for facial surgeries. Alas, importing medical data into Virtual Reality devices is not necessarily trivial, in particular, when a direct connection to a proprietary application is desired. Moreover, most researcher do not build their medical applications from scratch, but rather leverage platforms like MeVisLab, MITK, OsiriX or 3D Slicer. These platforms have in common that they use libraries like ITK and VTK, and provide a convenient graphical interface. However, ITK and VTK do not support Virtual Reality directly. In this study, the usage of a Virtual Reality device for medical data under the MeVisLab platform is presented. The OpenVR library is integrated into the MeVisLab platform, allowing a direct and uncomplicated usage of the head mounted display HTC Vive inside the MeVisLab platform. Medical data coming from other MeVisLab modules can directly be connected per drag-and-drop to the Virtual Reality module, rendering the data inside the HTC Vive for immersive virtual reality inspection. |
What are the True Volumes of SEGA Tumors? Reliability of Planimetric and Popular Semi-automated Image Segmentation Methods
|
Publication: MAGMA. 2017 Mar 20. PMID: 28321524 Authors: Stawiski K, Trelińska J, Baranska D, Dachowska I, Kotulska K, Jóźwiak S, Fendler W, Młynarski W. Institution: Department of Biostatistics and Translational Medicine, Hematology and Diabetology, Medical University of Lodz, Lodz, Poland. Background/Purpose: OBJECTIVE: To evaluate the reliability of the standard planimetric methodology of volumetric analysis and three different open-source semi-automated approaches of brain tumor segmentation. MATERIALS AND METHODS: The volumes of subependymal giant cell astrocytomas (SEGA) examined by 30 MRI studies of 10 patients from a previous everolimus-related trial (EMINENTS study) were estimated using four methods: planimetric method (modified MacDonald ellipsoid method), ITK-Snap (pixel clustering, geodesic active contours, region competition methods), 3D Slicer (level-set thresholding), and NIRFast (k-means clustering, Markov random fields). The methods were compared, and a trial simulation was performed to determine how the choice of approach could influence the final decision about progression or response. RESULTS: Intraclass correlation coefficient was high (0.95; 95% CI 0.91-0.98). The planimetric method always overestimated the size of the tumor, while virtually no mean difference was found between ITK-Snap and 3D Slicer (P = 0.99). NIRFast underestimated the volume and presented a proportional bias. During the trial simulation, a moderate level of agreement between all the methods (kappa 0.57-0.71, P < 0.002) was noted. CONCLUSION: Semi-automated segmentation can ease oncological follow-up but the moderate level of agreement between segmentation methods suggests that the reference standard volumetric method for SEGA tumors should be revised and chosen carefully, as the selection of volumetry tool may influence the conclusion about tumor progression or response. |
Anser EMT: The First Open-Source Electromagnetic Tracking Platform for Image-Guided Interventions
|
Publication: Int J Comput Assist Radiol Surg. 2017 Mar 29. PMID: 28357627 Authors: Jaeger HA, Franz AM, O'Donoghue K, Seitel A, Trauzettel F, Maier-Hein L, Cantillon-Murphy P. Institution: IHU Strasbourg, Strasbourg, France. Background/Purpose: PURPOSE: Electromagnetic tracking is the gold standard for instrument tracking and navigation in the clinical setting without line of sight. Whilst clinical platforms exist for interventional bronchoscopy and neurosurgical navigation, the limited flexibility and high costs of electromagnetic tracking (EMT) systems for research investigations mitigate against a better understanding of the technology's characterisation and limitations. The Anser project provides an open-source implementation for EMT with particular application to image-guided interventions. METHODS: This work provides implementation schematics for our previously reported EMT system which relies on low-cost acquisition and demodulation techniques using both National Instruments and Arduino hardware alongside MATLAB support code. The system performance is objectively compared to other commercial tracking platforms using the Hummel assessment protocol. RESULTS: Positional accuracy of 1.14 mm and angular rotation accuracy of [Formula: see text] are reported. Like other EMT platforms, Anser is susceptible to tracking errors due to eddy current and ferromagnetic distortion. The system is compatible with commercially available EMT sensors as well as the Open Network Interface for image-guided therapy (OpenIGTLink) for easy communication with visualisation and medical imaging toolkits such as MITK and 3D Slicer. CONCLUSIONS: By providing an open-source platform for research investigations, we believe that novel and collaborative approaches can overcome the limitations of current EMT technology. |
SLIDE: Automatic Spine Level Identification System using a Deep Convolutional Neural Network
|
Publication: Int J Comput Assist Radiol Surg. 2017 Mar 30. PMID: 28361323 Authors: Hetherington J, Lessoway V, Gunka V, Abolmaesumi P, Rohling R. Institution: Department of Electrical and Computer Engineering, The University of British Columbia, Vancouver, Canada. Background/Purpose: PURPOSE: Percutaneous spinal needle insertion procedures often require proper identification of the vertebral level to effectively and safely deliver analgesic agents. The current clinical method involves "blind" identification of the vertebral level through manual palpation of the spine, which has only 30% reported accuracy. Therefore, there is a need for better anatomical identification prior to needle insertion. METHODS: A real-time system was developed to identify the vertebral level from a sequence of ultrasound images, following a clinical imaging protocol. The system uses a deep convolutional neural network (CNN) to classify transverse images of the lower spine. Several existing CNN architectures were implemented, utilizing transfer learning, and compared for adequacy in a real-time system. In the system, the CNN output is processed, using a novel state machine, to automatically identify vertebral levels as the transducer moves up the spine. Additionally, a graphical display was developed and integrated within 3D Slicer. Finally, an augmented reality display, projecting the level onto the patient's back, was also designed. A small feasibility study [Formula: see text] evaluated performance. RESULTS: The proposed CNN successfully discriminates ultrasound images of the sacrum, intervertebral gaps, and vertebral bones, achieving 88% 20-fold cross-validation accuracy. Seventeen of 20 test ultrasound scans had successful identification of all vertebral levels, processed at real-time speed (40 frames/s). CONCLUSION: A machine learning system is presented that successfully identifies lumbar vertebral levels. The small study on human subjects demonstrated real-time performance. A projection-based augmented reality display was used to show the vertebral level directly on the subject adjacent to the puncture site. |
Revealing Cancer Subtypes with Higher-Order Correlations Applied to Imaging and Omics Data
|
Publication: BMC Med Genomics. 2017 Mar 31;10(1):20. PMID: 28359308 | PDF Authors: Graim K, Liu TT, Achrol AS, Paull EO, Newton Y, Chang SD, Harsh GR, Cordero SP, Rubin DL, Stuart JM. Institution: Biomedical Engineering, University of California, Santa Cruz, CA, USA. Background/Purpose: Patient stratification to identify subtypes with different disease manifestations, severity, and expected survival time is a critical task in cancer diagnosis and treatment. While stratification approaches using various biomarkers (including high-throughput gene expression measurements) for patient-to-patient comparisons have been successful in elucidating previously unseen subtypes, there remains an untapped potential of incorporating various genotypic and phenotypic data to discover novel or improved groupings. METHODS: Here, we present HOCUS, a unified analytical framework for patient stratification that uses a community detection technique to extract subtypes out of sparse patient measurements. HOCUS constructs a patient-to-patient network from similarities in the data and iteratively groups and reconstructs the network into higher order clusters. We investigate the merits of using higher-order correlations to cluster samples of cancer patients in terms of their associations with survival outcomes. RESULTS: In an initial test of the method, the approach identifies cancer subtypes in mutation data of glioblastoma, ovarian, breast, prostate, and bladder cancers. In several cases, HOCUS provides an improvement over using the molecular features directly to compare samples. Application of HOCUS to glioblastoma images reveals a size and location classification of tumors that improves over human expert-based stratification. CONCLUSIONS: Subtypes based on higher order features can reveal comparable or distinct groupings. The distinct solutions can provide biologically- and treatment-relevant solutions that are just as significant as solutions based on the original data. |
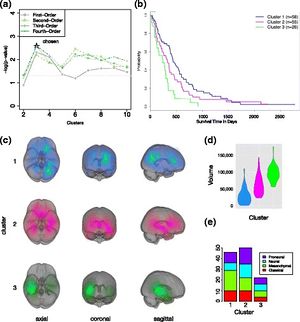 HOCUS of GBM MR Images. a. P-values of survival separation (log-rank test) for each of the orders of clustering across a range of k clusters. b. Kaplan-Meier plot of the third-order HOCUS clusters. c. Images of tumors within each cluster projected onto the MNI brain atlas. Showing sagittal, coronal, axial views. Brightness of color indicates the number of patients with tumor at a given location. Generated using 3D Slicer. d. Violin plot showing tumor volumes within each third-order cluster. e. Molecular (gene expression based) subtypes within the clusters. |
Three-Dimensional Volume Rendering of Pelvic Models and Paraurethral Masses Based on MRI Cross-Sectional Images
|
Publication: Int Urogynecol J. 2017 Mar 28. PMID: 28352953 Authors: Doumouchtsis SK, Nazarian DA, Gauthaman N, Durnea CM, Munneke G. Institution: Department of Obstetrics & Gynaecology, Epsom and St. Helier University Hospital NHS Trust, Epsom, UK. Background/Purpose: AIMS: Our aim was to assess the feasibility of rendering 3D pelvic models using magnetic resonance imaging (MRI) scans of patients with vaginal, urethral and paraurethral lesions and obtain additional information previously unavailable through 2D imaging modalities. METHODS: A purposive sample of five female patients 26-40 years old undergoing investigations for vaginal or paraurethral mass was obtained in a tertiary teaching hospital. 3D volume renderings of the bladder, urethra and paraurethral masses were constructed using 3D Slicer v.3.4.0. Spatial dimensions were determined and compared with findings from clinical, MRI, surgical and histopathological reports. The quality of information regarding size and location of paraurethral masses obtained from 3D models was compared with information from cross-sectional MRI and review of clinical, surgical and histopathological findings. RESULTS: The analysis of rendered 3D models yielded detailed anatomical dimensions and provided information that was in agreement and in higher detail than information based on clinical examination, cross-sectional 2D MRI analysis and histopathological reports. High-quality pelvic 3D models were rendered with the characteristics and resolution to allow identification and detailed viewing of the spatial relationship between anatomical structures. CONCLUSIONS: To our knowledge, this is the first preliminary study to evaluate the role of MRI-based 3D pelvic models for investigating paraurethral masses. This is a feasible technique and may prove a useful addition to conventional 2D MRI. Further prospective studies are required to evaluate this modality for investigating such lesions and planning appropriate management. |
A Study of Volumetric Variations of Basal Nuclei in the Normal Human Brain by Magnetic Resonance Imaging
|
Publication: Clin Anat. 2017 Mar;30(2):175-82. PMID: 28078760 Authors: Elkattan A, Mahdy A, Eltomey M, Ismail R. Institution: Department of Anatomy, Tanta University of Medical Sciences, Tanta, Egypt. Background/Purpose: Knowledge of the effects of healthy aging on brain structures is necessary to identify abnormal changes due to diseases. Many studies have demonstrated age-related volume changes in the brain using MRI. 60 healthy individuals who had normal MRI aged from 20 years to 80 years were examined and classified into three groups: Group I: 21 persons; nine males and 12 females aging between 20-39 years old. Group II: 22 persons; 11 males and 11 females aging between 40-59 years old. Group III: 17 persons; eight males and nine females aging between 60-80 years old. Volumetric analysis was done to evaluate the effect of age, gender and hemispheric difference in the caudate and putamen by the 3D Slicer 4.3.3.1 software using 3D T1-weighted images. Data were analyzed by student's unpaired t test, ANOVA and regression analysis. The volumes of the measured and corrected caudate nuclei and putamen significantly decreased with aging in males. There was a statistically insignificant relation between the age and the volume of the measured caudate nuclei and putamen in females but there was a statistically significant relation between the age and the corrected caudate nuclei and putamen. There was no significant difference on the caudate and putamen volumes between males and females. There was no significant difference between the right and left caudate nuclei volumes. There was a leftward asymmetry in the putamen volumes. The results can be considered as a base to track individual changes with time (aging and CNS diseases). |
MITK-OpenIGTLink for Combining Open-Source Toolkits in Real-Time Computer-Assisted Interventions
|
Publication: Int J Comput Assist Radiol Surg. 2017 Mar;12(3):351-61. PMID: 27687984 Authors: Klemm M, Kirchner T, Gröhl J, Cheray D, Nolden M, Seitel A, Hoppe H, Maier-Hein L, Franz AM. Institution: Laboratory for Computer-Assisted Medicine, Department of Electrical Engineering and Information Technology, Offenburg University, Offenburg, Germany. Background/Purpose: PURPOSE:
Due to rapid developments in the research areas of medical imaging, medical image processing and robotics, computer-assisted interventions (CAI) are becoming an integral part of modern patient care. From a software engineering point of view, these systems are highly complex and research can benefit greatly from reusing software components. This is supported by a number of open-source toolkits for medical imaging and CAI such as the medical imaging interaction toolkit (MITK), the public software library for ultrasound imaging research (PLUS) and 3D Slicer. An independent inter-toolkit communication such as the open image-guided therapy link (OpenIGTLink) can be used to combine the advantages of these toolkits and enable an easier realization of a clinical CAI workflow.
|
|
Publication: IEEE Trans Biomed Eng. 2017 Mar 2. PMID: 28362578 Authors: Jaeger HA, Nardelli P, O'Shea C, Tugwell J, Khan KA, Power T, O'Shea M, Kennedy MP, Cantillon-Murphy P. Institution: School of Engineering, University College Cork, Cork, Ireland. Background/Purpose: This paper describes a novel method of controlling an endoscopic catheter using an automated catheter tensioning system with the objective of providing clinicians with improved manipulation capabilities within the patient. Catheters are used in many clinical procedures to provide access to the cardiopulmonary system. Control of such catheters is performed manually by the clinicians using a handle, typically actuating a single or opposing set of pull-wires. Such catheters are generally actuated in a single plane, requiring the clinician to rotate the catheter handle to navigate the system. The automation system described here allows closed-loop control of a custom bronchial catheter in tandem with an electromagnetic tracking of the catheter tip and image guidance using 3D Slicer. An electromechanical drive train applies tension to four pull-wires to steer the catheter tip, with the applied force constantly monitored though force sensing load-cells. The applied tension is controlled through a PC connected joystick. An electromagnetic sensor embedded in the catheter tip enables constant real-time position tracking while a working channel provides a route for endoscopic instruments. The system is demonstrated and tested in both a breathing lung model and a preclinical animal study. Navigation to predefined targets in the subject's airways using the joystick while using virtual image guidance and electromagnetic tracking was demonstrated. Average targeting times were 24 seconds and 10 seconds respectively for the breathing lung and live animal studies. This paper presents the first reported remote controlled bronchial working channel catheter utilising electromagnetic tracking and has many implications for future development in endoscopic and catheter based procedures. |
Increased Cerebellar Gray Matter Volume in Head Chefs
|
Publication: PLoS One. 2017 Feb 9;12(2):e0171457. PMID: 28182712 | PDF Authors: Cerasa A, Sarica A, Martino I, Fabbricatore C, Tomaiuolo F, Rocca F, Caracciolo M, Quattrone A. Institution: Istituto di Bioimmagini e Fisiologia Molecolare, Consiglio Nazionale delle Ricerche, Catanzaro, Italy. Background/Purpose:OBJECTIVE:
Chefs exert expert motor and cognitive performances on a daily basis. Neuroimaging has clearly shown that that long-term skill learning (i.e., athletes, musicians, chess player or sommeliers) induces plastic changes in the brain thus enabling tasks to be performed faster and more accurately. How a chef's expertise is embodied in a specific neural network has never been investigated.
|
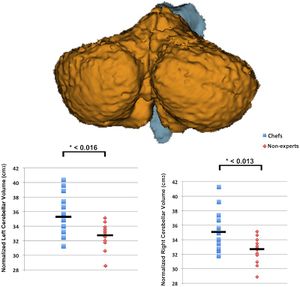 Sample color-coded automated brain segmentation results. A 3D surface image (created with 3D Slicer v 4.6, www.slicer.org) showing typical automated subcortical segmentation of the cerebellum performed by FreeSurfer (v 5.3). Scatter plot of the mean normalized volumes of the left and right cerebellar cortex for each single subject has been plotted. Advanced neuroimaging analysis reveals bilateral cerebellar volumetric increase in the chef group with respect to non-expert individuals. |
Tumor Heterogeneity Assessed by Texture Analysis on Contrast-Enhanced CT in Lung Adenocarcinoma: Association with Pathologic Grade
|
Publication: Oncotarget. 2017 Feb 16. PMID: 28430603 | PDF Authors: Liu Y, Liu S, Qu F, Li Q, Cheng R, Ye Z. Institution: Department of Radiology, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center of Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, China. Background/Purpose: To investigate whether texture features on contrast-enhanced computed tomography (CECT) images of lung adenocarcinoma have association with pathologic grade.Methods A cohort of 148 patients with surgically operated adenocarcinoma was retrospectively reviewed. Fifty-four CT features of the primary lung tumor were extracted from CECT images using open-source 3D Slicer software; meanwhile, enhancement homogeneity was evaluated by two radiologists using visual assessment. Multivariate logistic regression analysis was performed to determine significant image indicator of pathologic grade. Results Tumors of intermediate grade were more likely to be never smokers (P=0.020). Enhancement heterogeneity by visual assessment showed no statistical difference between intermediate grade and high grade (P=0.671). Among those 54 features, 29 of them were significantly associated with pathologic grade. Multivariate logistic regression analyses identified F33 (Homogeneity 1) (P=0.005) and F38 (Inverse Variance) (P=0.032) as unique independent image indicators of pathologic grade, and the AUC calculated from this model (AUC=0.834) was higher than clinical model (AUC=0.615) (P=0.0001).Conclusions Our study revealed that texture analysis on CECT images could be helpful in predicting pathologic grade of lung adenocarcinoma. |
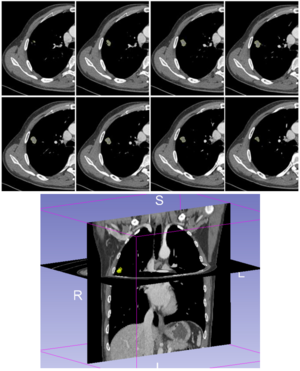 Example of CT images showing segmentation of lung tumor. Semiautomatic tumor segmentation was done on every slice of the tumor using 3D Slicer (a), and the 3D view of the segmented tumor (b) which was shown in yellow. |
Three-dimensional Printing of X-ray Computed Tomography Datasets with Multiple Materials using Open-source Data Processing
|
Publication: Anat Sci Educ. 2017 Feb 23. PMID: 28231405 Authors: Sander IM, McGoldrick MT, Helms MN, Betts A, van Avermaete A, Owers E, Doney E, Liepert T, Niebur G, Liepert D, Leevy WM. Institution: Department of Biological Sciences, College of Science, University of Notre Dame, Notre Dame, Indiana., USA. Background/Purpose: Advances in three-dimensional (3D) printing allow for digital files to be turned into a "printed" physical product. For example, complex anatomical models derived from clinical or pre-clinical X-ray computed tomography (CT) data of patients or research specimens can be constructed using various printable materials. Although 3D printing has the potential to advance learning, many academic programs have been slow to adopt its use in the classroom despite increased availability of the equipment and digital databases already established for educational use. Herein, a protocol is reported for the production of enlarged bone core and accurate representation of human sinus passages in a 3D printed format using entirely consumer-grade printers and a combination of free-software platforms. The comparative resolutions of three surface rendering programs were also determined using the sinuses, a human body, and a human wrist data files to compare the abilities of different software available for surface map generation of biomedical data. Data shows that 3D Slicer provided highest compatibility and surface resolution for anatomical 3D printing. Generated surface maps were then 3D printed via fused deposition modeling (FDM printing). In conclusion, a methodological approach that explains the production of anatomical models using entirely consumer-grade, fused deposition modeling machines, and a combination of free software platforms is presented in this report. The methods outlined will facilitate the incorporation of 3D printed anatomical models in the classroom. |
SEEG Assistant: A 3D Slicer Extension to Support Epilepsy Surgery
|
Publication: BMC Bioinformatics. 2017 Feb 23;18(1):124. PMID: 28231759 | PDF Authors: Narizzano M, Arnulfo G, Ricci S, Toselli B, Tisdall M, Canessa A, Fato MM, Cardinale F. Institution: Department of Informatics, Bioengineering Robotics and System engineering (DIBRIS), University of Genoa, Genova, Italy. Background/Purpose: In the evaluation of Stereo-Electroencephalography (SEEG) signals, the physicist's workflow involves several operations, including determining the position of individual electrode contacts in terms of both relationship to grey or white matter and location in specific brain regions. These operations are (i) generally carried out manually by experts with limited computer support, (ii) hugely time consuming, and (iii) often inaccurate, incomplete, and prone to errors.
|
 CPE out performs manual segmentation in complex and critical cases. a As an example of SEEG complexity, we show MRI and thresholded post-implant CT scans for one subject from our cohort. Contacts are shown as groups of white voxels. This case illustrates the complexity of SEEG implants with electrode shafts following non-planar directions (e.g. X), shafts targeting almost the same geometrical point (e.g. R and R’). b CPE segments all contacts (green spheres) belonging to each electrode from post-implant CT scans, represented here as red 3D meshes obtained tessellating the thresholded data to ease visualization. c Show the right pial surface with 3D post-implant thresholded-CT meshes and the cut plane used in panel d where the example of X and X’ electrodes are shown. Those examples represent the case of non-planar insertion trajectories which yielded an artefactually fused electrode. CPE integrating the knowledge of the electrode model can segment the contact positions more accurately than visual inspection. |
Associations of Radiomic Data Extracted from Static and Respiratory-Gated CT Scans with Disease Recurrence in Lung Cancer Patients Treated with SBRT
|
Publication: PLoS One. 2017 Jan 3;12(1):e0169172. PMID: 28046060| PDF Authors: Huynh E, Coroller TP, Narayan V, Agrawal V, Romano J, Franco I, Parmar C, Hou Y, Mak RH, Aerts HJ. Institution: Department of Radiation Oncology, Dana-Farber Cancer Institute, Brigham and Women's Hospital, Harvard Medical School, Boston, USA. Background/Purpose: Radiomics aims to quantitatively capture the complex tumor phenotype contained in medical images to associate them with clinical outcomes. This study investigates the impact of different types of computed tomography (CT) images on the prognostic performance of radiomic features for disease recurrence in early stage non-small cell lung cancer (NSCLC) patients treated with stereotactic body radiation therapy (SBRT). 112 early stage NSCLC patients treated with SBRT that had static free breathing (FB) and average intensity projection (AIP) images were analyzed. Nineteen radiomic features were selected from each image type (FB or AIP) for analysis based on stability and variance. The selected FB and AIP radiomic feature sets had 6 common radiomic features between both image types and 13 unique features. The prognostic performances of the features for distant metastasis (DM) and locoregional recurrence (LRR) were evaluated using the concordance index (CI) and compared with two conventional features (tumor volume and maximum diameter). P-values were corrected for multiple testing using the false discovery rate procedure. None of the FB radiomic features were associated with DM, however, seven AIP radiomic features, that described tumor shape and heterogeneity, were (CI range: 0.638-0.676). Conventional features from FB images were not associated with DM, however, AIP conventional features were (CI range: 0.643-0.658). Radiomic and conventional multivariate models were compared between FB and AIP images using cross validation. The differences between the models were assessed using a permutation test. AIP radiomic multivariate models (median CI = 0.667) outperformed all other models (median CI range: 0.601-0.630) in predicting DM. None of the imaging features were prognostic of LRR. Therefore, image type impacts the performance of radiomic models in their association with disease recurrence. AIP images contained more information than FB images that were associated with disease recurrence in early stage NSCLC patients treated with SBRT, which suggests that AIP images may potentially be more optimal for the development of an imaging biomarker. Funding:
|
 A) Examples of free breathing (FB) and average intensity projection (AIP) images, demonstrating the observable differences in tumor phenotype between each image type. AIP images were reconstructed from 4D computed tomography (CT) scans. B) Schematic representation of the radiomics workflow for FB and AIP images. I. CT images of the patient are acquired and the tumor is segmented. II. Imaging features (radiomic and conventional features) are extracted from the tumor volume. III. Radiomic features undergo a feature dimension reduction process to generate a low-dimensional feature set based on feature stability and variance. IV. Imaging features are then analyzed with clinical outcomes to evaluate their prognostic power. FB and AIP radiomics features are compared. A set of 644 radiomic features was extracted from tumor volumes isolated from FB or AIP images (Fig 1B) using an in-house Matlab 2013 toolbox and 3D Slicer 4.4.0 software |
Early Experiences of Planning Stereotactic Radiosurgery using 3D Printed Models of Eyes with Uveal Melanomas
|
Publication: Clin Ophthalmol. 2017 Jan 31;11:267-71. PMID: 28203052 | PDF Authors: Furdová A, Sramka M, Thurzo A, Furdová A. Institution: Department of Ophthalmology, Faculty of Medicine, Comenius University, Bratislava, Slovakia. Background/Purpose: OBJECTIVE:
The objective of this study was to determine the use of 3D printed model of an eye with intraocular tumor for linear accelerator-based stereotactic radiosurgery.
|
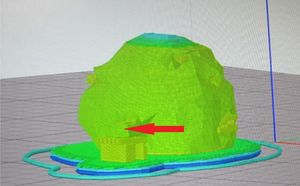 A) Virtual model of the eye, outer view; arrow indicates optic nerve. A virtual 3D model of eye globe with tumor based on tissue density was created from CT and MRI data by using the 3D Slicer software for segmentation. |
Intra-rater Variability in Low-grade Glioma Segmentation
|
Publication: J Neurooncol. 2017 Jan;131(2):393-402. PMID: 27837437 Authors: Bø HK, Solheim O, Jakola AS, Kvistad KA, Reinertsen I, Berntsen EM. Institution: Department of Radiology and Nuclear Medicine, St. Olavs University Hospital, Trondheim, Norway. Background/Purpose: Assessment of size and growth are key radiological factors in low-grade gliomas (LGGs), both for prognostication and treatment evaluation, but the reliability of LGG-segmentation is scarcely studied. With a diffuse and invasive growth pattern, usually without contrast enhancement, these tumors can be difficult to delineate. The aim of this study was to investigate the intra-observer variability in LGG-segmentation for a radiologist without prior segmentation experience. Pre-operative 3D FLAIR images of 23 LGGs were segmented three times in the software 3D Slicer. Tumor volumes were calculated, together with the absolute and relative difference between the segmentations. To quantify the intra-rater variability, we used the Jaccard coefficient comparing both two (J2) and three (J3) segmentations as well as the Hausdorff Distance (HD). The variability measured with J2 improved significantly between the two last segmentations compared to the two first, going from 0.87 to 0.90 (p = 0.04). Between the last two segmentations, larger tumors showed a tendency towards smaller relative volume difference (p = 0.07), while tumors with well-defined borders had significantly less variability measured with both J2 (p = 0.04) and HD (p < 0.01). We found no significant relationship between variability and histological sub-types or Apparent Diffusion Coefficients (ADC). We found that the intra-rater variability can be considerable in serial LGG-segmentation, but the variability seems to decrease with experience and higher grade of border conspicuity. Our findings highlight that some criteria defining tumor borders and progression in 3D volumetric segmentation is needed, if moving from 2D to 3D assessment of size and growth of LGGs. |
Hybrid Positron Emission Tomography Segmentation of Heterogeneous Lung Tumors using 3D Slicer: Improved Growcut Algorithm with Threshold Initialization
|
Publication: J. Med. Imag. 2017 Jan-Mar;4(1), 011009. PMID: 28149920 | PDF Authors: Thomas HM, Devakumar D, Sasidharan B, Bowen SR, Heck DK, Jebaseelan J, Samuel E. Institution: VIT University, School of Advanced Sciences, Department of Physics, Vellore, Tamil Nadu 632004, India. Background/Purpose: This paper presents an improved GrowCut (IGC), a positron emission tomography-based segmentation algorithm, and tests its clinical applicability. Contrary to the traditional method that requires the user to provide the initial seeds, the IGC algorithm starts with a threshold-based estimate of the tumor and a three- dimensional morphologically grown shell around the tumor as the foreground and background seeds, respectively. The repeatability of IGC from the same observer at multiple time points was compared with the traditional GrowCut algorithm. The algorithm was tested in 11 nonsmall cell lung cancer lesions and validated against the clinician-defined manual contour and compared against the clinically used 25% of the maximum standardized uptake value [SUV-(max)], 40% SUVmax, and adaptive threshold methods. The time to edit IGC-defined functional volume to arrive at the gross tumor volume (GTV) was compared with that of manual contouring. The repeatability of the IGC algorithm was very high compared with the traditional GrowCut (p = 0.003) and demonstrated higher agreement with the manual contour with respect to threshold-based methods. Compared with manual contouring, editing the IGC achieved the GTV in significantly less time (p = 0.11). The IGC algorithm offers a highly repeatable functional volume and serves as an effective initial guess that can well minimize the time spent on labor-intensive manual contouring. |
 A) A representative example of the uncertainty volume observed with the 3D Slicer GrowCutmethod. (a) The lesion was delineated in three separate runs. There was variability with each run and the composite error in the variability calculated as the uncertainty volume is highlighted in green in (b). |
Pre-clinical Validation of Virtual Bronchoscopy using 3D Slicer
|
Publication: Int J Comput Assist Radiol Surg. 2017 Jan;12(1):25-38. PMID: 27325238 Authors: Nardelli P, Jaeger A, O'Shea C, Khan KA, Kennedy MP, Cantillon-Murphy P. Institution: School of Engineering, University College Cork, College Road, Cork, Ireland. Background/Purpose: Lung cancer still represents the leading cause of cancer-related death, and the long-term survival rate remains low. Computed tomography (CT) is currently the most common imaging modality for lung diseases recognition. The purpose of this work was to develop a simple and easily accessible virtual bronchoscopy system to be coupled with a customized electromagnetic (EM) tracking system for navigation in the lung and which requires as little user interaction as possible, while maintaining high usability. Methods: The proposed method has been implemented as an extension to the open-source platform, 3D Slicer. It creates a virtual reconstruction of the airways starting from CT images for virtual navigation. It provides tools for pre-procedural planning and virtual navigation, and it has been optimized for use in combination with a [Formula: see text] of freedom EM tracking sensor. Performance of the algorithm has been evaluated in ex vivo and in vivo testing. Results: During ex vivo testing, nine volunteer physicians tested the implemented algorithm to navigate three separate targets placed inside a breathing pig lung model. In general, the system proved easy to use and accurate in replicating the clinical setting and seemed to help choose the correct path without any previous experience or image analysis. Two separate animal studies confirmed technical feasibility and usability of the system. Conclusions: This work describes an easily accessible virtual bronchoscopy system for navigation in the lung. The system provides the user with a complete set of tools that facilitate navigation towards user-selected regions of interest. Results from ex vivo and in vivo studies showed that the system opens the way for potential future work with virtual navigation for safe and reliable airway disease diagnosis. |
Anatomical Study and Locating Nasolacrimal Duct on Computed Topographic Image
|
Publication: J Craniofac Surg. 2017 Jan;28(1):275-9. PMID: 27977487 Authors: Zhang S, Cheng Y, Xie J, Wang Z, Zhang F, Chen L, Feng Y, Wang G. Institution: Department of Endocrinology, First Hospital of Jilin University, Changchun, China. Background/Purpose: We performed a novel anatomical and radiological investigation to understand the structure of nasolacrimal duct (NLD) and to provide data to help surgeons locate the openings of NLD efficiently based on landmarks. MATERIALS AND METHODS: We examined the NLD region using computed tomography images of 133 individuals and 6 dry skull specimens. Multiplanar reconstruction of the computed tomography images was performed, and the anatomical features of the NLD were studied in the coronal, sagittal, and axial planes. The long and short diameters of NLD were measured along its cross-section. The position of NLD was localized using the nostril, concha nasalis media, and medial orbital corner as landmarks. The free and open source software, 3D Slicer, was used for the segmentation of the NLD and 3D visualization of the superior and inferior openings of the NLD. RESULTS: The length, angle, and diameter of NLD were significantly influenced by the age in females compared to those in males. The inferior opening of the NLD could be located efficiently using the nostril and the midsagittal line while the superior opening of NLD could be located using the medial orbital corner. Third, 3D Slicer enabled us to measure the distance between the skin and the bony structure in the image. CONCLUSION: Our study indicates that the sex and age of the patient should be considered while selecting the optimal NLD stent for a patient, and that the precise location of NLD in reference to landmarks can simplify the surgical difficulties and reduce the risk of injury during the transnasal operation. |
Intra-rater Variability in Low-grade Glioma Segmentation
|
Publication: J Neurooncol. 2017 Jan;131(2):393-402. PMID: 27837437 Authors: Bø HK, Solheim O, Jakola AS, Kvistad KA, Reinertsen I, Berntsen EM. Institution: Department of Radiology and Nuclear Medicine, St. Olavs University Hospital, Trondheim, Norway Background/Purpose: Assessment of size and growth are key radiological factors in low-grade gliomas (LGGs), both for prognostication and treatment evaluation, but the reliability of LGG-segmentation is scarcely studied. With a diffuse and invasive growth pattern, usually without contrast enhancement, these tumors can be difficult to delineate. The aim of this study was to investigate the intra-observer variability in LGG-segmentation for a radiologist without prior segmentation experience. Pre-operative 3D FLAIR images of 23 LGGs were segmented three times in the software 3D Slicer. Tumor volumes were calculated, together with the absolute and relative difference between the segmentations. To quantify the intra-rater variability, we used the Jaccard coefficient comparing both two (J2) and three (J3) segmentations as well as the Hausdorff Distance (HD). The variability measured with J2 improved significantly between the two last segmentations compared to the two first, going from 0.87 to 0.90 (p = 0.04). Between the last two segmentations, larger tumors showed a tendency towards smaller relative volume difference (p = 0.07), while tumors with well-defined borders had significantly less variability measured with both J2 (p = 0.04) and HD (p < 0.01). We found no significant relationship between variability and histological sub-types or Apparent Diffusion Coefficients (ADC). We found that the intra-rater variability can be considerable in serial LGG-segmentation, but the variability seems to decrease with experience and higher grade of border conspicuity. Our findings highlight that some criteria defining tumor borders and progression in 3D volumetric segmentation is needed, if moving from 2D to 3D assessment of size and growth of LGGs. |
Open Wedge High Tibial Osteotomy using Three-Dimensional Printed Models: Experimental Analysis using Porcine Bone
|
Publication: Knee. 2017 Jan;24(1):16-22. PMID: 27876267 Authors: Kwun JD, Kim HJ, Park J, Park IH, Kyung HS. Institution: Department of Orthopaedic Surgery, School of Medicine, Kyungpook National University, Daegu, Republic of Korea. Background/Purpose: BACKGROUND: The purpose of this study was to evaluate the usefulness of three-dimensional (3D) printed models for open wedge high tibial osteotomy (HTO) in porcine bone. METHODS: Computed tomography (CT) images were obtained from 10 porcine knees and 3D imaging was planned using the 3D Slicer program. The osteotomy line was drawn from the three centimeters below the medial tibial plateau to the proximal end of the fibular head. Then the osteotomy gap was opened until the mechanical axis line was 62.5% from the medial border along the width of the tibial plateau, maintaining the posterior tibial slope angle. The wedge-shaped 3D-printed model was designed with the measured angle and osteotomy section and was produced by the 3D printer. The open wedge HTO surgery was reproduced in porcine bone using the 3D-printed model and the osteotomy site was fixed with a plate. Accuracy of osteotomy and posterior tibial slope was evaluated after the osteotomy. RESULTS: The mean mechanical axis line on the tibial plateau was 61.8±1.5% from the medial tibia. There was no statistically significant difference (P=0.160). The planned and post-osteotomy correction wedge angles were 11.5±3.2° and 11.4±3.3°, and the posterior tibial slope angle was 11.2±2.2° pre-osteotomy and 11.4±2.5° post-osteotomy. There were no significant differences (P=0.854 and P=0.429, respectively). CONCLUSION: This study showed that good results could be obtained in high tibial osteotomy by using 3D printed models of porcine legs. |
MRI Visible Fe3O4 Polypropylene Mesh: 3D Reconstruction of Spatial Relation to Bony Pelvis and Neurovascular Structures
|
Publication: Int Urogynecol J. 2017 Jan 25. PMID: 28124074 Authors: Chen L, Lenz F, Alt CD, Sohn C, De Lancey JO, Brocker KA. Institution: Pelvic Floor Research Group, Biomedical Engineering Department, University of Michigan, Ann Arbor, MI, USA. Background/Purpose:
INTRODUCTION AND HYPOTHESIS:
To demonstrate mesh magnetic resonance imaging (MRI) visibility in living women, the feasibility of reconstructing the full mesh course in 3D, and to document its spatial relationship to pelvic anatomical structures.
|
Go to 2016:: 2015 :: 2014-2011 :: 2010-2005
